* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Sports concussion management in the South African environment
History of neuroimaging wikipedia , lookup
Holonomic brain theory wikipedia , lookup
Neurobiological effects of physical exercise wikipedia , lookup
Cognitive flexibility wikipedia , lookup
Process tracing wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neuropsychology wikipedia , lookup
Aging brain wikipedia , lookup
Mental chronometry wikipedia , lookup
Clinical decision support system wikipedia , lookup
Cognitive interview wikipedia , lookup
Neurophilosophy wikipedia , lookup
Cognitive psychology wikipedia , lookup
Cognitive science wikipedia , lookup
Cognitive neuroscience wikipedia , lookup
Psychological evaluation wikipedia , lookup
Embodied cognitive science wikipedia , lookup
Impact of health on intelligence wikipedia , lookup
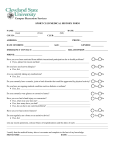
Sports concussion management in the South African environment Dr Jon Patricios Sports Physician, Johannesburg Director of Sports Concussion South Africa IRB, SA Rugby and BokSmart Concussion Consultant Introduction Together with the rest of the sporting world, South Africa has followed a decade-long evolution in clinical evaluation and care of the concussed athletes. Moreover, with the collision sport of rugby union accounting for by far the largest number of cases of concussion, we have adapted our protocols to reach the diverse populations playing this sport, intertwine clinical know-how with grassroots education of the public, coaches and referees and make the clinical assessment template more comprehensive. Definition The modern expanded definition of concussion as “a trauma-induced, complex patho-physiological alteration in brain function” that emphasises a wide array of possible clinical manifestations and highlights microscopic and physiological brain changes rather than gross structural abnormality, has remained intact since the first international conference on concussion in sport in Vienna, 2001. Indeed it is this broad descriptive terminology that dictates a multifaceted and serial clinical approach to the concussed athlete. The South African approach to concussion management takes its lead from the consensus documents that have emerged since then, most recently from the 2008 Zurich meeting and can be classified into the following categories: Education Fieldside care Initial clinical assessment Follow-up clinical assessments Return-to-play Education There is a drive internationally to better educate the sports-participating public as well as clinicians as to the significance of recognising concussion and the importance of following best clinical practice guidelines. Public education programmes make use of media campaigns (e.g. “Sports Concussion Awareness Week” on radio), public and school lectures and the internet (www.sportsconcussion.co.za). Most importantly educational drives are closely linked with the South African Rugby Union’s BokSmart injury-prevention campaign that aims to limit all but especially serious and catastrophic rugby injuries by targeting rugby referees and coaches. Educational posters, pocket concussion cards and pamphlets that summarise best concussion practice are freely available to schools and clubs and all protocols are fully described on the BokSmart website pages applying to concussion (www.boksmart.com). In addition free advice and emergency transport for head and spine-injured athletes is available from the 24 hour Spineline 0800-678678, as well as training for first aiders through the “Rugby Medics” programme. All rugby referees and coaches at any level from Springbok to primary school have to undergo a 2-yearly BokSmart certification course. The purpose of this multifaceted educational and intervention process is the early identification and appropriate referral of concussed players so as to prevent the potentially serious sequelae of head injury including intra-cranial haemorrhage, diffuse cerebral oedema or “second impact syndrome” which most often occur with mismanagement in the early stages of injury. Fieldside care Any player that loses consciousness, has neck pain or associated neurological symptoms should be treated as a neck injury, implying head and neck stabilisation and stretchering off the field. Facilitation of appropriate field side care medical or paramedical care is guided by the Pocket Field side Sports Concussion Assessment Tool (SCAT) card. The South African version of the field side card that emerged from the Zurich consensus meeting contains the following information: 1. 2. 3. 4. Identification of concussion using Simple memory function testing in the form of modified Maddock’s questions (on-field questions devised by a neuropsychologist to distinguish significant concussion) Common early symptoms and signs of concussion; “Do’s and don’ts” for the concussed athlete Identification of “Red Flags” that may indicate more serious or rapidly progressing pathology. Contact details for local emergency departments and sports concussion clinics Athletes identified as having possibly suffered a concussion should be removed from the field and receive further evaluation as soon as possible. Initial clinical evaluation The Sports Concussion Assessment Tool version 3 (SCAT3) emerged from the Zurich consensus meeting as the template best-suited to evaluate the concussed athlete. The SCAT3 (http://www.sportsconcussion.co.za/Pharos/Protocols.php) is designed for use by medical and paramedical personnel and includes the following important information: Educational information on the definition and significance of concussion Epidemiological information A symptom analysis and score Scores for: Glasgow Coma Scale Physical signs Verbal cognitive assessment Balance Athlete “Red Flag” information Athlete advice More recently (2011) the SCAT has become available as an iPad and iPhone application improving fieldside functionality. The South African experience is that the SCAT3 is appropriate for acute concussion assessment but that a more comprehensive tool is needed to facilitate record and guide complete concussion care. Serial follow-up clinical evaluation Following acute assessment and management of the concussed athlete, the next phase is the most essential in facilitating timely return-to-play for which the following criteria must be met: The athlete must be asymptomatic The neurological (including verbal cognitive and balance) examination must be normal Computerised cognitive tests must have returned to baseline or be equivalent to age-appropriate norms. An asymptomatic exercise stress test must have been completed. In our experience, the SCAT3 is inadequate to be used as a template for this more extensive assessment phase and there is a trend away from over-reliance on computerised cognitive tools which are most-appropriately interpreted as part of a thorough clinical evaluation. This has led to the creation of the Sports Concussion Office Assessment Tool (SCOAT) designed to facilitate continuity with SCAT3 but provide a more comprehensive template to serially monitor the resolution of sports concussion. In essence this template is designed to: Be used serially by clinicians in a consulting room environment Evolve from the SCAT3 by retaining the important features relevant to acute, subacute and subsequent presentations Exclude those aspects of SCAT3 only relevant to the field side assessment of concussion Follow the Zurich consensus guidelines as closely as possible Simplify the scoring system to one that tends towards zero before returning to play Aid as a tool for further research. SCOAT excludes those aspects of the SCAT3 only relevant to the most acute phase of concussion, duplicates the parts relevant in ongoing serial assessments, incorporates more features of significance to the concussed athlete and simplifies the scoring system. Instructions It is assumed that clinicians using the SCOAT are familiar with modern concussion management and many of the detailed instructions included in SCAT3 have been omitted. Epidemiological data These are expanded upon from the SCAT3 with the addition of “position played” and the “mechanism of injury” both of which may be relevant in epidemiological data capture. Loss of consciousness (LOC) and, in particular, amnesia are specifically recorded. Rather than an emphasis on the presence and duration of LOC which heavily influenced previous grading scales and RTP, amnesia is now acknowledged as the more significant acute marker of injury severity and duration. “Red Flags” As a reminder to clinicians that more serious intra-cranial pathology may mimic concussion particularly in the early stages of presentation, those symptoms that may indicate a need for neuroimaging and neurosurgical referral are afforded more prominence than in the SCAT3. Compliance record We have found that patient recovery is often influenced by compliance to the advice given. For example: Was a concussed child kept from school? Did he/she avoid unnecessary forms of cognitive stress (computer games; texting etc.)? Were all forms of physical exertion avoided? Failure to adequately comply may explain slower progress and is therefore recorded; similarly, claims of good compliance in the face of a failure to clinically improve may be a poor prognostic sign. Modifying factors Several associations have been described in the literature between predisposition and prognosis and their influences on recovery and prognosis. It is most beneficial to document such features as a qualitative record that may significantly influence player management. Symptom analysis One of the most influential determinants of clinical progress is the progression of symptom resolution. The SCOAT retains the same 22 symptoms as SCAT3 and the 7-point Likert scale form common to most concussion symptom scales but divides them into clusters to enable the clinician to more efficiently monitor trends in both presentation (i.e. are the manifestations of injury more physical, cognitive, emotional or sleep-related?) and resolution. Verbal Cognitive Assessment The clinical cognitive assessment (cognitive assessment, immediate memory, concentration and delayed recall) as described and validated in the Standardised Assessment Concussion is left almost unchanged from SCAT3. Of note however, is that SCOAT uses a modified scoring system where incorrect answers are awarded 1 point. The purpose of this is to again create a “norm” of zero mistakes, the aggregate score in the recovering patient trending towards zero. Balance Assessment The validated Balance Error Scoring System (BESS) is left unchanged as is the awarding of a point for each error scored, again aiming for a “normal” score of zero. Examination As the SCOAT is designed as a clinical evaluation form, space is afforded to clinical examination findings both general and neurological. Again a score of 1 point for any adverse finding is awarded as an acknowledgement that players should have a normal neurological examination before returning to sport. Computerised Cognitive Screening The trend in concussion evaluation is towards thorough and serial clinical assessments. However, the emergence of computerised cognitive test batteries has provided an additional validated tool enabling the clinician to evaluate changes in brain function particularly where a pre-injury baseline score is available. Neuroimaging Because the manifestations of concussion are largely functional rather than structural, brain scans (CT or MRI) have specific indications. In those cases where imaging is warranted, the indication, type of scan and result are recorded on the SCOAT. Scoring system The maximum aggregate score is 200 and before returning to play the patient should ideally score zero meaning there are no symptoms, the examination is normal and the verbal cognitive, co-ordination and balance tasks were perfectly completed. In a fully recovered patient this may still not be possible where baseline measures of these parameters are not perfect, but we feel that zero provides a benchmark towards which all recovering concussed athletes should trend. Recommended Management The SCOAT provides a record of medications prescribed, referrals to colleagues and paperwork dispensed. Checklist The final block is a checklist of those factors most highlighted in the consensus statements and essential for ensuring that the athlete is recovered before returning to sport namely that they are asymptomatic, have a normal examination, the computerised cognitive screen has normalised and the return-to-play exercise protocol has been followed whilst acknowledging the influence of modifying factors. Conclusion South African sports concussion management guidelines follow international consensus whilst also customising both educational programmes and clinical protocols to strive for appropriate standardised best clinical practice in this country. The integration of best practice guidelines into the BokSmart injury prevention programme has facilitated a national footprint, whilst the dividing of the clinical approach into field side, acute and follow-up protocols has streamlined medical management. The SCOAT is a clinical tool designed to integrate all aspects of concussion care deemed to be essential. References available on request. All protocols referred to are available at: www.sportsconcussion.co.za and www.boksmart.com Pocket Fieldside Sports Concussion Assessment Tool (SCAT) Concussion should be suspected in the presence of any one or more of the following: symptoms (such as headache) or physical signs (such as unsteadiness) or impaired brain function (e.g. confusion, memory loss) or abnormal behaviour. 1. Memory function Failure to answer all questions correctly may suggest a concussion. “At what venue are we at today?” “Which half is it now?” “Who scored last in this game?” “Did your team win the last game?” 2. Symptoms Presence of any of the following signs & symptoms may suggest a concussion. Loss of consciousness Blurred vision Difficulty remembering Seizure or convulsion Balance problems Fatigue or low energy Amnesia Sensitivity to light Confusion Headache Sensitivity to noise Drowsiness “Pressure in head” Feeling slowed down More emotional Neck Pain Feeling like “in a fog“ Irritability Nausea or vomiting “Don’t feel right” Sadness Dizziness Difficulty concentrating Nervous or anxious Any athlete with a suspected concussion should be IMMEDIATELY REMOVED FROM PLAY, urgently assessed medically and should not be left alone. Important Advice: A doctor must assess you after suffering a suspected concussion. If concerned about the player’s condition, transfer immediately to an Emergency Department; if the player is lucid and stable, he/she may be monitored at home and should attend the Sports Concussion Clinic in the coming days. Note: a normal X-ray, CT or MRI brain scan does NOT exclude concussion. If referred home: Always make sure that you are in the presence of a responsible adult for 48 hours. Record and monitor the symptoms of concussion including headache, nausea, dizziness, fatigue, sleep disturbances, memory lapses, mood swings, poor concentration or any other feeling that concerns you. Complete rest & sleep will help recovery. Use only mild painkillers (e.g. Panado) for headaches DO NOT: Consume alcohol Study Take excessive amounts of painkillers(follow doctor’s Work at the computer orders) Place yourself in an environment of loud noise and excessive light Drive for 48 hours Exercise until re-evaluation by a doctor