* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Atherosclerosis wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
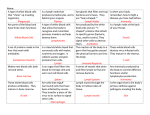
Gross Anatomy Lymph Lymph is a fluid derived from blood plasma. It is pushed out through the capillary wall by pressure exerted by the heart or by osmotic pressure at the cellular level. Lymph contains nutrients, oxygen, and hormones, as well as toxins and cellular waste products generated by the cells. As the interstitial fluid accumulates, it is picked up and removed by lymphatic vessels that pass through lymph nodes, which return the fluid to the venous system. As the lymph passes through the lymph nodes, lymphocytes and monocytes enter in the lymph node At the level of the gastrointestinal (GI) tract, lymph has a milky consistency that is attributable to fatty acids, glycerol, and rich fat content. Lacteals are lymph vessels that transport intestinal fat and are localized to the GI tract. Lymphatic vessels Lymphatic capillaries are blind-ended tubes with thin endothelial walls (only a single cell in thickness). They are arranged in an overlapping pattern, so that pressure from the surrounding capillary forces at these cells allows fluid to enter the capillary. The lymphatic capillaries coalesce to form larger meshlike networks of tubes that are located deeper in the body; these are known as lymphatic vessels. The lymphatic vessels grow progressively larger and form 2 lymphatic ducts: the right lymphatic duct, which drains the upper right quadrant, and the thoracic duct, which drains the remaining lymphatic tributaries. Like veins, lymphatic vessels have 1-way valves to prevent any backflow. The pressure gradients that move lymph through the vessels come from skeletal muscle action, smooth muscle contraction within the smooth muscle wall, and respiratory movement. Lymph nodes Lymph nodes are bean-shaped structures that are widely distributed throughout the lymphatic pathway, providing a filtration mechanism for the lymph before it rejoins the blood stream. The average human body contains approximately 600-700 of them, predominantly concentrated in the neck, axillae, groin, thoracic mediastinum, and mesenteries of the GI tract. Lymph nodes constitute a main line of defense by hosting 2 types of immunoprotective cell lines, T lymphocytes and B lymphocytes. Lymph nodes have 2 distinct regions, the cortex and the medulla. The cortex contains follicles, which are collections of lymphocytes. At the center of the follicles is an area called germinal centers that predominantly host B-lymphocytes while the remaining cells of the cortex are T-lymphocytes. Vessels entering the lymph nodes are called afferent lymphatic vessels and, likewise, those exiting are called efferent lymphatic vessels (see the image below). Extending from the collagenous capsule inward throughout the lymph node are connective tissue trabeculae that incompletely divide the space into compartments. Deep in the node, in the medullary portion, the trabeculae divide repeatedly and blend into the connective tissue of the hilum of the node. Thus the capsule, the trabeculae, and the hilum make up the framework of the node. Within this framework, a delicate arrangement of connective tissue forms the lymph sinuses, within which lymph and free lymphoid elements circulate. A subcapsular or marginal sinus exists between the capsule and the cortex of the lymph node. Lymph passes from the subcapsular sinus into the cortical sinus toward the medulla of the lymph node. Medullary sinuses represent a broad network of lymph channels that drain toward the hilum of the node; from there, lymph is collected into several efferent vessels that run to other lymph nodes and eventually drain into their respective lymphatic Spleen The spleen, the largest lymphatic organ, is a convex lymphoid structure located below the diaphragm and behind the stomach. It is surrounded by a connective tissue capsule that extends inward to divide the organ into lobules consisting of cells, small blood vessels, and 2 types of tissue known as red and white pulp. Red pulp consists of venous sinuses filled with blood and cords of lymphocytes and macrophages. Thus, the red pulp of the spleen is composed of thin-walled vascular sinusoids separated by fibrovascular splenic cords. These sinusoids are lined by a discontinuous epithelium, allowing passage of cells between the cords and the sinuses. The sinuses are lined with macrophages which are loosely connected by long dendritic processes, creating a filter through which the blood can seep. These sinuses act to trap red cell inclusions. These also act to trap older red blood cells (>120 days) for recycling, and to trap platelets. In a normal adult, up to 2 liters of blood per minute will filter through the spleen. White pulp is lymphatic tissue consisting of lymphocytes around the arteries. Lymphocytes are densely packed within the cortex of the spleen. The white pulp surrounds the central arteries as a peri-arterial lymphoid sheath (PALS). Lymphocytes of the PALS are likely to be T-lymphocytes. In addition, we see macrophages and plasma cells in the PALS. Lymph nodules, formed by B-lymphocytes, are present along the course of the central arteries. The central arteries are typically located in the periphery of the nodule. The spleen is surrounded by a capsule of dense connective tissue from which branched trabecula that extends into the parenchyma of the spleen. The parenchyma of the spleen is termed the pulp of the spleen. Most of the pulp of a fresh, unfixed spleen is a soft, dark red mass, the red pulp. It consists of large, irregular, thin-walled blood vessels, the splenic sinusoids, interposed between sheets and strands of reticular connective tissue, the splenic cords (of Billroth). Within the red pulp small, oval or rounded greyish white areas, the white pulp, is formed by lymphoid tissue. The spleen filters blood in much the same way that lymph nodes filter lymph. Lymphocytes in the spleen react to pathogens in the blood and attempt to destroy them. Macrophages then engulf and phagocytose damaged cells and cellular debris. The spleen, along with the liver, eradicates damaged and old erythrocytes from the blood circulation. Like other lymphatic tissue, it produces lymphocytes in an immunologic response to offending pathogens Therefore, the spleen conducts several important functions, as follows: It serves as a reservoir of lymphocytes for the body It filters blood It plays an important role in red blood cell and iron metabolism through macrophage phagocytosis of old and damaged red blood cells It recycles iron by sending it to the liver It serves as a storage reservoir for blood It contains T lymphocytes and B lymphocytes for immunologic response The spleen is, like the lymph nodes, a discriminatory filter. Unlike the lymph nodes, the spleen is inserted into the blood stream. The spleen clears the blood of aged blood cells and foreign particles and is the site of immune reactions to blood-borne antigens. The spleen is not essential to life in adult individuals. Other organs can take over its functions if the spleen is removed. Branches of the splenic artery (Where does it enter the spleen?) divides into trabecular arteries (Where are they found?), which enter the white pulp, where they are called central arteries. Branches of the central artery almost all divide into smaller vessels in the marginal zone, i.e. the border between the red and white pulp. Fine branches of the central artery - penicillar arteries (cuboidal epithelium) - branch again to form arterial capillaries, which, as they exit the white pulp, are surrounded by a sheath of phagocytotic cells and reticular fibres. They are now called sheathed arteries. From here, the blood enters the red pulp. Sheathed arteries may empty the blood which they carry directly into the splenic sinusoids (closed circulation, about 90% in cats) or into the reticular connective tissue of the splenic cords (open circulation). Macrophages are, in addition to reticular cell, the main resident cell population of the splenic cords. Blood cells which are emptied into the splenic cords re-enter the blood vessels through the endothelium of the sinusoids. The endothelial cells are elongated (in cross section they may appear cuboidal) and oriented along the long axis of the sinusoids. The endothelium of the sinusoids has no junctional complexes and its basement membrane is incomplete (forming narrow circular bands around the endothelial cells with large intervening fenestrations). Macrophages ingest aged erythrocytes, platelets and other particulate matter as they pass through the splenic cords. The composition of the plasma membrane of erythrocytes changes as the cell ages. It is thought that these changes eventually expose erythrocyte senescence antigens, which bind blood-borne antibodies and thus tag the erythrocyte for removal by macrophages. Erythrocyte removal is also one function of the resident macrophages of the liver, although splenic macrophages take care of most of the job. The sinusoids continue into the veins of the pulp, which empty into thinwalled trabecular veins, which eventually coalesce to form the splenic vein. The thymus The thymus is a bilobed lymphoid organ located in the superior mediastinum of the thorax, posterior to the sternum. After puberty, it begins to decrease in size; it is small and fatty in adults after degeneration. The primary function of the thymus is the processing and maturation of T lymphocytes. While in the thymus, T lymphocytes do not respond to pathogens and foreign organisms. After maturation, they enter the blood and go to other lymphatic organs, where they help provide defense. Structurally, the thymus is similar to the spleen and lymph nodes, with numerous lobules and cortical and medullary elements. It also produces thymosin, a hormone that helps stimulate maturation of T lymphocytes in other lymphatic organs. functions mainly in fetal life and early childhood. By puberty, the lymphoid tissues have largely been replaced by adipose tissue. The functional thymus is composed of two regions: the outer cortex and the inner medulla. Within the medulla are central structures known as Hassall's corpuscles that are composed of tight nests of epithelial cells. From the stem cells are derived pre-T cells that migrate from the cortex to the medulla, where they become functional CD4 and CD8 cells. The cortex is isolated from the thymic medulla by epithelial reticular cells. During development, about 98% of T cells in the cortex do not pass inspection for one reason or another (such as abnormal recognition of self-antigens) and are destroyed before reaching the thymic medulla, from which they are sent out to lymphoid regions throughout the body. In the adult thymus, there is no defined cortex and medulla. It is atrophic and mainly replaced by adipose tissue, though some lymphocytes and Hassall's corpuscles remain. Tonsils Tonsils are aggregates of lymph node tissue located under the epithelial lining of the oral and pharyngeal areas. The main areas are the palatine tonsils (on the sides of the oropharynx), the pharyngeal tonsils (on the roof of the nasopharynx; also known as adenoids), and the lingual tonsils (on the base of the posterior surface of the tongue). Because these tonsils are so closely related to the oral and pharyngeal airways, they may interfere with breathing when they become enlarged. The predominance of lymphocytes and macrophages in these tonsillar tissues offers protection against harmful pathogens and substances that may enter through the oral cavity or airway.[1, 2] Hematopoietic and Lymphoid Tissues Mucosa-Associated Lymphoid Tissue (MALT) The mucosal lining of the alimentary canal and airways is in many ways specialised to facilitate the exchange of substances between the external environment and the body. Unfortunately, these specialisation do not just apply e.g. to components of the digested food but also pathogens. This is combined with excellent living conditions for bacteria in parts of the alimentary canal - in particular the ileum and the colon. Lymphoid tissue located beneath the mucosal epithelia, mucosa-associated lymphoid tissue (MALT), protects the body against pathogens that may enter the body via the mucosa. The importance of this task is reflected in the mass of the MALT, which corresponds to the combined mass of the other lymphoid organs and tissues. The task that the immune cells of the MALT have to accomplish is different from that of other parts of the immune system. We do need a defense against pathogens, but it would not be a good idea to mount an immune response against components of the food. Immune cell activation therefore differs between the MALT and other lymphoid tissues. This difference is mediated by different receptors expressed by immune cells of the MALT and by different substances which they release upon contact with an antigen. Because of their specific functions, immune cells of the MALT do not mingle with other immune cells. Epithelial cells of the vessels supplying the MALT express specific receptor which are recognized by MALT immune cells and allow their homing to the MALT during recirculation. Lastly, MALT plasma cells produce a secretable form of antibodies, immunoglobulin type A dimers, which can be taken up by epithelial cells and then released onto the epithelial surface. Specialisation of MALT immune cells occur at the molecular level. In routine histological preparations, immune cells of the MALT look pretty much like immune cells of other lymphoid tissues. In the lamina propria and submucosal regions of the gastrointestinal tract from the tongue to the colon are collections of lymphoid tissue. In some areas, the lymphoid tissue is more prominent: Lingual Tonsil: at the posterior tongue are larger collections of lymphoid tissue. Pharyngeal Tonsil: these are the structures commonly called "tonsils" and comprise tissues functionally equivalent to lymph nodes. Peyer's Patches: these are ovoid areas from 0.5 to 1.5 cm wide and 1 to 4 cm long located in the terminal ileum. Appendix: the appendiceal submucosa contains abundant lymphoid tissue. Bone Marrow Early in fetal life, hematopoiesis begins as red blood cell precursors appear in the yolk sac at 2 weeks gestation. In the first trimester, hematopoiesis can be found in the spleen, but in the late first trimester and throughout most of the second trimester and well into the third trimester, the major hematopoietic organ is the liver. This extramedullary hematopoiesis (blood cell production outside the marrow) is normal. Beginning in the late first trimester, the bones become large enough to have marrow cavities, and hematopoiesis becomes established in marrow, increasing there until, at term, the majority of hematopoiesis occurs in the marrow. However, at term and continuing for a month or more, extramedullary hematopoiesis can still be found in the liver. Under condition of fetal and neonatal stress, hematopoiesis can shift outside of the marrow (extramedullary hematopoiesis) to other organs. Throughout childhood, many long bones contain red marrow, with hematopoietic elements, as well as the vertebral bone marrow, pelvis, ribs, and sternum. In adults, there is little red marrow in long bones, but mostly fatty marrow. An indicator of the reduction in mass of red marrow is the posterior iliac crest, the most common site for bone marrow biopsy. At age 50, the posterior iliac crest marrow is about 50% composed of hematopoietic elements, the rest fatty marrow. The cellularity decreases on average 10% per decade thereafter. In the elderly, most hematopoiesis is confined to vertebrae, ribs, and sternum. This is enough for normal circumstances, but in times of stress with blood loss and infection, for example, the demand for blood cell production can be increased, and the elderly (as well as infants) do not have a large reserve marrow capacity. When a bone marrow biopsy is performed, an aspirate of the marrow is also performed (and at some sites such as sternum, this is all that is done). The aspirate is made into bone marrow smears that are stained with Wright-Giemsa. It is easy to identify myelopoietic, erythroid, and megakaryocytic elements in the smears and count them to determine their relative numbers. The hematopoietic elements are present between the bone spicules. The marrow has a rich vascular supply, as well as sinusoids. The primordial cell that gives rise to all hematopoietic elements, as well as lymphoid cells, is the pleuripotential stem cell. A few of these cells circulate, but their job is to home in on marrow and establish cell lines for blood cell production. This pleuripotential stem cell gives rise to two cell lines: Uncommitted lymphoid stem cell: this in turn give rise to the B stem cells and the T stem cells that establish populations of B lymphocytes and T lymphocytes. Hematopoietic stem cell: from this line arise three additional subpopulations: the granulocyte-monocyte line, the megakaryocytic line, and the erythroid line. The granulocyte-monocyte line further differentiates into cell lines producing monocytes and granulocytes. The marrow is principally populated by the cell lines that are involved with myelopoiesis (granulocytes), erythropoiesis (red blood cells), and megakaryopoiesis (platelets) which will circulate in the bloodstream. The types of white blood cells that circulate include: Neutrophils: these cells have prominent cytoplasmic granules that are lysosomes containing the enzymes released when neutrophils are recruited into inflammatory reactions. The neutrophils have multilobed nuclei. Circulating neutrophils last about 12 hours and, therefore, must constantly be replaced from the marrow. Band neutrophils: a few of these slightly immature neutrophils circulate, and they have a crescent shaped nucleus that has not yet become lobated. They also have cytoplasmic granules. Lymphocytes: both T and B cells circulate, with about 80% of the peripheral blood lymphocytes being T cells. These cells have a single large nucleus and scant blue cytoplasm. Lymphocytes can live for months to years. Monocytes: these cells have a larger nucleus than lymphocytes, and it is folded. There is more cytoplasm than lymphocytes, and it is grey. Blood monocytes can migrate into tissues and become macrophages that persist for weeks to months. Eosinophils: these specialized granulocytes are not numerous. They have prominent bright red cytoplasmic granules. They respond to allergic reactions and parasitic infections. Basophils: these granulocytic cells have prominent dark purple cytoplasmic inclusions. They are the least numerous of circulating white blood cells. A differential count is routinely performed with a complete blood count (CBC) to determine the relative numbers of the white blood cells in the peripheral blood. The peripheral blood smear is scanned and 100 white blood cells are counted. Below is an example: Cell Type Count Normal Range (%) Segmented Neutrophil 61 45 - 79 Band Neutrophil 2 0-5 Lymphocyte 24 16 - 47 Monocyte 8 0-9 Eosinophil Basophil 4 1 0-6 0-3 Megakaryocytes are the prominent large multinucleated cells scattered through the bone marrow. Platelets are the circulating fragments of megakaryocyte cytoplasm. The platelets are involved in coagulation. They are short-lived, only lasting a few days. Platelets have cytoplasmic granules, but no nucleus. The major cell types of lymphoid tissues include T cells and B cells, both derived from an uncommitted lymphoid stem cell. The designation "T" derives from the origin of many T cells in the thymus. The "B" cells are the "bursa equivalent" cells (so named because in birds, B cells are concentrated in a bursa of Fabricius next to the gut, and early studies were done in birds). The B cells are responsible for production of globular proteins known as immunoglobulins that are directed against antigens. B cell markers include the CD19 and CD20 antigens. The immunoglobulins are, therefore, antibodies. The cells specialized to produce immunoglobulins are plasma cells. The plasma cells have an eccentrically placed nucleus with radially-arranged chromatin, a prominent Golgi apparatus next to the nucleus (the perinuclear "hof"), and abundant cytoplasmic endoplasmic reticulum for synthesizing immunoglobulin. Plasma cells specialize in terms of antibody production. Different plasma cells can make immunoglobulin types G, A, M, D, and E. When the immune system responds to an infection, there are typically antibody responses to a variety of antigens, so that there are different types of immunoglobulin produced with specificities for the antigens. Such a response is called "polyclonal" because several clones of plasma cells, each producing a specific antibody, are stimulated to produce different immunoglobulins (mostly IgG, but the earliest production of antibody is of the IgM type). A neoplastic transformation of B cells that results in a proliferation of plasma cells causes a "monoclonal" production of immunoglobulin, because the neoplasm (called a myeloma) is a proliferation derived from a single clone. The use of immunizations (e.g., to protect against childhood infections such as rubella or pertussis) is based upon the introduction of antigenic components of the infectious agent into the body that stimulate the immune system to produce specific antibodies. An encounter with the real infectious agent at a later date will result in quick production of antibodies against the infectious agent, because there are circulating antibodies as well as plasma cells in "storage" waiting to respond to the challenge. The T cells are primarily involved in cell-mediated immune responses. They are identified by the presence of the CD3 antigen. In fetal life and childhood, the T cells arose in the thymus and then populated other lymphoid tissues. The major T cells are the "helper" cells that mark with the CD4 antigen and the "suppressor" cells that mark with the CD8 antigen. The recognition and stimulation of T cells is largely dependent upon recognition of major histocompatibility complex (MHC) antigens, also known as HLA antigens. Many cells of the human body express these antigens. The T cells are often aided by macrophages, which phagocytize infectious agents, process the antigens, and present them to the T cells (and to B cells). Antibodies coating an invading micro-organism can lead to lysis by specialized lymphocytes called "natural killer" or NK cells./P> Mast cells are specialized cells that have many cytoplasmic granules that can be released in response to inflammatory reactions, particularly type I hypersensitivity reactions. The granules contain mediators of the inflammatory process such as histamine. Dendritic reticulum cells serve to assist in storing and transferring antigens to lymphoid cells which will respond to the antigens. The dendritic cells located in skin and mucous membranes are known as Langerhans cells. Within lymph nodes, they are known as follicular dendritic cells. These dendritic cells are named because of the long cell processes which catch antigens and "warehouse" them.