* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Biochemistry - Elon University
Cell culture wikipedia , lookup
Biochemistry wikipedia , lookup
Gene regulatory network wikipedia , lookup
Protein moonlighting wikipedia , lookup
Protein adsorption wikipedia , lookup
Western blot wikipedia , lookup
Intrinsically disordered proteins wikipedia , lookup
Protein–protein interaction wikipedia , lookup
Two-hybrid screening wikipedia , lookup
Cell-penetrating peptide wikipedia , lookup
Endomembrane system wikipedia , lookup
Biochemical cascade wikipedia , lookup
Paracrine signalling wikipedia , lookup
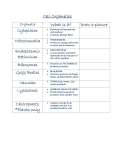
BCL-2 protein regulation of apoptosis in diabetic cardiomyopathy December 7, 2011 Abstract A complication of diabetes that affects heart function, known as diabetic cardiomyopathy (DCM), contributes to the mortality of over 80% of the diabetic population. Despite scientific advances made in the treatment and prevention of cardiovascular disease, the improvement in life expectancy that has been achieved in the non-diabetic population has not been mirrored in the diabetic population. Since current cardiovascular treatments are similar for diabetics and non-diabetics, there is a need to elucidate mechanisms of DCM’s progression in order to develop new therapeutic treatments. High blood sugar (hyperglycemia) has been identified as a major contributor to DCM’s development. Previous studies have identified the BCL-2 family, a group of similar proteins involved in the regulation of cell death (apoptosis), as being involved in hyperglycemia-induced heart cell damage. Apoptosis is not an inherently bad process; it is an efficient way to remove damaged or unneeded cells. However, when cells die when they should not, as in DCM, it can lead to major complications. Although BCL-2 proteins have been shown to be involved in hyperglycemia-induced apoptosis, the precise mechanisms of BCL2’s involvement remain unclear. This study will assess changes to apoptotic proteins, as well as structural alterations to mitochondria (the cellular functional units involved in apoptosis where BCL-2 proteins interact) that are induced by hyperglycemia. We will look at living heart cells to see how the proteins that control the normal cell death process are affected when exposed to high glucose levels. Introduction of Field The field of research pertaining to the biochemical basis of diabetic cardiomyopathy is an important field that aims to elucidate potential therapeutic targets for diabetes-associated heart failure. Diabetic cardiomyopathy (DCM) is a complication of both type I and type II diabetes, which are projected to affect 300 million people worldwide by 2025.1,2 Diabetes is therefore very common and is a serious global health concern of the 21st century. Because cardiovascular complications of diabetes are responsible for 80% of diabetic mortality, DCM is a condition associated with diabetes to which much attention needs to be paid.2 It is necessary to understand basic mechanisms and conditions associated with diabetes to properly understand DCM. Diabetes is a metabolic disorder in which patients affected are not able to use the food they eat to properly produce energy for cellular processes. Healthy individuals consume food, which their bodies are able to break down into a type of sugar called glucose. Glucose is the primary source that the body uses to make energy. Once glucose is in the bloodstream, it has to be recruited and helped to enter the cells that are able to convert glucose into cellular energy. A hormone called insulin, which is secreted by the pancreas, is responsible for helping glucose enter cells so that it can be metabolized, or converted to energy. Patients with type I diabetes have an autoimmune response that attacks the cells that produce insulin. This means that the body’s own immune system fights the cells that it needs to produce its insulin. As a result, people with type I diabetes must take insulin in order to be able to metabolize glucose. People with type II diabetes initially produce enough insulin on their own, but their bodies are resistant to insulin. Due to this insulin resistance, eventually natural production of insulin decreases since produced insulin is not being used. In both cases, the result is that glucose builds up in the bloodstream because it is unable to be used by cells.3 Diabetes causes a variety of problems as a result of cells not being able to metabolize the glucose needed to carry out cellular processes. One of these problems is DCM.1 DCM was first proposed in 1972 after four patients were observed to experience congestive heart failure (CHF) without any of the typical causes.4 CHF is characterized by the heart’s inability to pump the needed amount of blood to a patient’s body (called systolic heart failure) or a stiffness of muscular tissue resulting in the inability of the heart to fill with blood easily or completely (called diastolic heart failure).5 Prior to the observation of these patients, CHF had always been observed accompanied by one or more risk factors. These include factors such as coronary artery disease (clogging of arteries by sticky fats and plaques), congenital heart disease (abnormal heart development from birth), hypertension (high blood pressure), and smoking or alcoholism.4 Because there were patients exhibiting CHF without any signs of these factors, it was proposed that there was a cardiomyopathy, or a heart disease, specific to diabetic patients.6 Because of the absence of the typical risk factors, it was also proposed that this cardiomyopathy develops by a unique mechanism.4 Understanding the basic mechanisms of how the heart functions is important to understanding how CHF affects patients. The human heart is comprised of four main chambers: two atria and two ventricles.7 (See Figure I) Oxygen-deficient blood is pumped into the heart through the right atrium. The right atrium pumps blood to the right ventricle, which in turn pumps blood to the lungs so that it can be oxygenated. The oxygenated blood is pumped into the left atrium, and subsequently is pumped into the left ventricle (LV). The LV is very important because it pumps freshly oxygenated blood to the rest of the body.8 Patients with DCM typically have several structural and functional ventricular abnormalities. The LV is particularly affected in DCM, as patients with DCM often exhibit LV hypertrophy and fibrosis. LV hypertrophy is characterized by an increase in LV mass, and is closely linked to fibrosis, which is an increase in the connective tissue of the heart. LV hypertrophy and fibrosis lead to LV dysfunction.4 LV dysfunction can be manifested in many different ways. One way that LV dysfunction in DCM patients is seen is by the observation of decreased ejection fraction.4 The ejection fraction refers to the Figure I: Diagram of the human heart.7 amount of oxygenated blood that is expelled from the heart through the left ventricle as compared to the amount of deoxygenated blood that enters the heart.9 Essentially, DCM causes changes to the LV (in particular) that result in improper heart function and ultimately lead to CHF.4 Because of the vast number of people affected by diabetes and DCM, it is important to understand this condition in more detail. Currently, the biochemical basis of DCM is incompletely understood.10 Understanding the biochemical basis of diseases is very important, because it allows treatments to be developed that target specific biochemical pathways involved in the development of those diseases. Literature indicates that the current treatments for DCM are the same as for other types of CHF.4 Since DCM develops through a different pathway, it is not ideal to be treating it in the same way that normal CHF is treated. This is reflected by the fact that improvements that have been made in the survival of non-diabetic patients have not been mirrored in the diabetic population.2 One study indicated that while a 36.4% decrease in cardiovascular mortality has been observed in non-diabetic men, only a 13.1% decrease has been seen in diabetic men. More strikingly, while a 17% decrease in the mortality of non-diabetic women has been achieved, an increase of 23% has been observed in diabetic women.11 Similarly, it has been shown that patients with diabetes (both type I and type II) are two to four times more likely to experience complications such as coronary artery disease or stroke.12 Because biochemical studies have led to improved treatments for other diseases, there is the potential for similar advancements in DCM. Elucidating the biochemical mechanisms and pathways involved in DCM is very important in order to develop treatments that may lead to the decreased cardiovascular mortality of the diabetic population. The main risk factors associated with diabetes that have been identified as important to DCM’s biochemical basis include hyperglycemia, hyperinsulinemia, and dyslipedimia.1 Hyperglycemia refers to an increase in blood glucose content, such as the increase seen in patients with both types of diabetes. When a patient with type II diabetes still produces insulin but is simply resistant to it, his or her inability to use insulin can lead to hyperinsulinemia, or an increase in the concentration of insulin in the blood. Dyslipidemia is characterized by abnormal concentrations of lipids in the blood. Lipids are biomolecules that have many purposes and effects. Cholesterol is a specific type of lipid that is involved in the development of heart disease. Too much cholesterol can lead to the development of plaques in arteries. Dyslipidemia skews the balance of lipids in the body, which can have drastic effects on the heart.1 Although these risk factors have been identified, not all of the biochemical pathways that are affected by them are understood. Researchers in the field examining the biochemical basis of DCM look at how cellular structures and processes are affected by the different risk factors associated with diabetes. Changes to organelles (functional units in cells) as well as to cellular processes (such as metabolism, etc.) are being determined biochemically so that the development of and basis for DCM can be properly elucidated.10 Much of the research done in this field is first done in cell culture models. Cell cultures allow researchers in this field to look at how cells are affected by a factor of interest in an environment that is much more easily controlled than an entire organism. Cultured cells are cells that have been isolated from an organism, and have been modified so that they can be grown outside of the organism. Once the effect of a particular factor of interest on single cells has been determined, this information can be used to conduct experiments in animal models, and later in clinical trials involving humans. A large majority of research in the field right now uses cell culture and animal models because DCM is a relatively new condition. Understanding more about the pathways involved in the development of DCM will be very important if a decrease in cardiovascular mortality of diabetic patients is to be achieved. The field researching the biochemical basis of DCM is very important to this goal. Build to Question One of the known events in the pathogenesis of DCM is tissue damage due to a loss of cardiomyocytes, or heart cells. Understanding how and why cardiomyocytes die at an increased rate in diabetic patients is one of the important questions in the field that needs to be answered. By elucidating the pathway of this aspect of DCM’s development, new molecular targets for therapeutic treatments could be identified. Since cardiomyocytes die at an increased rate in DCM, it is important to first determine the pathway through which cardiomyocytes are dying. There are two major types of cell death that could be responsible for this tissue damage: necrosis and apoptosis. Necrosis is typically referred to as accidental or non-programmed cell death.13 It is generally detrimental; that is, necrosis is not a normal biological process that occurs in healthy organisms. It is a direct response to physical external stressors, such as an increase in concentrations of chemicals that can damage cells. Necrosis is called non-programmed death because there is not a complex cell-signaling pathway that is followed before death occurs.13 Whatever is antagonizing the cell physically kills it, and the cell itself does not regulate this process. In contrast, apoptosis is a form of programmed cell death that occurs in a very specific manner and is regulated by a number of different proteins and factors at the cellular level. It is sometimes called “cellular suicide” because it is a process through which the cell actually dismantles itself after a cascade of intracellular signals.13 (See Figure II) It is a normal aspect of both embryogenesis and homeostasis, and should not be considered to be inherently detrimental. For example, in human embryogenesis, or the development of a human embryo, apoptosis is the process through which initially webbed hands are transformed into hands with separated fingers. In human homeostasis, apoptosis is the process through which the body gets rid of unneeded or unhealthy cells. Apoptosis is therefore a very beneficial cellular process; there is only a problem when there is a dysregulation of apoptosis. In cancer cells, cells that should undergo apoptosis do not, which leads to massive cellular replication and eventually tumors. This is an example of apoptosis failing to occur when the body needs it in order to maintain homeostasis. The opposite problem, apoptosis occurring when it should not, is seen in many diseases such as sepsis, AIDS, and several neurodegenerative diseases.15 Figure II: Cellular death through apoptosis and Kuethe, et al. (2007) showed that necrosis. In necrosis, the cell membrane is ruptured diabetic patients with cardiomyopathy had and the cell dies in a disorganized fashion. In significantly more apoptotic cardiomyocytes apoptosis, the cell dismantles itself through a than non-diabetics with similar complex signaling pathway.14 cardiomyopathy.16 This was accomplished through the analysis of periodic biopsies from patients with and without diabetes. Therefore, it is thought that apoptotic cell death is the major contributing factor to the cardiac tissue damage associated with the pathogenesis of DCM. Understanding why an increased frequency of apoptosis occurs in DCM is an important step towards a better understanding of the molecular pathways involved in DCM’s progression. Cai et al. (2002) investigated the link between hyperglycemia, which is one of the diabetic risk factors thought to be associated with DCM’s pathogenesis, and cardiomyocyte apoptosis.17 This study confirmed increased apoptosis through a specific pathway of apoptosis (called the mitochondrial cytochrome-c mediated caspase-3 activation pathway) to be a direct result of hyperglycemia. In this pathway, the ultimate commitment to cellular death is when the outer membranes of the mitochondria (see Figure III) are permeated in a process called mitochondrial outer membrane permeabilization, or MOMP.13 When MOMP occurs, chemicals and proteins that are normally Figure III: Diagram of the mitochondria. in the intermembrane space are released into the cell, and those Mitochondria are membrane-bound chemicals/proteins cause a cascade of events that leads to cell organelles within cells and are responsible for energy production as well as are involved in regulation of apoptosis.18 death. One of the released proteins is cytochrome-c, which is able to activate a specific protein called caspase-3. Caspases are proteins that, when activated, can cleave other proteins. When caspases are activated in a cell, they cleave important proteins and effectively dismantle the cell. Cai et al. (2002) induced diabetes in mice, and looked at changes in apoptosis in the mouse hearts.17 They simultaneously grew H9c2 cells (a mouse heart cell line) in varying glucose conditions. Cai et al. used standard biochemical techniques to determine that cell viability was decreased, apoptosis was occurring, and cytochrome-c and caspase-3 were involved in both the mouse and cell models. The results from this study confirmed that hyperglycemia increases the incidence of apoptosis in heart cells, specifically through the mitochondrial cytochrome-c-mediated caspase-3 activation pathway. Although this study indicated the apoptotic pathway that is activated in hyperglycemic cardiomyocyte apoptosis, it did not indicate precisely how that pathway was activated by hyperglycemia. Identifying the proteins involved in the pathway of activation is an important next step. Other studies have shown changes, as a result of hyperglycemia, to proteins called BCL-2 proteins. Apoptosis is controlled by the interaction of several different proteins, including the BCL-2 family of proteins. A family of proteins is simply a group of proteins that are structurally and functionally similar. BCL-2 family proteins are all small, globular proteins that contain anywhere from one to four regions of BCL-2 sequence homology (BH) domains.19 This means that there are four regions of BCL-2 proteins that are very similar between different types of BCL-2 proteins. (See Figure IV) Within the BCL-2 family, there are two broad categories of proteins. Anti-apoptotic proteins, containing all four BH domains, protect cells from apoptosis by discouraging MOMP. Pro-apoptotic proteins, which can contain either BH domains 1-3 or only the BH3 domain, work together to promote Figure IV: BCL-2 family proteins contain anywhere apoptosis by causing MOMP. There are from 1-4 BCL-2 homology (BH) domains.20 certain proteins that can directly cause MOMP, and other proteins that encourage MOMP without directly causing it. This division of the BCL-2 family is further described in Table I. Anti-apoptotic proteins (BH1-4) Pro-apoptotic (BH1-4 and BH3-only) Proteins that protect from MOMP: •Include BCL-2, MCL-1, BCL-XL, BCL-W Proteins that directly cause MOMP (BH1-3): •BAX and BAK •Promote cell death Activators (BH3-only): •Activate BAX/BAK •Include BIM, BID Sensitizers (BH3-only): •Help activators be able to do their job •Include BAD, NOXA, PUMA Table I: Classification and description of BCL-2 family proteins. One of the dominant proposed models of BCL-2 regulation of apoptosis (see Figure V) indicates that anti-apoptotic BCL-2 family proteins (such as BCL-2) are embedded in the mitochondrial outer membrane and preferentially bind activator BH3-only proteins (such as BIM). When a cell receives a signal to die, an upregulation or translocation of BH3-only sensitizers (such as BAD) results in competitive binding to anti-apoptotic BCL-2 proteins, thereby releasing activators to be free to activate BAX and BAK. When BAX and BAK are activated, they are thought to oligomerize (or bind to each other), creating pores in the outer mitochondrial membrane (and thereby causing MOMP).19 A delicate balance and specific interactions between BCL-2 proteins protects cells from undergoing the mitochondrial cytochrome-cmediated caspase-3 activation pathway of apoptosis.22 When a cell receives a signal that it needs to die, the balance of and interaction between BCL-2 family members changes. In normal processes, there will be slight variations in protein concentration and location within cells, which results in the standard levels of apoptosis needed to maintain normal organism function. However, if the balance between pro- and anti-apoptotic proteins is severely shifted, it is possible that cells will die when it is unnecessary or will live when they are not needed. Therefore, it is very important for the balance of and interactions between BCL-2 family Figure V: One of the proposed models for BCL-2 members to be maintained. If it is not, apoptosis will protein regulation of apoptosis [adapted from either occur too frequently or not frequently (21)]. enough.22 Hasnan et al. (2010) showed an increase of BAX in the cells of diabetic patients.23 In this study, researchers collected skin biopsy samples from diabetic human patients and assessed them for proapoptotic markers, such as BCL-2 proteins, that promote apoptosis. The significant increase in BAX seen in this study matched BAX upregulations seen in other studies using kidneys of diabetic animals as well as human diabetic retinas with high levels of glucose. Although this indicates that perhaps BAX is one of the more important proteins involved in hyperglycemia-induced apoptosis, it does not give information as to how hyperglycemia increases the level of this protein, nor does it necessarily indicate the apoptotic mechanisms in heart cells. These studies do, however, confirm that BCL-2 proteins are relevant to the increase of apoptosis due to hyperglycemia. Since cardiomyocyte loss has been shown to be important in the progression of DCM, and because the mitochondrial pathway of apoptosis has been indicated to be relevant, understanding how the BCL-2 family is involved in hyperglycemia induced apoptosis could potentially yield new therapeutic targets for diabetic patients. Although the BCL-2 family members have been identified as major players in hyperglycemia-induced tissue damage, the precise mechanisms and interactions that govern their participation have still not been elucidated.24 In order to develop more effective therapeutic treatments and preventative measures for diabetic patients, it is necessary to understand the precise mechanisms involved. This study will ask How does hyperglycemia affect BCL-2 proteins and their interactions to promote apoptosis in cardiomyocytes? It will employ a cell culture model in which apoptosis due to different concentrations of glucose will be studied. One of the major goals will be to establish exactly which BCL-2 activators and sensitizers might be important in promoting cell death, and how hyperglycemia causes changes to those proteins. This model of diabetic cardiomyopathy will therefore provide more information on how hyperglycemia causes tissue damage. Understanding which BCL-2 proteins are important, and how they and their interactions are changed in hyperglycemic conditions, will help in the overall understanding of how DCM develops. References 1 Battiprolu, P.K., Gillette, T.G., Wang, Z.V., Lavandero, S., Hill, J.A. Diabetic cardiomyopathy: mechanisms and therapeutic targets. Drug Discov Today Dis Mech. 2010; 7(2):135-143. 2 C. Voulgari, D. Papadogiannis, N. Tenolouris. Diabetic cardiomyopathy: from the pathophysiology of the cardiac myocytes to current diagnosis and management strategies. Vascular Health and Risk Management. 2010; 6:883-903. 3 National Diabetes Information Clearinghouse. Diabetes Overview. http://diabetes.niddk.nih.gov/dm/pubs/overview/index.aspx (accessed October 13, 2011) 4 Spector, K.S. Diabetic Cardiomyopathy. Clin Cardiol. 1998; 21(12):885-887. This article gives an overview of the discovery and history of diabetic cardiomyopathy. It describes the clinical manifestations, as well as gives epidemiological data on the incidence of heart disease in diabetics. It contains information that helps to explain why understanding DCM is so important, because it stresses the unique risks diabetics face in terms of developing congestive heart failure. It begins to discuss some potential biochemical causes of DCM, though it does not conclusively identifying the main pathways. This paper is instrumental to my research, since it has provided me with much of the physiological information upon which my project is based. 5 PubMed Health. Heart Failure. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001211/ (accessed September 20, 2011) 6 Rubler, S., Dlugash, J., Yuceoglu, Y.Z., Kumrad, T., Brandwood, A.W.,Grishman, A. New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol. 1972; 30:595-602. 7 The Patient’s Guide to Heart Valve Surgery. Heart. http://www.heart-valvesurgery.com/Images/Human-Heart-Diagram-Picture.gif (accessed September 27, 2011) 8 Howard Hughes Medical Institute. Anatomy and physiology of the heart. http://www.hhmi.org/biointeractive/vlabs/cardiology/content/cg/basic.html (accessed October 13, 2011) 9 Mayo Clinic. Ejection Fraction. http://www.mayoclinic.com/health/ejection-fraction/AN00360 10 Boudina, S., Abel, E.D. Diabetic cardiomyopathy, causes and effects. Rev Endocr Metab Disord. 2010; 11(1):31-39. 11 Barrett-Conner, E., Wingard, D.L., Sex differences in ischemic heart disease mortality in diabetics: a prospective polulation based study. Am J Epidemiol. 1983; 118:489-496. 12 Zimmet, P., Alberti, K.G. M.M., Swan, J. Global and social implications of the diabetes epidemic. Nature. 2001; 414:782-787. 13 Hotchkiss, R.S., Strasser, A., McDunn, J.E., Swanson, P.E. Cell Death. N Engl J Med. 2009; 361:1570-1583. 14 University of Alcaca De Henares. Characteristics of apoptosis. http://www2.uah.es/daviddiaz/Apoptosis/Imagenes/ApopNecrot.jpg (accessed November 10, 2011). 15 Ramirez Chamond, R., Anon, J.C., Aguilar, M., Pasadas, F.G. Apoptosis and Disease. Alergol Inmunol Clin. 1999; 14(6):367-374. 16 Kuethe, F., Sigusch, H.H., Bornstein, S.R., Hilbig, K., Kamvisi, V., Figulla, H.R. Apoptosis in patients with dilated cariomyopathy and diabetes: a feature of diabetic cardiomyopathy? Horm Metab Res. 2007; 39:672-676. 17 Cai, L., Wei, L., Wang, G., Guo, L., Jiang, Y., Kang, Y.J. Hyperglycemia-Induced Apoptosis in Mouse Myocardium. Diabetes. 2002; 51:1938-1948. This research article is incredibly important to my project, as it confirms the increased incidence of apoptosis as a result of hyperglycemia in two different models: a cell culture and an animal model. Many of the assays used to determine cell viability and apoptosis may be utilized in my project. The hyperglycemia model will also be helpful in terms of providing me an example to replicate/modify. It is a key paper in the development of my project, as it clearly identifies an increase in cell death as a result of hyperglycemia, but does not conclusively point to mechanisms or pathways that might effect the proteins involved in regulation of apoptosis. 18 Florida State University: Molecular Expressions. Mitochondria. http://micro.magnet.fsu.edu/cells/mitochondria/images/mitochondriafigure1.jpg (accessed November 10, 2011). 19 Lindsay, J.; Esposti, M.D.; Gilmore, A.P. Bcl-2 proteins and mitochondria – specificity in membrane targeting for death. Biochim Biophys Acta. 2011; 1813(4): 532-539. This article gives a detailed description of how BCL-2 proteins interact at the mitochondria to cause apoptosis. It characterizes the family members in terms of their BCL-2 homology domains and is a comprehensive overview of BCL-2 regulation. It discusses the two dominant theories of how BCL-2 proteins cause mitochondrial outer membrane permeabilization (including the subscribed to theory of activator and sensitizer proteins). This article describes the mechanisms by which BCL-2 proteins are recruited to the mitochondria, namely through n-terminus pre-sequences and c-terminus tail anchors. While it contains information extraneous to my project, there is a lot of information that has helped to formulate ideas about the potential interactions that could be occurring in my cell culture model. 20 Cell Signaling Technology. Apoptosis BH 1-4 Domains. http://www.cellsignal.com/reference/domain/bh14.html (accessed October 26, 2011). 21 Moore, V.D.G., Brown, J.R., Certol, M., Love, T.M., Tovina, C.D., Letai, A. Chronic lymphocytic leukemia requires BCL2 to sequester prodeath BIM, explaining sensitivity to BCL2 antagonist ABT-737. J. Clin. Invest. 2007; 117:112–121. 22 Brunelle, J.K., Letai, A. Control of mitochondrial apoptosis by the Bcl-2 family. J of Cell Science. 2009; 122:437-441. 23 Hasnan, J., Yusof, M.I., Damitri, T.D., Faridah, A.R., Adenan, A.S., Norbaini, T.H. Relationship between apoptotic markers (Bax and Bcl-2) and biochemical markers in type 2 diabetes mellitus. Singapore Med J. 2010; 51(1): 50-55. 24 van den Oever, I.A.M., Raterman, H.G., Nurmohamed, M.T., Simsek, S. Endothelial dysfunction, inflammation, and apoptosis in diabetes mellitus. Mediators of Inflammation. 2010; 1-15. Methods/Approach A cell culture model will be used to conduct this research. I have obtained the HL-1 line of mouse atrial cardiomyocytes, and am working on a hyperglycemia model. Cells will be grown with normal media (prepared as indicated by Dr. William Claycomb at Louisiana State University) to 80% confluence (or until they cover 80% of the growing surface). At that time, the media will be changed to the experimental media. Cells will either be treated with a control media, containing the typical amount of glucose for HL-1 cells, or hyperglycemic media, containing a high concentration of glucose. Cell viability will be determined through an MTT Assay, which measures the amount of a reactant solution cells are able to convert to a purple colored product to assess the health of the mitochondria (and by extension the cells). Apoptosis will be confirmed using a similar assay called a caspase-3 assay, which measures a color change produced when a reactant is cleaved by activated caspase-3. Increased cleavage indicates increased apoptosis. BCL-2 family protein presence will be assessed by a standard biochemical technique called Western Blotting. Proteins are extracted from the cells and separated based on size using a standard technique called electrophoresis. They are then transferred to a membrane, which is probed using an antibody specific to the protein of interest. This means that the antibody will bind to the protein on the membrane. Therefore, if the antibody binds to the membrane, it indicates the protein is present. Once the major proteins present have been determined, a technique called coimmunoprecipitation will be used to determine which proteins exist in complexes in the cells. This is similar to the Western Blotting procedure, however only proteins complexed (or interacting) with a specific protein of interest are initially run on the gel before antibody analysis. A novel technique (developed in my mentor’s post-doctoral research lab) called BH3-profiling will be then be used to determine which of the present proteins are the most important for regulation of cell death in normal and hyperglycemic HL-1 cells. A cross-linker, which is a chemical that preserves protein-protein interactions, will be used to determine the level of BAX/BAK oligomerization in the two cell cultures. This will help to confirm if this is the pathway of apoptosis being taken, as well as will provide more information about the BCL-2 protein changes being caused by hyperglycemia. Once the protein levels and interactions are determined, mitochondria will be isolated so that the location of the proteins can be determined. This is important because recruitment of BCL-2 proteins to the mitochondria indicates cell death. Understanding not only the concentration, but also the location, of the important proteins is crucial to understanding how hyperglycemia might promote apoptosis. Messenger RNA (mRNA) will be assessed to determine at what point any observed changes to BCL-2 are effected. If an increased amount of mRNA is observed, that means hyperglycemia causes an increase in the production of the protein of interest. If changes in mRNA levels are not observed, then it is likely that any changes to BCL-2 being observed occur as post-translational modifications (or occur after the protein has been synthesized). It will be important to know at which point any observed changes occur to understand how hyperglycemia produces increased apoptosis by modifying BCL-2 proteins involved in apoptosis regulation. Timeline Winter 2012 Spring 2012 Summer 2012 Fall 2012 Winter 2013 Spring 2013 Proposed activities Validate hyperglycemia model Conduct immunoprecipitaion studies Assess protein changes in hyperglycemia model Attend Cell Biology Conference (December 3-7) Winter term: 1 hour LUM 498 Use cross-linker to study BAX/BAK oligomerization Isolate mRNA & assess changes Present at SURF 1 hour LUM 498 Submit Junior Fellows Progress Report: March 30, 2012 REU or other external summer research program Isolate mitochondria and assess changes Submit abstract for American Society for Biochemistry and Molecular Biology (likely November) 1 hour LUM 498 Data analysis and preparation of manuscript for publication 1 hour LUM 498 Present at SURF Present at American Society for Biochemistry and Molecular Biology (April 20-24) 1 hour LUM 498 Manuscript finalized/final paper submitted: April 15, 2013 Submit Senior Fellows Progress Report (due one week before Senior Celebration) Participate in Leaders of the 21st Century and Fellows Senior Celebration (May) Budget/Budget Justification Items Fellows Lumen Total Cell Culture Reagents/supplies $100 $800 $900 Special chemicals, as well as sterile flasks, are needed for growing the cells. The majority of this has/will come out of my Lumen Budget. Protein analysis reagents $400 $3,500 $3,900 These will be used to analyze BCL-2 proteins, as well as changes to mitochondria. Antibodies as well as synthesized proteins are very expensive, so this will be one of the biggest expenses for my project. Miscellaneous supplies $200 $800 $1,000 Gloves, centrifuge tubes, pipettes, shipping fees for chemicals/supplies Conference fees $0 $2,500 $2,500 American Society for Cell Biology (December 2011), American Society for Biochemistry and Molecular Biology (April 2013), Poster printing Total $700 $7,600 $8,300