* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The integration of T cell migration, differentiation and function
Survey
Document related concepts
Transcript
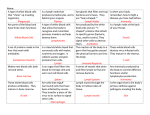
REVIEWS The integration of T cell migration, differentiation and function David Masopust and Jason M. Schenkel Abstract | T cells function locally. Accordingly, T cells’ recognition of antigen, their subsequent activation and differentiation, and their role in the processes of infection control, tumour eradication, autoimmunity, allergy and alloreactivity are intrinsically coupled with migration. Recent discoveries revise our understanding of the regulation and patterns of T cell trafficking and reveal limitations in current paradigms. Here, we review classic and emerging concepts, highlight the challenge of integrating new observations with existing T cell classification schemes and summarize the heuristic framework provided by viewing T cell differentiation and function first through the prism of migration. Department of Microbiology, Center for Immunology, University of Minnesota Medical School, Minneapolis, Minnesota 55455, USA. Correspondence to D.M. e-mail: [email protected] doi:10.1038/nri3442 Published online 19 April 2013 The fundamental problem that T cells must solve is making contact with rare antigen-bearing cells. This is no easy task, given that a single T cell occupies only one onehundred-trillionth of the volume of an adult human. This feat is achieved in a timely manner by targeted migration (homing), a process that is coordinately regulated with T cell differentiation state. Naive T cells recirculate through the paracortical regions of secondary lymphoid organs (SLOs), a strategy that maximizes their opportunity for antigen detection. Activated effector T cells disseminate broadly to exert contact-dependent functions. After antigen clearance, memory T cells remain distributed throughout the organism, providing an anatomically pervasive network for immunosurveillance. Memory T cells themselves are quite heterogeneous, with their functions being integrated with their location. New approaches and technologies have precipitated several recent important discoveries related to T cell migration. These observations, which include visualization of T cell mobility within different lymphoid and non-lymphoid compartments, refinements in our understanding of T cell egress, the concept of T cell residency, new insights into the regulation of homing molecule expression and further dissection of the relationship between T cell location and function, are shaping models of lineage differentiation and the perceived requirements for effective immunosurveillance. This Review summarizes the recent literature, synthesizes emerging concepts and highlights future directions for the field. Immunosurveillance by naive T cells Entry into secondary lymphoid organs. The adult mouse contains several billion cells, only ~100 of which are naive T cells with specificity for any single given peptide–MHC complex 1,2. However, immunization is sufficient to initiate recognition and subsequent activation of essentially all naive T cells within 3 days1. This remarkable feat is mediated by the antigen collecting capacity of SLOs coupled with the selective migration of naive T cells to these sites. Enough lymphocytes leave lymph and enter the subclavian vein to replace all blood-borne lymphocytes 11 times daily3. Half a century ago, Gowans traced the fate of these cells, discovering that small lymphocytes continuously recirculate among blood, SLOs and lymph4 (FIG. 1a). Naive blood-borne T cells enter SLOs within 30 minutes5, where they scan antigen-presenting cells (APCs) for cognate antigen before egressing via the efferent lymphatics. They then pass through the thoracic duct before returning to the blood ~10–20 h later to begin the cycle anew 6,7. To overcome shear forces in blood, lymphocytes must tether; this precipitates their rolling on high endothelial venules (HEVs), a specialized type of post-capillary vascular endothelium present within lymph node paracortical regions. This action is typically mediated via short-term interactions between CD62L (L‑selectin) on T cells and 6‑sulpho sialyl Lewis X oligosaccharides that decorate various core proteins expressed on HEVs8,9. Peripheral node addressin (PNAd) is a widely used term to collectively denote CD62L‑reactive ligands within HEVs. Selectin-mediated tethering affords the opportunity for chemokine sampling via G‑protein-coupled chemokine receptors expressed by T cells. CC‑chemokine ligand 21 (CCL21), which is immobilized on HEVs via binding to heparin glycosaminoglycans, is recognized by CC‑chemokine receptor 7 (CCR7) and mediates signalling and subsequent activation of lymphocyte functionassociated antigen 1 (LFA1; also known as integrin-αL)10. NATURE REVIEWS | IMMUNOLOGY VOLUME 13 | MAY 2013 | 309 © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS a c Efferent lymph Thoracic duct Non-lymphoid tissue CCR7 ‘Upstream’ lymph node T cell Lymph node CCR7 dependent Efferent lymphatic b Afferent lymphatic Afferent lymphatic Heart B cell follicle HEV Paracortex (T cell zone) CD62L Rolling Environment rich in CCL19 and CCL21 HEV PNAd S1P dependent LFA1 CCR7 Sinus CCR7 dependent Activation Efferent lymphatic Environment rich in S1P CCL21 d Time in lymph node Arrest S1PR1 ↑ sensitivity to S1P ↓ sensitivity to CCL19 and CCL21 ICAM1 Time in lymph CCR7 ↑ sensitivity to CCL19 and CCL21 ↓ sensitivity to S1P Figure 1 | T cell recirculation through lymph nodes. a | T cells enter lymph nodes from blood, then exit lymph nodes via Nature Reviews | Immunology efferent lymph. Efferent lymph collects in the thoracic duct before returning to blood. b | Many T cells enter lymph nodes from blood within high endothelial venules (HEVs). These specialized post-capillary venules constitutively express homing molecules that allow rolling, activation and arrest. c | T cells may also enter the lymph node sinuses via the lymphatics, either from upstream lymph nodes or from non-lymphoid tissues. Regardless of the mechanism of lymph node entry, further migration into the T cell zone is CC‑chemokine receptor 7 (CCR7) dependent. d | Sphingosine-1‑phosphate (S1P) is present in blood and lymph, whereas CC‑chemokine ligand 19 (CCL19) is expressed in lymph node T cell zones. Exposure to either CCL19 or S1P induces transient CCR7 or S1P receptor 1 (S1PR1) desensitization, respectively. This process ensures that T cells recirculate among lymph nodes, lymph and blood, rather than dwelling indefinitely in one compartment. ICAM1, intercellular adhesion molecule 1; PNAd, peripheral node addressin. Activated LFA1 binds intercellular adhesion molecule 1 (ICAM1), and this precipitates T cell arrest within HEVs, followed by their transmigration into the T cell zone (also referred to as the paracortex) of lymph nodes. Thus, CD62L, CCR7 and LFA1 together mediate the requisite rolling, activation and arrest processes by which naive T cells selectively enter lymph nodes (FIG. 1b). Each homing receptor is required, thus allowing selective recruitment of specific cell subsets. For example, neutrophils express CD62L but lack CCR7, and thus are excluded from routine traffic through lymph nodes11. The requisite involvement of three distinct homing receptors allows for considerable combinatorial complexity, as three different selectins, 18 distinct chemokine receptors and numerous integrin heterodimers that may contribute to homing have been identified12. As discussed later in this Review, effector subsets of T cells use distinct combinations of homing molecules to specifically migrate where needed. It should be noted that the requirement for CD62L and CCR7 for SLO entry is not absolute. α4β7 integrin, which is expressed at low levels among naive T cells, can mediate rolling via interaction with mucosal vascular addressin cell adhesion molecule 1 (MADCAM1), which is expressed on the HEVs of gut-associated SLOs13. Consequently, genetic defects in CD62L do not impair T cell homing to Peyer’s patches and only modestly impair migration to mesenteric lymph nodes. Neither rolling nor CD62L is required for entering the splenic white pulp owing to the low shear forces in spleen. Moreover, a small fraction of memory T cells can use CXC-chemokine receptor 4 (CXCR4) rather than CCR7 to traffic into lymph nodes, although the significance of this observation is not yet clear 14–16. After lymph node entry via HEVs, naive T cells may enter downstream lymph nodes via the lymphatics. Many lymph nodes are arrayed in chains. Accordingly, 310 | MAY 2013 | VOLUME 13 www.nature.com/reviews/immunol © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS many lymph nodes will have afferent lymphatic inputs that effectively represent a continuation of the efferent vessels of more peripheral lymph nodes in addition to those inputs that directly drain non-lymphoid tissues. A recent study demonstrated that when T cells are injected directly into the lymphatics afferent to the popliteal lymph node, they traffic through the subcapsular sinus and accumulate in the medullary sinus and cords17. Whereas this process is putatively selectin- and chemokine-independent, subsequent chemotaxis to the paracortex still requires CCR7. Afferent lymphatic entry is likely to represent a prominent pathway by which naive T cells enter downstream lymph nodes (FIG. 1c). T cell egress from non-lymphoid tissues (discussed below) highlights another context in which they enter lymph nodes via the afferent lymphatics, although this pathway may be limited to antigen-experienced T cells. Motility and egress. In addition to their functions in T cell recruitment and antigen collection, lymph nodes must provide an environment that maximizes cell‑to‑cell collaboration. After T cells enter lymph nodes, chemokinesis within the T cell zone is CCR7 dependent. In addition to CCL21, CCL19 (an alternative ligand for CCR7) is expressed in the T cell zone and increases T cell motility 18. This facilitates scanning; it is estimated that a single dendritic cell (DC) encounters up to 500 T cells per hour 19. Competing forces are likely to regulate the longevity of T cell retention within the lymph node. Sphingosine-1‑phosphate (S1P) induces chemotaxis of T cells and is abundantly expressed in blood and lymph, but it is absent from the T cell zone of lymph nodes and splenic white pulp. As S1P induces transient desensitization of S1P receptor 1 (S1PR1), recent migrants that enter SLOs from blood or afferent lymph are relatively insensitive to S1P signals within efferent lymph and thus are not initially drawn to exit 20,21. Indeed, treatment with artificial S1P agonists, such as FTY720, transiently blocks egress and results in accumulation of T cells within SLOs22,23. Similarly, CCL19 induces desensitization of CCR7 (REFS 24–26). Consequently, the strength of CCR7‑dependent retention within the T cell zone will gradually diminish the longer that resting T cells are positioned within SLOs. Contemporaneously, the sensitivity to S1P emanating from efferent lymph will gradually be restored, precipitating T cell egress via the lymphatics (FIG. 1d). Return of T cells to lymph, or eventually blood, reverses this process, thus permitting continued recirculation. Although further validation is needed, the CCR7– S1P axis provides an elegant model of how T cells enter SLOs and spend an appropriate amount of time surveying DCs in the tissue before leaving to sample different lymph nodes for cognate antigen22. Inflammation and T cell activation. HEVs are unusual among post-capillary venules in that they support high levels of lymphocyte traffic under uninflamed conditions. However, inflammatory signals such as CCL2 and tumour necrosis factor (TNF), which are expressed either within inflamed (referred to as ‘reactive’) lymph nodes or within the tissues that they drain27–29, induce changes in lymph node architecture and homing requirements. These changes increase the probability of rare naive T cell interaction with cognate antigen and also allow recruitment of different T cell subsets and other leukocyte populations. For instance, local inflammation increases the size of the primary feed arteriole and microvascular circulation, which serve to hasten the rate of T cell entry into the affected lymph node30–34. Reactive lymph nodes induce CCR5 expression on populations of naive CD8+ T cells, which are subsequently drawn to local CCL3 and CCL4 gradients emanating from sites of DC and CD4+ T cell collaboration35,36. Similarly, early effector CD4+ T cells upregulate CXCR3 and localize to interfollicular and medullary zones in a CXC-chemokine ligand 10 (CXCL10)-dependent manner 37. Additionally, CXCL9 expression increases substantially within the HEVs of reactive nodes, resulting in the CD62L- and CCR7‑independent recruitment of CXCR3+ effector T cells38. Thus, lymph-node-homing rules are not static, but instead undergo dramatic changes under conditions of inflammation that optimize antigen sampling specifically at sites of pathogen exposure and also allow infected lymph nodes to serve as effector sites. In the rare event that a naive T cell encounters its cognate antigen within the SLO, developmental cues spur a dramatic series of events. Initial T cell receptor (TCR) activation elicits a transient upregulation in CCR7 and CD69 expression. CD69 prevents expression of S1PR1 at the cell surface39. This crucial event effectively increases the dwell time of recently activated T cells within the supportive environment of the SLO, which provides the essential instructional cues of antigen, co‑stimulation and cytokines to promote productive T cell proliferation40. After a few days, much of the expanded population leaves the T cell zone of the lymph node. There is evidence that T cells compete for antigen, and those that leave the lymph node first are of the lowest affinity, whereas those that compete more successfully for antigen stay longer and continue to proliferate41. This process may ensure that there is a rapid wave of effectors while also allowing the cells with optimal specificity to amplify the most. Migration to non-lymphoid tissues The imperative for migration. Proliferation signals that induce clonal expansion are coupled with differentiation and migration cues that coordinate function with localization. Some T cells may remain within the SLO; for example, CD4+ T follicular helper (TFH) cells upregulate CXCR5 and migrate to lymphoid follicles to provide B lymphocyte help42,43. However, most T cells exit the SLO to seek infected cells in the organism at large. Indeed, non-lymphoid tissues represent sites of infections for most pathogens. Unlike B cells, which can differentiate into plasma cells and exert effector functions from distant sites, T cells often need to make direct contact with antigen-bearing cells to exert their effector functions and contribute to infection control. Herein lies a fundamental problem; the human host comprises 1013 somatic cells that occupy approximately 70 litres in volume. By comparison, a resting lymphocyte has a volume of 290 femtolitres44, occupying only NATURE REVIEWS | IMMUNOLOGY VOLUME 13 | MAY 2013 | 311 © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS a b Sunlight DC Skin Activation stimulus c Dietary vitamin A Vitamin D metabolites Intestine Vitamin A metabolites Lymph node T cell Tissue factors ↑ CD69 ↑ CD103 ↓ CD122 ↓ CD127 ↓ LY6C Further T cell differentiation induced in tissue ↑ CCR10 ↑ CCR4 ↑ P- and E- ↑ α4β7 ↑ CCR9 selectin Homing potential is programmed by: • Tissue-specific cues • TCR stimulation strength • Inflammation in SLOs • Inflammation in peripheral tissues Figure 2 | Location dictates homing and differentiation in two discrete phases. a | The location of T cell priming influences the induction of peripheral homing molecules to the skin and small intestine. T cell activation in skin-draining Nature Reviews | Immunology secondary lymphoid organs (SLOs) preferentially programs the upregulation of skin homing molecules. Vitamin D metabolites, catalysed by sunlight, may contribute to this process by inducing CC‑chemokine receptor 10 (CCR10) expression. b | In the small intestine, dietary vitamin A metabolites are processed by αEβ7+ (also referred to as CD103+) dendritic cells (DCs) and delivered to T cells during activation in gut-draining SLOs, where they promote α4β7 integrin and CCR9 expression. c | After migrating to non-lymphoid tissues, a second round of developmental cues is provided by the tissue microenvironment itself. These factors, which have not been completely identified, modify effector and memory T cell differentiation in situ. TCR, T cell receptor. ~one one-hundred-trillionth of the organism. Although T cell proliferation increases the chance that antigen-specific T cell clones will locate cognate antigen, colocalizing effector T cells with infected host cells is the key biological challenge; increasing the probability of this interaction probably provided a major selective pressure in evolving the organization and design principles of the immune system. Multiple levels of trafficking regulation enable this interaction to occur, and to occur quickly. Area code hypothesis. It had long been suspected that T cells home preferentially to sites of infection45. The development of the multi-step homing paradigm provided a mechanistic basis for such tissue-selective homing. The combinatorial complexity of unique selectin, chemokine and integrin combinations that a multi-step homing model affords precipitated the hypothesis of organ-specific ‘area codes’, wherein each tissue could display a unique molecular signature required for entry 46. In support of this model, different homing molecules are required for migration to SLOs, gut and skin. On activation, most effector T cells downregulate CD62L and CCR7, and upregulate homing molecules that target them to non-lymphoid tissues rather than to SLOs. Remarkably, the expression of distinct homing programmes among effector T cells can be shown to reflect the site of priming. For example, T cells that undergo activation in gastrointestinal associated lymphoid tissue (GALT) preferentially upregulate α4β7 integrin and CCR9, which both have important roles in homing to the small intestinal mucosa47,48. This function is dependent on GALT stromal cells and the capacity of intestinal αEβ7+ (also referred to as CD103+) DCs to convert dietary vitamin A metabolites to retinoic acid, which in turn induces the expression of gut-homing molecules on activated lymphocytes49–52. By contrast, T cells that are activated within the skin-draining inguinal lymph nodes preferentially upregulate functional E‑selectin and P‑selectin ligands as well as CCR4 and/or CCR10, which are associated with homing to skin53–57. Interestingly, evidence suggests that vitamin D metabolites, which are induced by exposure to sunlight and are overrepresented in skin, induce CCR10 while suppressing gut homing 58 (FIG. 2a). These profound discoveries provide a mechanistic explanation for how the site of T cell priming could program homing to local non-lymphoid tissues. 312 | MAY 2013 | VOLUME 13 www.nature.com/reviews/immunol © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS Limits of the tissue-specific homing model. The transformative paradigm that T cell priming in specific inductive sites results in a homing programme that is biased to support trafficking to associated non-lymphoid tissues has substantial and elegant experimental support and teleological appeal12,59. However, this paradigm was never intended to be rigid. Tissue entry requirements are rarely absolute, regulation of non-lymphoid homing is multi-factorial and there is abundant evidence that effector T cells seed uninfected tissues. Indeed, tissue entry requirements vary by context. For instance, one study demonstrated that in vitro primed effector T cell migration to the small intestine was stringently dependent on CCR9 expression. However, when T cells were primed in vivo, there was significant intestinal homing that occurred independently of CCR9 (REF. 60). To add to this complexity, an intraperitoneal route of immunization exhibited less CCR9‑dependence than oral immunization for homing to the small intestine60. Thus, in vivo priming is complicated and observations do not always conform to predicted outcomes of a simplified programmed homing model. Moreover, there are multiple levels of regulation for effector T cell accumulation within tissues. For instance, secondary encounters with antigen after effector cells have already migrated into a non-lymphoid tissue may affect continued division, survival or retention61,62. Antigen dose and strength of stimulation may affect the induction of tissue-homing molecules63,64. And inflamed tissues promote effector T cell recruitment independently of priming site65. Indeed, exogenous application of CXCR3 ligands, which are broadly recognized by effector T cells, is sufficient to recruit effectors into the mouse lung or female reproductive tract 66,67. Additional evidence suggests that early effector T cells migrate between SLOs before entering tissues, indicating that they may be subject to homing cues from several different lymphoid environments68. Interestingly, most early effector CD8+ T cells isolated from murine spleen transiently express α4β7 after systemic infections or even upon local infections outside the gut 68–70. Similar observations were made in human peripheral blood following subcutaneous vaccination with the yellow fever vaccine YFV‑17D70. In fact, many studies have demonstrated that extraintestinal infections or immunization routes result in the establishment of antigen-specific CD8+ T cells within the small intestine or otherwise demonstrate that effector T cells disseminate broadly 68–76. In summary, the oft-quoted conclusion that infection of a particular tissue is absolutely required to elicit local effector T cell migration may not always be true. That said, the evidence for the induction of tissue-specific homing programmes within distinct SLO environments is unequivocal, and there is certainly compelling in vivo evidence for biased homing in relation to immunization route. It is likely that the degree to which T cell trafficking is promiscuous as opposed to specifically directed will vary considerably depending on the context of antigen priming and perhaps even among CD8+ and CD4+ T cells. Promiscuous homing may also vary among tissues, with skin and the central nervous system (CNS) perhaps being particularly selective. The challenge moving forward will be to define the rules and then apply this knowledge to optimize vaccination strategies that achieve the establishment of T cell responses in the appropriate locations. Action in non-lymphoid tissues. Effector T cells migrate to non-lymphoid tissues to seek cognate antigen, and this requires that they interact with large populations of host cells. Two-photon microscopy is a tremendously powerful tool that allows dynamic imaging of T cell responses in living animals77. Although early two-photon microscopy studies focused on SLOs, this technology is increasingly being applied to many non-lymphoid tissues, including pancreas, brain, skin, liver, intestine, lung and even the beating heart in order to visualize immune responses in vivo in real time61,78–83. Initial studies have already revealed tantalizing new insights into effector T cell behaviour in non-lymphoid tissues. For example, intravital imaging confirmed that after migration into the CNS, effector T cells that recognize cognate antigen undergo division in situ61. Hunter and colleagues recently demonstrated that unlike naive T cells in SLOs84, effector T cells do not patrol brain via Brownian walks in a murine Toxoplasma gondii infection model85. Rather, they randomly scan in patterns known as Lévy walks, which cover more territory (FIG. 3a). This strategy is used by a number of animals, including marine predators, birds and monkeys, to increase foraging efficiency. The presence of CXCL10 within the inflamed brain increased the T cell motility rate, but did not alter this migration pattern. However, crucial questions remain unanswered. For instance, how many effector T cells are needed to survey each and every host cell within a given time frame? How might these numerical requirements vary between different organs and during different states of inflammation and infection, and even under different effector T cell modes of action? In this light, the few measurements available for effector T cell motility in non-lymphoid tissues indicate that their movement is not particularly fast; being measured at ~4–10 μm min–1 (REFS 79,85,86). One study modelled the cytotoxic T lymphocyte (CTL) concentration required to eliminate a fast-growing tumour and arrived at the startling conclusion that >3 × 106 antigen-specific CTLs per gram of tumour were required to mediate tumour regression87. Recent data suggest that CD4+ T cells can be remarkably more efficient. In a Leishmania sp. infection model, Bousso and colleagues demonstrated that effector CD4+ T cells could signal infected phagocytes to upregulate inducible nitric oxide synthase (iNOS) and promote clearance of the infection as long as the phagocytes were within an 80 μm radius of an effector CD4+ T cell88. This function was dependent on interferon‑γ (FIG. 3b). Of course, more pathological T cell effector functions, such as cytolysis, depend on the specificity that a requirement for target cell contact provides. Other strategies, including the adoption of a dendritic morphology by T cells within skin epidermis, may increase the number of cell–cell contacts and the efficiency of immunosurveillance79,89 (FIG. 3c). NATURE REVIEWS | IMMUNOLOGY VOLUME 13 | MAY 2013 | 313 © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS b T cell a Phagocyte c Pathogen Migration pathway Skin Epithelial cell Brownian walk IFNγ Epidermis versus CD4+ T cell Lévy walk Infected phagocyte Resting memory T cell Figure 3 | Means by which T cells within non-lymphoid tissues increase their efficiency of immunosurveillance and pathogen control. a | Effector T cells scan infected brain via random Lévy walks (bottom pattern), which cover more Naturesuch Reviews | Immunology territory than Brownian walks (upper pattern)85. b | CD4+ T cells can extend some effector functions, as secreted interferon‑γ (IFNγ, in blue), far beyond the point of contact with an infected phagocyte. This contributes to the elimination of pathogen in target cells that were not in direct contact with effector CD4+ T cells88. c | Resting memory T cells have a dendritic morphology in the epidermis and simultaneously contact many epithelial cells79,89. Memory: homing begets differentiation Following the resolution of an infection, most effector T cells die, but a fraction of responding T cells differentiate into long-lived memory T cells. Unlike naive T cells, which have SLO-restricted homing patterns, antigen-experienced T cells exhibit a much broader anatomical distribution, being present in both SLOs and nonlymphoid tissues. Memory T cells also exhibit remarkable heterogeneity with respect to phenotype, differentiation and function; importantly, these parameters are associated with their migration patterns and associated anatomical locations. Central and effector memory. Historically, analyses of cell-mediated immune responses were biased towards populations of cells that can be easily harvested (that is, from venous blood) or that are present in high concentrations (that is, in SLOs). Secondary T cell responses were largely viewed as just a faster and more efficacious recapitulation of a primary immune response. It was thought that like primary immune responses, secondary immune responses were initiated in SLOs and depended on a period of proliferation before migration of the expanded effector T cell populations to sites of infection. Crucially, in this model T cells would not be immediately available to intercept pathogens at nonlymphoid tissue points of entry, where they are typically first encountered. Instead, memory T cells would be latecomers to non-lymphoid tissue sites of pathogen re‑exposure. In 1999, a pivotal study from Lanzavecchia and colleagues highlighted heterogeneity among memory CD4+ and CD8+ T cells isolated from human blood90. They conceptualized this heterogeneity by delineating memory T cells into two subsets: central and effector memory T cells (TCM cells and TEM cells, respectively). TCM cells were defined by the expression of lymph-node-homing molecules, and together with later studies, the data supported a model in which they exhibited the canonical memory T cell properties traditionally associated with anamnestic responses; like naive T cells, they recirculated through SLOs, possessed considerable capacity for interleukin‑2 (IL‑2) synthesis and proliferation upon TCR stimulation and, after several days of stimulation, gave rise to abundant effector T cells that migrated to sites of infection91,92. TEM cells were defined in blood by the absence of SLO-homing molecules, and thus putatively represented populations that recirculated through non-lymphoid tissues. Interestingly, many TEM cells constitutively maintained heightened effector-like functions (such as cytolytic activity among CD8+ T cells) that could be rapidly expressed without requiring a period of re‑differentiation. The great elegance of the TCM/TEM model was that it married functional specialization with T cell migration patterns and location. Innumerable studies have demonstrated that a surprisingly large proportion of both CD4+ and CD8+ memory T cells can be recovered from non-lymphoid tissues. Congruent with the TCM/TEM model, the pheno type and functional properties varied considerably between SLO and non-lymphoid tissue populations of memory T cells93,94. To emphasize this crucial theme, tissue location is often highly predictive of memory T cell phenotype irrespective of antigen-specificity and stimulation history 95,96. For example, virusspecific memory TCRαβ+ CD8αβ+ T cells isolated from the intestinal mucosa constitutively retain granzyme B expression and cytolytic activity after antigen clearance93,97. Moreover, they express low levels of CD127 (also known as IL‑7Rα) and CD122 (also known as 314 | MAY 2013 | VOLUME 13 www.nature.com/reviews/immunol © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS Immediate interception Who’s fighting the infection? Tissueresident TEM cell Migratory TEM cell Early response • In situ proliferation? • Recruitment? • Retention of migratory TEM cell? Delayed response Infected Progeny of tissue reactivated TCM cell Lymph node TCM cell Ignorant Proliferation Migration Figure 4 | Location dictates the rapidity by which memory T cells contribute to protection. Immediate pathogen interception can only be achieved by those memory T cells present in the tissue at the time of infection: namely resident Nature Reviews | Immunology and migrating subsets. If the infection is not immediately controlled, local responses may be rapidly augmented by in situ proliferation, retention and accumulation of recirculating memory T cells, and recruitment of resting memory T cells from blood after inflammation. Contemporaneously, central memory T (TCM) cells will be reactivated in draining secondary lymphoid organs and begin to proliferate and form a new wave of differentiated effectors. After several days, the effector cell daughters of reactivated TCM cells will migrate to the site of infection in great numbers, making a delayed but robust contribution to pathogen control. TEM cell, effector memory T cell. IL‑15Rβ), undergo little homeostatic cell turnover and exhibit limited proliferation upon reactivation98. Similar observations have been made for memory T cells in other non-lymphoid tissues, suggesting that TEM cells at the frontline are positioned to intercept pathogens at initial infection sites, where they can provide protection through immediate effector functions. By contrast, TCM cells, which populate SLOs that drain frontline tissue sites of infection, are best poised to regenerate abundant effector responses when needed, although such a response requires days of proliferation and re‑differentiation. Thus, the broad anatomical distribution of memory T cells and the coupling of function with location revealed that anamnestic responses occurred in anatomically and temporally distinct phases; a paradigm that provides a more complete explanation of T cell-dependent protective immunity 91,92,95,96,99 (FIG. 4). T EM cell recirculation. The interpretation that T EM cells were in equilibrium between blood and nonlymphoid tissues was consistent with early evidence suggesting that T cells re‑circulate between the two compartments. In sheep, memory-phenotype T cells were shown to be present in afferent lymphatics that drained peripheral tissues100,101, and in humans some memory T cells in blood constitutively express skinhoming molecules54; these findings are consistent with a model of constitutive tissue ingress and egress45. To test the regulation of egress, T cells were injected into mouse footpad or lung. Paradoxically, recovery of these cells from afferent lymphatics was CCR7 dependent 102,103. As CCR7 expression is the cardinal signature of TCM cells, and TCM cells do not exhibit non-lymphoid tissue homing characteristics by definition, it is difficult to conceptualize this observation. Nevertheless, these findings do not appear to be an artefact of the transfer system, as a large fraction of CD4+ and CD8+ T cells isolated from skin-draining afferent lymphatics in sheep do indeed express CCR7 (REF. 102). Thus, some observations are inconsistent with the predictions of the TCM/TEM model. TEM cell diversity and limits of the two-subset model. It has become increasingly clear that a model of a single recirculating TEM cell subset fails to capture the phenotypical and functional diversity of memory T cells in non-lymphoid tissues. For instance, CD8+ TEM cells in the gut express a panoply of markers that are not present on memory T cells isolated from the blood. This can be explained by several studies using tissue grafting, intravascular memory T cell transfers and/or parabiosis that indicate that memory T cells can be long-term residents in many non-lymphoid tissues, including the small intestine, skin, brain, lung and salivary glands62,70,104–108. These data support a model whereby effector T cells migrate to non-lymphoid tissues, where they then differentiate in situ while establishing residence without continued recirculation and without representation in peripheral blood70. Interestingly, the tissue microenvironment plays a crucial part in the induction of a tissue-specific pheno type post-migration. To illustrate this concept, local production of transforming growth factor‑β (TGFβ) induces αEβ7 integrin expression on T cells after their migration to the small intestinal epithelium (αE is also NATURE REVIEWS | IMMUNOLOGY VOLUME 13 | MAY 2013 | 315 © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS referred to as CD103). This αEβ7 induction is required for local T cell maintenance, putatively by binding E‑cadherin on epithelium97,109. So whereas the SLO priming environment partially regulates T cell migration to a tissue, once there the tissue provides developmental cues to fine tune compartment-specific T cell differentiation; a process that putatively optimizes local adaptive immunity (FIG. 2b). Each tissue is likely to induce distinct differentiation programmes62,98,105,110,111, balancing the need for site-specific protective immunity while preserving organ homeostasis. However, certain signatures do seem common to at least a portion of memory CD8+ T cells established in many tissues, including enhanced expression of CD69, αEβ7 and granzyme B, and diminished expression of IL‑7Rα and IL‑15Rβ62,65,97,104–108,110,112,113. Although CD69 expression occurs transiently on TCR stimulation, this activation marker is maintained in many non-lymphoid tissues without the requirement for constitutive cognate antigen recognition65,97,110. CD69 regulates S1P responsiveness, and S1P has been implicated in regulating T cell egress not only from SLOs but also from non-lymphoid tissues114. Thus, it is appealing to propose that CD69 could be a marker of tissue residence, although this remains to be validated more stringently. The field must now discriminate between recirculating and resident TEM cell subsets. Recent studies showed that memory CD8+ T cells in the epidermis were relatively sessile, whereas memory CD4+ T cells recirculated through the dermis79,115. Previous ovine studies found that most T cells in the hindlimb draining afferent lymphatics were CD4+ T cells100,116, suggesting that CD4+ T cells recirculate more frequently through peripheral tissues than do CD8+ T cells. However, CD4+ T cells within the mouse lung can be resident (and, interestingly, they remain imprinted with lunghoming potential if removed)107. Furthermore, circulating memory CD8+ T cells accumulate in the small intestinal lamina propria in a β7 integrin-dependent process117. These data indicate the presence of both resident and recirculating CD4+ and CD8+ T cells, and hint that recirculation may be defined by anatomical compartment (that is, epithelium versus stroma) rather than by T cell lineage. Box 1 | Complexity of non-lymphoid tissues Non-lymphoid tissues are not just ‘bags of cells’ that exist outside lymphoid organs. Rather, each organ exhibits a unique cell-type composition, organization and function, and a single organ comprises many distinct tissue types and structures (FIG. 5). Localization within an organ has an important bearing on T cell recirculation, residence and location-specific differentiation. Approaches that depend on lymphocyte isolations and subsequent ex vivo analyses (for example, flow cytometry-based or enzyme-linked immunosorbent spot (ELISPOT) assays) may contain cells that were present in various immunologically distinct compartments, including lamina propria, blood, lymph, tertiary lymphoid aggregates and various types of epithelial surfaces (FIG. 6). To more fully appreciate T cell immunobiology in non-lymphoid tissues, we will have to consider not only the organ of origin but also the tissue compartment within an organ. Although challenging, this goal may be facilitated by the development of new technologies such as histo-cytometry, a technique that blends the quantitative aspects of flow cytometry with the localization data from microscopy128. This raises the importance of appreciating the fine architecture of tissues. Enzymatic methods for isolating and studying tissue lymphocytes literally homogenize what may be several discrete populations that occupy epithelium and stroma, as well as lymphoid aggregates, tertiary lymphoid organs, blood and lymphatic vessels and, in many cases, SLOs (BOX 1; FIGS 5,6). Also, every tissue is unique. As a cautionary tale, up to 95% (depending on the context) of memory T cells isolated from the lung were shown to actually be in the microvasculature, despite perfusion118 (FIG. 6). Restricting analysis to tissue cells, which are protected from intravascular staining, will give clearer insight into T cell homing, differentiation and contributions to local protective immunity. Likewise, most T cells in liver are within sinusoids, which is contiguous with blood. However, to complicate matters, intravascular sinusoidal and lung microvasculature residence has been documented for natural killer T (NKT) cells119–121. So, it is possible that blood may be anatomically heterogeneous and may contain resident and recirculating subsets. The original definition of a TEM cell has been complicated by the vast location-dependent heterogeneity and the distinct migratory patterns of what may be more precisely described as a collection of several distinct subsets122. Further refinement is needed to embrace the more recently discovered complexity. Anamnestic responses: the primacy of location T cells require contact with antigen-bearing cells for triggering effector functions. Infections are typically initiated at body surfaces, particularly mucosal tissues. If pathogens are not immediately contained at the site of entry, pathogen-derived antigens subsequently drain to SLOs. Accordingly, T cell location dictates how quickly they may contribute to protective immune responses (FIG. 4). For immediate target interception, T cells need to be pre-positioned at the site of infection. Initial responders only include resident memory T cells and those migrating T cells that happen to be present within the tissue at the time of infection. In support of this concept, the presence of local resident memory T cells in mice greatly accelerated pathogen clearance in two skin challenge models104,105. Similar observations have been made in lung 107. Thus, vaccines will need to establish memory T cells in tissues if very rapid T cell-mediated control of the infection is the goal, such as may be the case for HIV, malaria and tuberculosis vaccines. Infections induce inflammation, changes in vascular addressin expression and permeability, and upregulation of chemokine responses in tissues. Although this is driven by the innate immune system, a recent report indicates that chemokine induction is potentiated by in situ reactivation of CD4+ memory T cells123. Topical application of CXCL9 and CXCL10 to the lumen of the female reproductive tract in mice recruited other T cells, although this was limited to effector T cells that had already been activated in SLOs67. However, there is evidence that memory T cells can be recruited to sites of inflammation before antigen-specific reactivation. This 316 | MAY 2013 | VOLUME 13 www.nature.com/reviews/immunol © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS occurs in the lung airways in response to local influenza infection, in the dorsal root ganglia in response to latent virus reactivation, and in the skin in response to a local hypersensitivity reaction79,124,125. Interestingly, if cognate antigen is recognized in the tissue, recruited memory T cells may initiate proliferation in situ125. It will be important to define the role that memory (not effector) T cell migration to sites of inflammation has in accelerating pathogen control. If not immediately contained within a non-lymphoid tissue site of initial exposure, antigen drains via afferent lymphatics, where it may then be recognized by memory T cells in downstream SLOs. Such recognition recapitulates the cardinal features of a primary immune response (albeit more quickly), characterized by T cell proliferation, differentiation and upregulation of peripheral homing molecules. These processes take several days but eventually result in a numerically robust tissue-directed effector immune response (FIG. 4). To conclude, the rapidity by which memory T cells help to control infectious re‑challenges in tissues is crucially dependent on their anatomical location92. Antigen and pathogen sampling M cell Type I epithelium Lamina propria Type II epithelium MALT Basement membrane Afferent lymph Capillary Efferent lymph TCM cell Resident TEM cell Naive Migratory TEM cell Lymph node Figure 5 | Tissue architecture considerations for T cell trafficking, subsets and Nature Reviews | Immunology analyses of isolated populations. An idealized tissue prototype illustrates several compartments. Epithelium is organized into monolayers (type I) or is stratified (type II). Mucosal type I epithelial surfaces are often associated with mucosal-associated lymphoid tissue (MALT). The term MALT is frequently misused129, but only refers to lymphoid structures that lack afferent lymphatics and sample antigens directly from the lumen of mucosal tissues via M (microfold) cells. Epithelium is avascular and separated from connective tissue (referred to as stroma or lamina propria) that contains both blood and lymphatic vessels. Non-lymphoid tissues drain to lymph nodes via afferent lymphatics. Each compartment is populated by distinct T cell subsets with distinct functions and homing patterns. When T cells are isolated from tissue resections or biopsies, T cells are often pooled from several compartments before analysis, creating an additional source of heterogeneity. TCM cell, central memory T cell; TEM cell, effector memory T cell. Closing thoughts “What kind of music do you usually have here?” “Oh, we got both kinds. We got country and western.” The Blues Brothers (1980) The more I learn, the more I learn how little I know. Socrates (circa 400 BC) T cell homing is tightly regulated, and naive, effector and memory T cells exhibit a variety of migration patterns. Crucially, the regulation of migration is highly integrated with differentiation and function. However, this integration is not absolute, and antigen-experienced T cells exhibit a profound level of heterogeneity that we have in all likelihood only partly grasped. Challenges for the field include conceptualizing this diversity while understanding what it is good for, how it is regulated and how to manipulate it. Moreover, it is still unclear to what degree distinct memory T cell populations cooperate during re‑infection. Is diversity good or will one memory T cell subset rule them all? Rational pursuit of these questions will require accepted and precise definitions. In this, the field has struggled in the past by attributing a broad range of biological properties (for example, homing, proliferation, cytokine expression profiles, surface phenotype and lytic activity) to either TCM or TEM cells122. Different investigators use different criteria. However, these properties are not always coordinately regulated and cannot be used as synonyms for the same cell type. For example, expression of CD62L (the most common marker used to define TCM cells in the mouse) can be dissociated from proliferation potential126. Likewise, lack of CD62L expression (one defining signature of TEM cells) does not always predict maintenance of lytic activity among memory CD8+ T cells (another defining signature of TEM cells)93. Cells that recirculate through non-lymphoid tissues express CCR7 upon exit; are these TCM or TEM cells? This imprecision of definitions has produced what some have referred to as the Tower of Babel127. We are not all speaking the same language. The field is now at a crossroads, as we have newfound appreciation for additional memory T cell diversity. This carries the risk of creating additional confusion but also the opportunity to bring clarity by judiciously applying appropriate definitions for T cell subsets. As T cell location is antecedent to antigen-recognition, and thus adaptive immune function, the field may be wise to maintain the spirit of the original TCM/TEM paradigm: viewing T cell classification through the prism of migration before all other considerations. In this scheme, TCM cells have a single exact definition: they possess the capacity to migrate across HEVs under homeostatic (uninflamed) conditions, whereas TEM cells do not. Importantly, this biological definition can be inferred on the basis of phenotype. Unfortunately this nomenclature is not the way the field is headed, and we are poised to add to the ambiguity. For example, resident memory T cells have now widely been referred to as ‘TRM cells’ (and we ourselves have used this term). There are two questions worthy of reflection before the field settles on this new convention: NATURE REVIEWS | IMMUNOLOGY VOLUME 13 | MAY 2013 | 317 © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS a b c Vagina Cervix iBALT * Epithelium Isolated lymphoid follicle 100 µm 100 µm * Uterus Vascular memory CD8+ T cell Lamina propria 100 µm Ovary * * IEL 100 µm 100 µm 20 µm 100 µm Figure 6 | Anatomic compartmentalization of representative tissues where T cells may be sampled. a | Lymphocytes sampled from the intestinal mucosa may include those from epithelium, lamina propria and mucosal-associated Nature Reviews lymphoid | Immunology tissue (MALT). Isolated lymphoid follicle is pictured; >100 isolated lymphoid follicles exist in the mouse large intestine and terminal ileum. MALT and blood can be contaminating sources of naive T cell and central memory T (TCM) cell preparations from various non-lymphoid tissues. b | For example, lung may contain inducible broncho-associated lymphoid tissue (iBALT), which contains high endothelial venules (HEVs) and naive lymphocytes (top panel, red = CD3, blue = B220, green = epithelium). Lung is also heavily vascularized and T cells are not completely removed by perfusion. The bottom panel illustrates a vascular memory CD8+ T cell labelled via intravascular staining (cyan) and a CD8+ intraepithelial lymphocyte (IEL) protected from intravascular staining (blue). Red = epithelium. c | Even a single organ can be quite heterogeneous. For example, in the vagina and ectocervix the epithelium is stratified squamous, in the uterus it is simple columnar and in the ovary it is cuboidal (‘*’ marks epithelium). Stromal composition and density also vary among compartments. These complexities are likely to affect differentiation and maintenance requirements, recirculation patterns and function. White = DAPI and red = collagen IV. how will we view the past, and how will we conceptualize the future? If we divorce TRM cells from the TEM cell canon and anoint them as a completely new subset, will this bring clarity to the many past studies that described properties of non-recirculating memory T cells but referred to them as TEM cells? Or will this create additional confusion, particularly for those outside the immediate field of memory T cell ‘subsetology’? And what will it mean to be neither a TCM nor a TRM cell? Those cells that remain catalogued under TEM are still quite heterogeneous and poorly defined transcriptionally. Will we continue to parse them into completely new ‘lineages’ with entirely new labels? If so, what will it mean in the future to be a TEM cell? We would argue that the literature and concepts will be more accessible if we maintain the TCM and TEM dichotomy, with each defined precisely as indicated above. One could claim that central and effector are inadequate descriptors that carry undesired connotations. Indeed, as the definition of TEM has evolved, it no longer exclusively refers to memory cells that maintain potent effector functions. Likewise, many TCM cells rapidly produce effector cytokines and even precipitate Obar, J. J., Khanna, K. M. & Lefrançois, L. Endogenous naive CD8+ T cell precursor frequency regulates primary and memory responses to infection. Immunity 28, 859–869 (2008). 2.Moon, J. J. et al. Naive CD4+ T cell frequency varies for different epitopes and predicts repertoire diversity and response magnitude. Immunity 27, 203–213 (2007). 3. Gowans, J. L. The effect of the continuous re‑infusion of lymph and lymphocytes on the output of lymphocytes 1. 4. 5. 6. killing of certain antigen-bearing host cells, and thus express important effector functions. But it may be far too late to rebrand these populations with more specific designations (for example, as THEV+ and THEV– cells) without massive consensus and cooperation among those that publish in this domain. At this juncture, as new subsets emerge they could be placed appropriately into the TCM and TEM taxonomy. Using migration as the primary guiding principle, one might imagine that we will describe resident TEM cells (those cells that exhibit little or no recirculation), migrating TEM cells (which routinely enter and leave tissues) and other subsets (perhaps there are lymph-node-recirculating populations of TCM cells that express stem-cell-like qualities, or TEM cell populations that enter neither non-lymphoid tissues nor SLOs under homeostatic conditions). This nomenclature is compatible with the literature of the past (which only bifurcated memory T cells into TCM and TEM subsets) yet remains flexible enough for the future classification of emerging or more refined subsets. It has the potential to be precise, and it defers to the primacy that the location of a T cell has in the execution of its functions. from the thoracic duct of unanaesthetized rats. Br. J. Exp. Pathol. 38, 67–78 (1957). Gowans, J. L. & Knight, E. J. The route of re‑circulation of lymphocytes in the rat. Proc. R. Soc. Lond. B. 159, 257–282 (1964). Whaler, B. C. & Widdicombe, J. G. The blood life-span of the lymphocyte in rabbits and rats. J. Physiol. 132. 41–42 (1956). Gowans, J. L. The recirculation of lymphocytes from blood to lymph in the rat. J. Physiol. 146, 54–69 (1959). 318 | MAY 2013 | VOLUME 13 7.Mandl, J. N. et al. Quantification of lymph node transit times reveals differences in antigen surveillance strategies of naïve CD4+ and CD8+ T cells. Proc. Natl Acad. Sci. USA 38, 263–274 (2012). 8. Gallatin, W. M., Weissman, I. L. & Butcher, E. C. A cell-surface molecule involved in organ-specific homing of lymphocytes. Nature 304, 30–34 (1983). 9. Rosen, S. D. Ligands for L‑selectin: homing, inflammation, and beyond. Annu. Rev. Immunol. 22, 129–156 (2004). www.nature.com/reviews/immunol © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS 10.Bao, X. et al. Endothelial heparan sulfate controls chemokine presentation in recruitment of lymphocytes and dendritic cells to lymph nodes. Immunity 33, 817–829 (2010). 11. Andrian, von, U. H. & Mempel, T. R. Homing and cellular traffic in lymph nodes. Nature Rev. Immunol. 3, 867–878 (2003). 12. Andrian, von, U. H. & Mackay, C. R. T‑cell function and migration. Two sides of the same coin. N. Engl. J. Med. 343, 1020–1034 (2000). 13. Bargatze, R. F., Jutila, M. A. & Butcher, E. C. Distinct roles of L‑selectin and integrins α4β7 and LFA‑1 in lymphocyte homing to Peyer’s patch-HEV in situ: The multistep model confirmed and refined. Immunity 3, 99–108 (1995). 14.Scimone, M. L. et al. CXCL12 mediates CCR7‑independent homing of central memory cells, but not naive T cells, in peripheral lymph nodes. J. Exp. Med. 199, 1113–1120 (2004). 15.Okada, T. et al. Chemokine requirements for B cell entry to lymph nodes and Peyer’s patches. J. Exp. Med. 196, 65–75 (2002). 16.Hargreaves, D. C. et al. A coordinated change in chemokine responsiveness guides plasma cell movements. J. Exp. Med. 194, 45–56 (2001). 17.Braun, A. et al. Afferent lymph-derived T cells and DCs use different chemokine receptor CCR7‑dependent routes for entry into the lymph node and intranodal migration. Nature Immunol. 12, 879–887 (2011). 18. Kaiser, A. A., Donnadieu, E. E., Abastado, J.‑P. J., Trautmann, A. A. & Nardin, A. A. CC chemokine ligand 19 secreted by mature dendritic cells increases naive T cell scanning behavior and their response to rare cognate antigen. J. Immunol. 175, 2349–2356 (2005). 19. Bousso, P. & Robey, E. Dynamics of CD 8+ T cell priming by dendritic cells in intact lymph nodes. Nature Immunol. 4, 579–585 (2003). 20.Lo, C. G. et al. Cyclical modulation of sphingosine1‑phosphate receptor 1 surface expression during lymphocyte recirculation and relationship to lymphoid organ transit. J. Exp. Med. 201, 291–301 (2005). 21. Arnon, T. I., Xu, Y., Lo, C., Pham, T. & An, J. GRK2‑Dependent S1PR1 desensitization is required for lymphocytes to overcome their attraction to blood. Science 333, 1898–1903 (2011). 22. Cyster, J. G. & Schwab, S. R. Sphingosine-1‑phosphate and lymphocyte egress from lymphoid organs. Annu. Rev. Immunol. 30, 69–94 (2012). 23. Rosen, H., Sanna, M. G., Cahalan, S. M. & Gonzalez-Cabrera, P. J. Tipping the gatekeeper: S1P regulation of endothelial barrier function. Trends Immunol. 28, 102–107 (2007). 24. Bardi, G. G., Lipp, M. M., Baggiolini, M. M. & Loetscher, P. P. The T cell chemokine receptor CCR7 is internalized on stimulation with ELC, but not with SLC. Eur. J. Immunol. 31, 3291–3297 (2001). 25.Kohout, T. A. T. et al. Differential desensitization, receptor phosphorylation, beta-arrestin recruitment, and ERK1/2 activation by the two endogenous ligands for the CC chemokine receptor 7. J. Biol. Chem. 279, 23214–23222 (2004). 26. Zidar, D. A., Violin, J. D., Whalen, E. J. & Lefkowitz, R. J. Selective engagement of G protein coupled receptor kinases (GRKs) encodes distinct functions of biased ligands. Proc. Natl Acad. Sci. USA 106, 9649–9654 (2009). 27.Palframan, R. T. et al. Inflammatory chemokine transport and presentation in HEV: a remote control mechanism for monocyte recruitment to lymph nodes in inflamed tissues. J. Exp. Med. 194, 1361–1373 (2001). 28.McLachlan, J. B. et al. Mast cell-derived tumor necrosis factor induces hypertrophy of draining lymph nodes during infection. Nature Immunol. 4, 1199–1205 (2003). 29.Janatpour, M. J. et al. Tumor necrosis factordependent segmental control of MIG expression by high endothelial venules in inflamed lymph nodes regulates monocyte recruitment. J. Exp. Med. 194, 1375–1384 (2001). 30.Webster, B. et al. Regulation of lymph node vascular growth by dendritic cells. J. Exp. Med. 203, 1903–1913 (2006). 31.Soderberg, K. A. et al. Innate control of adaptive immunity via remodeling of lymph node feed arteriole. Proc. Natl Acad. Sci. USA 102, 16315–16320 (2012). 32. Hay, J. B. & Hobbs, B. B. The flow of blood to lymph nodes and its relation to lymphocyte traffic and the immune response. J. Exp. Med. 145, 31–44 (2012). 33. Steeber, D. A., Erickson, C. M., Hodde, K. C. & Albrecht, R. M. Vascular changes in popliteal lymph nodes due to antigen challenge in normal and lethally irradiated mice. Scann. Microsc. 1, 831–839 (1987). 34. Cahill, R. N., Frost, H. & Trnka, Z. The effects of antigen on the migration of recirculating lymphocytes through single lymph nodes. J. Exp. Med. 143, 870–888 (1976). 35.Castellino, F. et al. Chemokines enhance immunity by guiding naive CD8+ T cells to sites of CD4+ T cell– dendritic cell interaction. Nature 440, 890–895 (2006). 36.Hickman, H. D. et al. Chemokines control naive CD8+ T cell selection of optimal lymph node antigen presenting cells. J. Exp. Med. 208, 2511–2524 (2011). 37.Groom, J. R. et al. CXCR3 chemokine receptor-ligand interactions in the lymph node optimize CD4+ T helper 1 cell differentiation. Immunity 37, 1091–1103 (2012). References 35–37 demonstrate the highly orchestrated localization of T cells to interfollicular and medullary zones within lymph nodes in response to antigen challenge. 38.Guarda, G. et al. L‑selectin-negative CCR7− effector and memory CD8+ T cells enter reactive lymph nodes and kill dendritic cells. Nature Immunol. 8, 743–752 (2007). This study demonstrates that migration into reactive lymph nodes is transiently CD62L and CCR7 independent. 39.Shiow, L. R. et al. CD69 acts downstream of interferon-alpha/beta to inhibit S1P1 and lymphocyte egress from lymphoid organs. Nature 440, 540–544 (2006). 40.Mescher, M. F. et al. Signals required for programming effector and memory development by CD8+ T cells. Immunol. Rev. 211, 81–92 (2006). 41. Zehn, D., Lee, S. Y. & Bevan, M. J. Complete but curtailed T‑cell response to very low-affinity antigen. Nature 458, 211–214 (2009). 42. Ma, C. S., Deenick, E. K., Batten, M. & Tangye, S. G. The origins, function, and regulation of T follicular helper cells. J. Exp. Med. 209, 1241–1253 (2012). 43.León, B. et al. Regulation of TH2 development by CXCR5+ dendritic cells and lymphotoxin-expressing B cells. Nature Immunol. 13, 681–690 (2012). 44. Segel, G. B., Cokelet, G. R. & Lichtman, M. A. The measurement of lymphocyte volume: importance of reference particle deformability and counting solution tonicity. Blood 57, 894–899 (1981). 45. Butcher, E. C. & Picker, L. J. Lymphocyte homing and homeostasis. Science 272, 60–66 (1996). 46. Springer, T. A. Traffic signals for lymphocyte recirculation and leukocyte emigration: the multistep paradigm. Cell 76, 301–314 (1994). 47. Salmi, M. & Jalkanen, S. Lymphocyte homing to the gut: attraction, adhesion, and commitment. Immunol. Rev. 206, 100–113 (2005). 48. Johansson-Lindbom, B. & Agace, W. W. Generation of gut-homing T cells and their localization to the small intestinal mucosa. Immunol. Rev. 215, 226–242 (2007). 49.Iwata, M. et al. Retinoic acid imprints gut-homing specificity on T cells. Immunity 21, 527–538 (2004). This paper defined a mechanism for imprinting T cells with tissue-specific homing. 50.Johansson-Lindbom, B. et al. Functional specialization of gut CD103+ dendritic cells in the regulation of tissue-selective T cell homing. J. Exp. Med. 202, 1063–1073 (2005). 51. Stagg, A. J., Kamm, M. A. & Knight, S. C. Intestinal dendritic cells increase T cell expression of α4β7 integrin. Eur. J. Immunol. 32, 1445–1454 (2002). 52.Hammerschmidt, S. I. et al. Stromal mesenteric lymph node cells are essential for the generation of guthoming T cells in vivo. J. Exp. Med. 205, 2483–2490 (2008). 53.Austrup, F. et al. P− and E‑selectin mediate recruitment of T‑helper‑1 but not T‑helper‑2 cells into inflamed tissues. Nature 385, 81–83 (1997). 54.Picker, L. J. et al. Control of lymphocyte recirculation in man. II. Differential regulation of the cutaneous lymphocyte-associated antigen, a tissue-selective homing receptor for skin-homing T cells. J. Immunol. 150, 1122–1136 (1993). 55. Reiss, Y., Proudfoot, A. E., Power, C. A., Campbell, J. J. & Butcher, E. C. CC chemokine receptor (CCR)4 and the CCR10 ligand cutaneous T cell-attracting chemokine (CTACK) in lymphocyte trafficking to inflamed skin. J. Exp. Med. 194, 1541–1547 (2001). NATURE REVIEWS | IMMUNOLOGY 56. Campbell, D. J. & Butcher, E. C. Rapid acquisition of tissue-specific homing phenotypes by CD4+ T cells activated in cutaneous or mucosal lymphoid tissues. J. Exp. Med. 195, 135 (2002). 57. Sigmundsdottir, H. & Butcher, E. C. Environmental cues, dendritic cells and the programming of tissueselective lymphocyte trafficking. Nature Immunol. 9, 981–987 (2008). 58.Sigmundsdottir, H. et al. DCs metabolize sunlightinduced vitamin D3 to ‘program’ T cell attraction to the epidermal chemokine CCL27. Nature Immunol. 8, 285–293 (2007). 59. Kunkel, E. J. & Butcher, E. C. Chemokines and the tissue-specific migration of lymphocytes. Immunity 16, 1–4 (2002). 60. Stenstad, H., Svensson, M., Cucak, H., Kotarsky, K. & Agace, W. W. Differential homing mechanisms regulate regionalized effector CD8αβ+ T cell accumulation within the small intestine. Proc. Natl Acad. Sci. USA 104, 10122–10127 (2007). 61.Kang, S. S. et al. Migration of cytotoxic lymphocytes in cell cycle permits local MHC I‑dependent control of division at sites of viral infection. J. Exp. Med. 208, 747–759 (2011). 62. Wakim, L. M., Woodward-Davis, A. & Bevan, M. J. Memory T cells persisting within the brain after local infection show functional adaptations to their tissue of residence. Proc. Natl Acad. Sci. USA 107, 17872–17879 (2010). 63.Svensson, M. et al. Retinoic acid receptor signaling levels and antigen dose regulate gut homing receptor expression on CD8+ T cells. Mucosal Immunol. 1, 38–48 (2008). 64.Román, E. et al. CD4 effector T cell subsets in the response to influenza: heterogeneity, migration, and function. J. Exp. Med. 196, 957–968 (2002). 65.Mackay, L. K. et al. Long-lived epithelial immunity by tissue-resident memory T (TRM) cells in the absence of persisting local antigen presentation. Proc. Natl Acad. Sci. USA 109, 7037–7042 (2012). 66. Campanella, G. S. V., Medoff, B. D., Manice, L. A., Colvin, R. A. & Luster, A. D. Development of a novel chemokine-mediated in vivo T cell recruitment assay. J. Immunol. Methods 331, 127–139 (2008). 67. Shin, H. & Iwasaki, A. A vaccine strategy that protects against genital herpes by establishing local memory T cells. Nature 491, 463–467 (2012). 68. Liu, L., Fuhlbrigge, R. C., Karibian, K., Tian, T. & Kupper, T. S. Dynamic programming of CD8+ T cell trafficking after live viral immunization. Immunity 25, 511–520 (2006). 69.Masopust, D. et al. Activated primary and memory CD8 T cells migrate to nonlymphoid tissues regardless of site of activation or tissue of origin. J. Immunol. 172, 4875 (2004). 70.Masopust, D. et al. Dynamic T cell migration program provides resident memory within intestinal epithelium. J. Exp. Med. 207, 553–564 (2010). 71.Kaufman, D. R. et al. Trafficking of antigen-specific CD8+ T lymphocytes to mucosal surfaces following intramuscular vaccination. J. Immunol. 181, 4188–4198 (2008). 72.Stevceva, L. et al. Both mucosal and systemic routes of immunization with the live, attenuated NYVAC/ simian immunodeficiency virus SIV(gpe) recombinant vaccine result in gag-specific CD8+ T‑cell responses in mucosal tissues of macaques. J. Virol. 76, 11659–11676 (2002). 73.Li, H. et al. Durable mucosal simian immunodeficiency virus-specific effector memory T lymphocyte responses elicited by recombinant adenovirus vectors in rhesus monkeys. J. Virol. 85, 11007–11015 (2011). 74. Belyakov, I. M., Hammond, S. A., Ahlers, J. D., Glenn, G. M. & Berzofsky, J. A. Transcutaneous immunization induces mucosal CTLs and protective immunity by migration of primed skin dendritic cells. J. Clin. Invest. 113, 998–1007 (2004). 75.Marshall, D. R. et al. Measuring the diaspora for virusspecific CD8+ T cells. Proc. Natl Acad. Sci. USA 98, 6313–6318 (2001). 76.Agrewala, J. N. et al. Unique ability of activated CD4+ T cells but not rested effectors to migrate to non-lymphoid sites in the absence of inflammation. J. Biol. Chem. 282, 6106–6115 (2007). 77. Coombes, J. L. & Robey, E. A. Dynamic imaging of host-pathogen interactions in vivo. Nature Rev. Immunol. 10, 353–364 (2010). 78.Fife, B. T. et al. Interactions between PD‑1 and PD‑L1 promote tolerance by blocking the TCR-induced stop signal. Nature Immunol. 10, 1185–1192 (2009). VOLUME 13 | MAY 2013 | 319 © 2013 Macmillan Publishers Limited. All rights reserved REVIEWS 79.Gebhardt, T. et al. Different patterns of peripheral migration by memory CD4+ and CD8+ T cells. Nature 477, 216–219 (2011). This study identified both recirculating and resident memory T cell populations within the skin, and showed that migration behaviour varied between the dermis and epidermis. 80.Egen, J. G. et al. Intravital imaging reveals limited antigen presentation and T cell effector function in mycobacterial granulomas. Immunity 34, 807–819 (2011). 81.McDole, J. R. et al. Goblet cells deliver luminal antigen to CD103+ dendritic cells in the small intestine. Nature 483, 345–349 (2012). 82.Looney, M. R. et al. Stabilized imaging of immune surveillance in the mouse lung. Nature Methods 8, 91–96 (2010). 83.Li, W. et al. Intravital 2‑photon imaging of leukocyte trafficking in beating heart. J. Clin. Invest. 122, 2499–2508 (2012). References 82 and 83 apply intravital two‑photon microscopy to visualize leukocyte motility within the lung and the heart. 84. Miller, M. J., Wei, S. H., Parker, I. & Cahalan, M. D. Two-photon imaging of lymphocyte motility and antigen response in intact lymph node. Science 296, 1869–1873 (2002). 85.Harris, T. H. et al. Generalized Lévy walks and the role of chemokines in migration of effector CD8+ T cells. Nature 486, 545–548 (2012). References 85 and 88 show various strategies that increase the efficiency of pathogen immunosurveillance or control by effector T cells within non-lymphoid tissues. 86. Boissonnas, A., Fetler, L., Zeelenberg, I. S., Hugues, S. & Amigorena, S. In vivo imaging of cytotoxic T cell infiltration and elimination of a solid tumor. J. Exp. Med. 204, 345–356 (2007). 87.Budhu, S. et al. CD8+ T cell concentration determines their efficiency in killing cognate antigen-expressing syngeneic mammalian cells in vitro and in mouse tissues. J. Exp. Med. 207, 223–235 (2010). 88. Eberl, G., Aebischer, T., Späth, G. F. & Bousso, P. CD4+ T cells rely on a cytokine gradient to control intracellular pathogens beyond sites of antigen presentation. Immunity 37, 147–157 (2012). 89.Ariotti, S. et al. Tissue-resident memory CD8+ T cells continuously patrol skin epithelia to quickly recognize local antigen. Proc. Natl Acad. Sci. USA 109, 19739–19744 (2012). 90. Sallusto, F., Lenig, D., Forster, R., Lipp, M. & Lanzavecchia, A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401, 708–712 (1999). This study was the first to parse memory T cells into TCM and TEM cells. 91. Sallusto, F., Geginat, J. & Lanzavecchia, A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu. Rev. Immunol. 22, 745–763 (2004). 92. Masopust, D. & Picker, L. J. Hidden memories: frontline memory t cells and early pathogen interception. J. Immunol. 188, 5811–5817 (2012). 93. Masopust, D., Vezys, V., Marzo, A. L. & Lefrançois, L. Preferential localization of effector memory cells in nonlymphoid tissue. Science 291, 2413–2417 (2001). 94. Reinhardt, R. L., Khoruts, A., Merica, R., Zell, T. & Jenkins, M. K. Visualizing the generation of memory CD4 T cells in the whole body. Nature 410, 101–105 (2001). 95. Lefrançois, L. & Puddington, L. Intestinal and pulmonary mucosal T cells: local heroes fight to maintain the status quo. Annu. Rev. Immunol. 24, 681–704 (2006). 96. Woodland, D. L. & Kohlmeier, J. E. Migration, maintenance and recall of memory T cells in peripheral tissues. Nature Rev. Immunol. 9, 153–161 (2009). 97.Casey, K. A. et al. Antigen-independent differentiation and maintenance of effector-like resident memory T cells in tissues. J. Immunol. 188, 4866–4875 (2012). 98. Masopust, D., Vezys, V., Wherry, E. J., Barber, D. L. & Ahmed, R. Cutting edge: gut microenvironment promotes differentiation of a unique memory CD8 T cell population. J. Immunol. 176, 2079–2083 (2006). This study showed that the tissue microenvironment influences T cell differentiation in situ. 99. Gebhardt, T., Mueller, S. N., Heath, W. R. & Carbone, F. R. Peripheral tissue surveillance and residency by memory T cells. Trends Immunol. 34, 27–32 (2013). 100.Mackay, C. R., Marston, W. L. & Dudler, L. Naive and memory T cells show distinct pathways of lymphocyte recirculation. J. Exp. Med. 171, 801–817 (1990). 101.Abitorabi, M. A. et al. Differential expression of homing molecules on recirculating lymphocytes from sheep gut, peripheral, and lung lymph. J. Immunol. 156, 3111–3117 (1996). 102.Debes, G. F. et al. Chemokine receptor CCR7 required for T lymphocyte exit from peripheral tissues. Nature Immunol. 6, 889–894 (2005). 103.Bromley, S. K., Thomas, S. Y. & Luster, A. D. Chemokine receptor CCR7 guides T cell exit from peripheral tissues and entry into afferent lymphatics. Nature Immunol. 6, 895–901 (2005). References 102 and 103 provide evidence that T cell egress from non-lymphoid tissues is regulated by CCR7. 104.Gebhardt, T. et al. Memory T cells in nonlymphoid tissue that provide enhanced local immunity during infection with herpes simplex virus. Nature Immunol. 10, 524–530 (2009). 105.Jiang, X. et al. Skin infection generates non-migratory memory CD8+ TRM cells providing global skin immunity. Nature 483, 227–231 (2012). 106.Hofmann, M. & Pircher, H. E‑cadherin promotes accumulation of a unique memory CD8 T‑cell population in murine salivary glands. Proc. Natl Acad. Sci. USA 108, 16741–16746 (2011). 107.Teijaro, J. R. et al. Cutting edge: tissue-retentive lung memory CD4 T cells mediate optimal protection to respiratory virus infection. J. Immunol. 187, 5510–5514 (2011). References 104, 105 and 107 show that resident TEM cells positioned within non-lymphoid tissues accelerate pathogen control upon local re‑infection. 108.Lee, Y. T. et al. Environmental and antigen receptorderived signals support sustained surveillance of the lungs by pathogen-specific cytotoxic T lymphocytes. J. Virol. 85, 4085–4094 (2011). 109.El‑Asady, R. et al. TGF-β-dependent CD103 expression by CD8+ T cells promotes selective destruction of the host intestinal epithelium during graft-versus-host disease. J. Exp. Med. 201, 1647–1657 (2005). 110. Kohlmeier, J. E., Miller, S. C. & Woodland, D. L. Cutting edge: antigen is not required for the activation and maintenance of virus-specific memory CD8+ T cells in the lung airways. J. Immunol. 178, 4721 (2007). 111.McCully, M. L. et al. Epidermis instructs skin homing receptor expression in human T cells. Blood 120, 4591–4598 (2012). 112.Sathaliyawala, T. et al. Distribution and compartmentalization of human circulating and tissue-resident memory T cell subsets. Immunity 38, 1–11 (2012). 113.Wakim, L. M. et al. The molecular signature of tissue resident memory CD8 T cells isolated from the brain. J. Immunol. 189, 3267–3268 (2012). 114.Ledgerwood, L. G. et al. The sphingosine 1‑phosphate receptor 1 causes tissue retention by inhibiting the entry of peripheral tissue T lymphocytes into afferent lymphatics. Nature Immunol. 9, 42–53 (2008). 115. Bromley, S. K., Yan, S., Tomura, M., Kanagawa, O. & Luster, A. D. Recirculating memory T cells are a unique subset of CD4+ T cells with a distinct phenotype and migratory pattern. J. Immunol. 190, 970–976 (2013). 320 | MAY 2013 | VOLUME 13 116. Abernethy, N. J., Hay, J. B., Kimpton, W. G., Washington, E. & Cahill, R. N. Lymphocyte subsetspecific and tissue-specific lymphocyte-endothelial cell recognition mechanisms independently direct the recirculation of lymphocytes from blood to lymph in sheep. Immunology 72, 239–245 (1991). 117.Klonowski, K. D. et al. Dynamics of blood-borne CD8 memory T cell migration in vivo. Immunity 20, 551–562 (2004). 118.Anderson, K. G. et al. Cutting edge: intravascular staining redefines lung CD8 T cell responses. J. Immunol. 189, 2702–2706 (2012). 119.Thomas, S. Y. et al. PLZF induces an intravascular surveillance program mediated by long-lived LFA‑1– ICAM‑1 interactions. J. Exp. Med. 208, 1179–1188 (2011). 120.Geissmann, F. et al. Intravascular immune surveillance by CXCR6+ NKT cells patrolling liver sinusoids. PLoS Biol. 3, e113 (2005). 121.Scanlon, S. T. et al. Airborne lipid antigens mobilize resident intravascular NKT cells to induce allergic airway inflammation. J. Exp. Med. 208, 2113–2124 (2011). 122.Jameson, S. C. & Masopust, D. Diversity in T cell memory: an embarrassment of riches. Immunity 31, 859–871 (2009). 123.Strutt, T. M. et al. Memory CD4+ T cells induce innate responses independently of pathogen. Nature Med. 16, 558–564 (2010). 124.Ely, K. H. et al. Nonspecific recruitment of memory CD8+ T cells to the lung airways during respiratory virus infections. J. Immunol. 170, 1423–1429 (2003). 125.Wakim, L. M., Gebhardt, T., Heath, W. R. & Carbone, F. R. Cutting edge: local recall responses by memory T cells newly recruited to peripheral nonlymphoid tissues. J. Immunol. 181, 5837–5841 (2008). 126.Hikono, H. et al. Activation phenotype, rather than central- or effector-memory phenotype, predicts the recall efficacy of memory CD8+ T cells. J. Exp. Med. 204, 1625–1636 (2007). 127.Rocha, B. & Tanchot, C. The Tower of Babel of CD8+ T‑cell memory: known facts, deserted roads, muddy waters, and possible dead ends. Immunol. Rev. 211, 182–196 (2006). 128.Gerner, M. Y., Kastenmuller, W., Ifrim, I., Kabat, J. & Germain, R. N. Histo-cytometry: a method for highly multiplex quantitative tissue imaging analysis applied to dendritic cell subset microanatomy in lymph nodes. Immunity 37, 364–376 (2012). This report describes an approach for gathering the cellular positioning information of histological analyses with the quantitative power of flow cytometry. 129.Brandtzaeg, P., Kiyono, H., Pabst, R. & Russell, M. W. Terminology: nomenclature of mucosa-associated lymphoid tissue. Mucosal Immunol. 1, 31–37 (2008). Acknowledgements The authors thank V. Vezys and S. Jameson (University of Minnesota) for helpful discussion. This study was supported by U S N a t i o n a l I n s t i t u t e s o f H e a l t h ( N I H ) g ra n t R01AI084913‑01 (to D.M.), NIH grant T32AI007313 (to J.M.S.) and the Office Of The Director, NIH, under Award Number DP2OD006467 (to D.M.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Competing interests statement The authors declare no competing financial interests. FURTHER INFORMATION David Masopust’s homepage: http://masopustvezyslabs.umn.edu/Welcome.html ALL LINKS ARE ACTIVE IN THE ONLINE PDF www.nature.com/reviews/immunol © 2013 Macmillan Publishers Limited. All rights reserved