* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Audit
Genome evolution wikipedia , lookup
DNA damage theory of aging wikipedia , lookup
Cre-Lox recombination wikipedia , lookup
BRCA mutation wikipedia , lookup
Genealogical DNA test wikipedia , lookup
Public health genomics wikipedia , lookup
Extrachromosomal DNA wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Population genetics wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Genetic engineering wikipedia , lookup
Cell-free fetal DNA wikipedia , lookup
Designer baby wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Deoxyribozyme wikipedia , lookup
Medical genetics wikipedia , lookup
Non-coding DNA wikipedia , lookup
Genetic testing wikipedia , lookup
Frameshift mutation wikipedia , lookup
History of genetic engineering wikipedia , lookup
Cancer epigenetics wikipedia , lookup
Genome (book) wikipedia , lookup
Point mutation wikipedia , lookup
Microevolution wikipedia , lookup
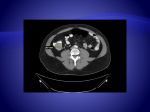
Audit of Lynch Syndrome (HNPCC) Carriers Northern Genetic Service Alex Henderson Consultant Clinical Geneticist Lorraine Cowley Principal Genetic Counsellor Lynch Syndrome/HNPCC Update of Genetics of Lynch Syndrome/HNPCC Results of Northern Genetics Service audit of screening in patients with known MMR genetic abnormalities Further audit plans Lynch syndrome/HNPCC Lynch syndrome (Hereditary non-polyposis colorectal cancer) is an autosomal dominant genetic condition which has a high risk of colon cancer as well as other cancers including: endometrium, ovary, stomach, small intestine, hepatobiliary tract, upper urinary tract, brain, skin. The increased risk for these cancers is due to inherited mutations that impair DNA mismatch repair. DNA mismatch repair DNA mismatch repair is a system for recognising and repairing erroneous insertion, deletion and mis-incorporation of bases that can arise during DNA replication and recombination, as well as repairing some forms of DNA damage. Mutations in the DNA mismatch genes (specifically the human homologues of the Mut proteins) affect genomic stability which can result in microsatellite instability (MI). Microsatellite Instability Microsatellites are repeated sequences of DNA. These repeated sequences are common, and normal. Although the length of these microsatellites is highly variable from person to person, each individual has microsatellites of a set length. In cells with mutations in DNA repair genes, some of these sequences accumulate errors and become longer or shorter. The appearance of abnormally long or short microsatellites in an individual's DNA is referred to as microsatellite instability. MI is implicated in most human cancers. Specifically the overwhelming majority of cancers in HNPCC are attributed to mutations in MMR genes . Cancer risks in Lynch Syndrome Individuals with HNPCC mutation have about an 80% lifetime risk for colon cancer. Two-thirds of these cancers occur in the proximal colon. The mean age of colorectal cancer diagnosis is 44 for members of families that meet the Amsterdam criteria. Women with HNPCC have a 80% lifetime risk of endometrial cancer. The average age of diagnosis of endometrial cancer is about 46 years. Amsterdam criteria The initial Amsterdam criteria were a series of clinical criteria that were colloquially known as the ‘‘3-2-1’’ rule: At least 3 relatives with histologically confirmed colorectal cancer, 1 of whom is a first degree relative of the other 2; familial adenomatous polyposis should be excluded; At least 2 successive generations involved; At least 1 of the cancers diagnosed before age 50. These criteria were expanded to include the associated non-colorectal cancers: 3 or more relatives with an HNPCC associated cancer; 2 or more successive generations affected; 1 or more relatives diagnosed before the age of 50 years; 1 should be a first-degree relative of the other two. Bethesda Guidelines The Bethesda guidelines are an alternative method for the identification of individuals who should receive genetic testing for Lynch syndrome related tumors: Colorectal carcinoma (CRC) diagnosed in a patient who is less than 50 years old; Presence of synchronous or metachronous CRC or other Lynch syndrome-associated tumors, regardless of age; CRC with high microsatellite instability histology diagnosed in a patient less than 60 years old; CRC diagnosed in one or more first-degree relatives with a Lynch syndrome-associated tumour, with one of the cancers being diagnosed at less than 50 years of age; CRC diagnosed in two or more first-degree or second-degree relatives with Lynch syndrome-associated tumours, regardless of age Genes implicated in HNPCC Genes MLH1 MSH2 MSH6 PMS2 PMS1 TGFBR2 MLH3 Frequency 30% 60% 7-10% <5% case reports case reports disputed Locus 3p21.3 2p22 2p16 7p22 2q31q33 3p22 14q24.3 Genetic testing in Lynch Syndrome Genetic testing for mutations in DNA mismatch repair genes is expensive and time-consuming. In general, we try to identify those families where we are most likely to identify mutations: 1. The Amsterdam Criteria are useful, but do not identify up to 30% of potential Lynch syndrome carriers. 2. Microsatellite instability can be assessed in tumour specimens; when microsatellite instability is identified (or MSI-H) there is a high likelihood for a Lynch syndrome diagnosis. 3. Immunohistochemistry testing also allows testing for expression of DNA mismatch repair genes; by combining this with MSI, an additional >30% of Lynch syndrome carriers who would have been missed on MSI profiling alone are identified. Sensitivity of Amsterdam and Bethesda Criteria Not all families fulfilling the clinical criteria for Lynch syndrome have an identifiable deleterious mutation in the MMR genes. Conversely, many families who do not fulfil the criteria have been found to harbour MMR mutations. A recent review of sensitivity and specificity suggest that the revised Amsterdam criteria are met by 62%, 48%, 87% and 38% of families with mutations in MSH2, MSH6, MLH1 and PMS2. The Bethesda criteria had low sensitivity for identifying MSH6 or PMS2 mutations. Amsterdam and Bethesda criteria are inadequate for identifying all mutations – particularly in MSH6/PMS2, implying that MSH6 mutations may be more common than currently assumed. Clinical Management in Lynch Syndrome Screening remains mainstay of management. NGS guidelines are based on The British Society of Gastroenterology and the Association of Coloproctology for Great Britain and Ireland update guidelines of 2010: 18-24 monthly colonoscopy from 25 years; 2 yearly OGD from 50 years to 75 in patients with family history of gastric cancer. Aspirin Prevents Cancer in Lynch Syndrome http://www.audiomedica.com/oncology/longerfollow-up-reveals-aspirin-prevents-cancer-inlynch-syndrome/ Audit - Introduction 212 patients identified, 197 suitable for audit Aim: To find out the referral and follow up pattern of patients who have received a MMR gene diagnosis through the Northern Genetic Service. Practice compared to department standards: 2 Yearly bowel screening Gynaecological advice over 35, discussion about surgery if peri or post menopausal Opportunity to access genetics department How many patients have been referred for Bowel Surveillance? Reason for no referral Number of Patients Future Contact 5 No referral Declined (1) No record (2) No Colon (3) One off (3) (too old to start regular screening) 9 Offered referral but no response 3 What type of Gynaecological Surveillance is offered? What Genetic Follow up is offered? Conclusion Bowel Surveillance Gynaecological Awareness Genetic Follow Up What Next?