* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download histology of lymphoid organs lymphoid organs
Survey
Document related concepts
Immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Molecular mimicry wikipedia , lookup
Adaptive immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Innate immune system wikipedia , lookup
X-linked severe combined immunodeficiency wikipedia , lookup
Transcript
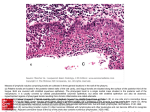
HISTOLOGY OF LYMPHOID ORGANS INTRODUCTION • Immune systems consists of : 4 – Lymphoid L h id organs – Heterogeneous group of motile cell types • 2 components of immune systems : 3 – IInnate t Immune I System S t Æ non spesific ifi (complement, ( l t macrophages & Neutrophils, Natural Killer cells/NK cells)) Æ nonclonal defense mechanism – Adaptive Immune System Æ specific (T Lymphocytes, B lymphocytes, Antigen Presenting C ll /APC ) Cells/APCs) • Adaptive immune system : 4 – Humoral immune response : B lymphocytes produce antibodies Æ phagocytosis & digestion of bacteria by macrophages & neutrophils leukocytes – A cell-mediated ll di t d immune i response : T lymphocytes bind to surface of parasites or virus-infected virus infected cells Æ lyse them by secreting a membrane-disrupting protein & a Hydrolytic Enzyme y Lymphoid organs : 1, 3 • Primary/central organs : Thymus & Bone Marrow Æ responsible for development & maturation of lymphocytes y p y • Secondary/Pheripheral y p organs g : Lymph nodes, Spleen, Tonsils, solitary nodules, Peyer’s Patches of ileum, Appendix Origin of Immune System Cells • Pluripotent hematopoetic stem cell in bone marrowÆ growth factors stimulation Æ proliferation and maturation of the cells Æ formed elements of the blood y progenitor p g cell & • Stem cell Æ myeloid lymphoid progenitor cells • Lymphoid progenitor cells Æ B lymphocytes & T lymphocytes Growth factors on hematopoietic p system y • G-CSF, GM-CSF, M-CSF, IL- 1, IL-3, IL-4, IL-6, EPO TPO etc EPO, etc. • Cytokines are a unique family of growth factors Æ messenger molecules that can communicate signals from one cell type to another – Secreted primarily from leukocytes but also produced by various cells of the body Æ interleukin (IL) – IL instruct the receiving cells to proliferate, differentiate, secrete additional cytokines cytokines, migrate or die – IL Stimulate both the humoral and cellular immune responses, as well as the activation of phagocytic cells – The list of identified interleukins grows continuously Origin of the main types of lymphocytes B lymphocytes and lymphocytes. natural killer lymphocytes are formed in the bone marrow and lea e the bone marrow leave marro already alread mature, to seed the secondary lymphoid organs and transit th through h the th blood, bl d epithelia, ith li andd connective tissues. Immature CD4– and CD8– T lymphocyte precursors are transported t t d by b the th blood circulation from the bone marrow to the thymus, where they complete l t their th i maturation t ti andd leave as either CD4+ or CD8+ cells. CLONAL SELECTION OF LYMPHOCYTES • In bone marrow & Thymus Æ primary lymphoid organ • Single type receptor on Lymphocytes can recognize all possible antigens Æ but self tolerance • Lymphocytes with receptors not self tolerance are eliminated li i t d by b apoptosis t i Æ clonal l l deletion d l ti B Lymphocytes Maturation • Bone marro marrow Æ Lymphoid L mphoid stem cell Æ Pro B cell Æ Pre B Cell Æ Immature/naive B cells (Ig M)Æ mature B Cells (Ig M + Ig D) Æ blood stream & circulate Æ secondary lymphoid organ • Proliferation lif i andd maturation i off B-cell ll responses are mediated by cytokines T Cells Maturation • Fetal liver/bone marrow Æ Pre T Cell Æ migrate g to Thymus y Æ Stage g 1: T cells with CD 4- & CD8- (double negative) Æ Stage 2: T Cells with CD 4+ & CD 8+ (Double positive) Æ Stage 3 : mature T Cell with CD4+ or CD 8+ (single positive) Approximate percentage of lymphocytes in l lymphoid h id organs1 Lymphoid organs Thymus T lymphocytes B Lymphocytes % % 100 0 Bone marrow 10 90 Spleen 45 55 L Lymph h nodes d 60 40 Blood 80 20 THYMUS • In superior mediastinum 1, 2 • 2 lobes Æ Thin capsules Æ septa Æ subdivide into incomplete lobules 1, 3 • Each lobule consist of cortex & , medulla:1,3 A.Cortex : • Darker than medulla Æ due to large number of T lymphocytes • Also contain macrophages & E ith li l Reticular Epithelial R ti l Cells C ll • 95-98% of developing T cells p p in cortex Æ die byy apoptosis phagocytosed by macrophages B. Medulla : 1, 3 – Stain lighter than cortex Æ less T cells population & large number b off epithelial ith li l reticular ti l cells – 3 types of epithelial reticular cells in medulla : o Type IV cells o Type V cells o T Type VI cells ll Æ Hassl’s H l’ Body / Thymic Corpuscle (found only in medulla, cornified, even calcified, unknown function) Thymus vascular supply1, 3 • Blood-thymus barrier Æ formed by continuous cappillaries in cortex with thick basal lamina, invested by sheath of type I epithelial reticular cells Æ preventing contact of developing T Cells to blood-borne macromolecules • Self macromolecules crossed barrier Æ to select & eliminate T cells react with self antigens Æ clonal selection & clonal deletion • No barrier in medulla • T cells leave medulla via veins drainning the thymus Hormones in thymus 1, 3 • Epithelial reticular cells produce : – Thymosin – Thymopoietin – Thymulin – Thymic Th i humoral h l factor f t Æ Facilitate T cell proliferation & expression of surface markers • Other hormones influence T cells maturation : – Corticosteroids Æ decrease T cells number in cortex – Thyroxin h i Æ stimulates i l epithelial i h li l reticular i l cells ll to increase i thymulin production – Somatotropin p Æ ppromotes T cells development p in thymus y cortex THYMUS INVOLUTION4 • Start after puberty • Parenchym replaced adipose tissue and connective tissue • Decrease weights : 40 g at puberty, 10-15 g late in life • After involution, thymus still has its function as a maturation place for T cells LYMPH NODE • Kidney shape, encapsulated (capsul of Conn. Tissue ÆTrabeculae) • Location : neck,, axilla,, scrotum,, blood vessels in thorax, etc 1, 2 • Have Afferent lymph vessel & Efferent lymph vessel 1 • Hilum : concave depresion which arteries & nerve enter, veins & lymphatic vessels leave1,2 • Parenchym composed of T cells, B cells, APCs & macrophages3 • On average, naive lymphocyte spend less than ½ hour h iin circulation i l i before b f homing h i to another lymphoid organ • 2 main ports of entry into Lymph Node : – By High Endothelial Venule (HEV) • Specialized type of post capillary venule, lined by cuboid or high endothelial cells • Found F d only l iin secondary d lymphoid l h id organs except spleen • Main site of B & T lymphocytes entry from blood Æ by diapedesis – By afferent lymph vessel Æ Site of some memory cells, free antigens & or antigen-loaded APC BLOOD & LYMPH CIRCULATION OF LYMPH NODE CORTEX 1, 2 o Outer Cortex • Lymphoid nodules – B cells Æ imunocytes – Germinal center/secondary nodules Æ only in response of antigenic challenge • Reticular cells & fiber o IInner Cortex/Paracortical C t /P ti l Area Æ T cells activated & proliferated o Subcapsular Sinus & intermediate/Peritrabekular Sinus Section of a lymph node showing the cortex and the medulla and their primary components. B: (1) Capsule; (2) lymphoid nodule with germinative center; (3) subcapsular sinus; (4) i t intermediate di t sinus; i (5) medullary d ll cords; d (6) medullary sinus; (7) trabecula. H&E stain. Low magnification. (Courtesy of PA Abrahamsohn.) Section of a portion of the outer cortex of a lymph node showing the capsule, subcapsular sinuses, diffuse lymphoid tissue and lymphatic nodules. tissue, nodules H&E stain stain. Medium magnification. (Courtesy of PA Abrahamsohn.) MEDULLA : 1, 2, 3 Medullary Cords : • B cells, plasma cells, macrophages • Reticular cells & fiber • More irregular trabeculae than in cortex Medullary Sinus Æ continue with subcapsular p sinus & intermediate sinus Æend up in efferent lymph vessels SPLEEN • • • • Largestt lymphoid L l h id organ in i body b d 3 Hilum Capsul Æ trabeculae Consist of : 1, 2, 3 A. White Pulp p: • Formed by : – Lymphoid nodules Æ B cells – Peri Arterial Lymphatic Sheath/PALS Æ formed by T cells surrounding A. Centralis • Lymphoid nodules Æ germinal centre due to antigenic challenge B. Marginal i l zone 3 – Separate white pulp to red pulp – Composed of plasma cells, T cells, B cells, macrophages, APCs – Marginal sinuses – Contain an abundance of blood antigens Æ plays l major j role l in i immunologic i l i activities ti iti off spleen 1 3 C Red C. R dP Pulp l :1, • Consist of : Splenic Cords / Billroth’s Billroth s Cords Æ macrophages, T cells, B cells, plasma cells, blood cells Splenic Sinusoids : Endothelial cells fusiform, elongated Discontinuous basal lamina Blood Circulation of Spleen TONSILS • Incompletely encapsulated aggregates of lymphoid nodules 1 • Based on location : p palatine,, pharyngeal, p y g , lingual g tonsils1 • Produce lymphocytes1 PALATINE TONSILS • A pair, in pars oralis pharynx1 1 2, 2 3 • Consist C i off : 1, – Stratified squamous p Epithelium – A band of lymphoid nodule with germinal center – Crypts C t : • Invagination of epithelium • 10-20 crypts/tonsil • Contain food debris, dead leucocytes, desquamated of epithelial cells,bacteria etc – C Capsule l Æ partially ti ll att the th base The palatine Th l ti t il consists tonsil i t off diffuse diff l lymphocytes h t and d lymphoid nodules disposed under a stratified squamous epithelium. One of the crypts of the tonsil is shown; the crypts often contain dead epithelial and inflammatory cells. B: (1) Crypt; (2) stratified squamous epithelium; (3) lymphoid nodules; (4) diffuse lymphoid tissue; (5) germinative center; (6) capsule; (7) mucous glands. Hematoxylin and eosin (H&E) stain. Low magnification. (Courtesy of PA Abrahamsohn.) PHARYNGEAL TONSILS • Single in posterior nasopharynx1, 2 1 22, 3 • Consist C i t off :1, – Pseudostratified ciliated columar epithelium – Lymphoid nodules – No crypts, only shallow longitudinal infolding called pleats l – Thinner capsule than T. Palatina LINGUAL TONSILS • Smaller & more numerous than other tonsils • At base of tongue • Consist of :1,, 2,, 3 – Stratified Squamous Epithelium – Lymphoid L h id nodules d l Æ germinal i l center t – Each lingual tonsils has a single crypts MUCOSA--ASSOCIATED LYMPHOID MUCOSA TISSUE / MALT3 • Non capsulated • Lymphoid nodules in mucosa or submucosa of GI tract respiratory tract tract, tract, urinary tract. Gut-Associated Associated lymphoid • Gut tissue (GALT) Æ peyer’s patches (B Cells surround b T cells by ll & APCs) APC ) • Bronchus-associated lymphoid tissue (BALT) Æ similar to peyer’s patches Section of lung showing a collection of lymphocytes in the connective tissue of the bronchiolar mucosa, an example of mucosa-associated i d lymphoid l h id tissue i (MALT). Pararosaniline—toluidine blue (PT) stain. Low magnification. REFERENCES : 1. 2. 3. 4. Basic Histology Text & Atlas , 10th ed. , L. Carlos Junquira MD, Jose Carneiro MD, Robert O. Kelley PhD, Lange Medical Books, Mc Graw Graw-Hill Hill , 2003. Pp 265 – 290. Essentials of Human Histology, 2nd Edition, William J. Krausse PhD PhD, Little Brown & Company (Inc) (Inc), 1996 1996. Pp 197-228 Color Textbook of Histologi, 2nd edition, Gartner LP, Hiatt JL WB S JL, Saunders d C Company, Phil Philadelphia, d l hi Pennsylvania, P l i 2001. Pp 273-299 Consise Histology, 2nd edition, Don W Fawcett, Ronald P Jensh, Arnold publisher, London, 2002. Pp 148-161