* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular Lecture:
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Rheumatic fever wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Artificial heart valve wikipedia , lookup
Jatene procedure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
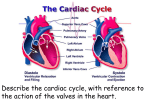
Circulatory System Lecture: Cardiovascular and lymphatic 1. Functions include: exchange & transportation 2. Cardiac Muscle Tissue revisited: uninucleate, branched, striated, intercalated disks are where two cells come together and join tightly like clasped fingers, and gap channels - allow ions to pass freely from cell to cell, resulting in rapid conduction of the exciting electrical impulse 3. Blood Vessel Structure: veins, arteries and capillaries 4. The Heart a. location and size: apex towards left hip base points to rt shoulder b. coverings and wall: pericardium (double sac of serous membranes) secrete serous fluid, visceral/ epicardium hugs external surface of heart @ apex: connects parietal pericardium from heart to diaphragm and sternum heart wall has 3 layers: 1. epicardium 2. myocardium: muscle 3. endocardium: lines cavity chambers of the heart and continues to vessels (think glistening sheet) c. chambers and associated vessels 4 chambers: 2 atria (receive blood) and 2 ventricles (pump blood out) rt atria receives blood from vena cava; lt atria receives blood from lungs rt side is pulmonary pump rt ventricle: most anterior surface left ventricle: apex lt side: systemic pump d. valves atrioventricular valves: AV prevent backflow into atria o left: bicuspid / mitral valve (two flaps or cusps of endocardium) o rt: tricuspid valve (3) chordae tendinae: anchor cusps to wall o semilunar valves (3 cusps fit tightly together) o when ventricles contract semilunar valves open and blood rushes through o Leaky valves: incompetent valve: heart repumps same blood o Valvular stenosis: valves become stiff (bacterial infection of myocardium) e. cardiac circulation o Coronary arteries feed the heart while the ventricles contract; branch out from the aorta down the atrioventricular groove o cardiac veins empty into coronary sinus and empties into right atrium o If heart rate increases (too rapid) myocardium may not receive enough blood (no oxygen) crushing chest pain = angina pectoris, if angina is prolonged then the ischemic heart cells die = infarct = myocardial infarct = coronary heart attack f. conduction physiology 2 types of control to regulate 1. ANS: para and sympathetic 2. intrinsic conduction system (nodal) o Tissue is muscle and nerve o Muscle depolarization is one way: atria to ventricle (75 beats per min) o Sinoatrial node (SA) pacemaker (on the rt atrium) has the highest rate of depolarization o Atrioventricular node (av node and bundle of his) o Rt and left branches (septum) o Purkinje fibers spread into ventricles walls o Heart block: AV node not under control of SA node and vetricles beat on their own o Ischemia: lackof blood supply toheart and leads to fibrillation (uncontrolled shuddering of theheart) looks like a bag of worms o Tachycardia: rapid heart beats > 100 per min o Bradycardia: < 60 beats per min g. Cardiac cycle/heart sounds o Systole (contraction) diastole ( relaxation) o Cardiac cycle: both atria and ventricles contract in 8 sec o 3 Periods: a. mid to late diastole: heart is relaxed, blood flows passively into atria and to ventricles from both circulatory systems - semilunar valves closed - AV valves opne - atria contract b. ventricular systole: ventricles contract, atria passively fill up with blood c. early diastole: ventricles are completely closed chambers o lub = closing of AV valves o dub = closing of semilunar valves o Murmurs: unusual heart sounds, indicate valve problems h. Cardiac output: (CO) regulation of stroke volume and heart rate o CO the amount of blood pumped out by each ventricle/ min The venous return o SV: volume of blood pumped out by each ventricle/ beat (pump out 60% of blood in heart) CO = SV X HR Ex. 5200 ml/min = 70 ml/beat X 75 beats /min o If SV is low then HR is high (weakened heart or low blood vol) o Starlings law: SV controlled by how much cardiac muscle cells are stretched depends on venous return Although heart rate is independent, the ANS, ions and hormones can modify heart rate. Sympathetic nerve can stimulate SA and AV node Parasympathetic or vagus nerve slows down/steadies heart Hormones: epinephrine (mimics sympathetic ) and thyroxine Ca+ is low: depresses heart Ca+ is high causes prolonged contractions (hypercalcemia) K+ is low causes feeble heart beat and abnormal rythms appear Congestive heart failure: pumping efficiency is low = inadequate blood to tissue, usually progressive by atherosclerosis Left side of heart fails: pulmonary congestion 5. Major Blood Vessels a. systemic circulation : body b. pulmonary circulation : lungs 6. Special circulation a. circulation of willis: surrounds base of brain: provides more than one route b. hepatic portal: veins: drain digestive organs, spleen and pancreas and deliver to liver through hepatic portal vein liver checks glucose etc.. liver is drained by hepatic veins and enters inferior vena cava c. fetal: shunt moves blood through septum in foramen ovale into LA, if blood gets to RVand pulmonary trunk meets 2nd shunt (ductus arteriosus) 7. Blood Pressure a. systolic b. diastolic c. what does it mean? 8. Lymphatic system a. organs: nodes, spleen, thymus gland, tonsil, peyers patches of intestines and lymphatic tissue scattered in ET b. vessels: rt lymphatic duct: drains rt arm, head and thorax; throcic duct : rest of body c. nodes 9.Monitoring EKG (electrocardiogram) a. graphical recording of the electrical events occurring within the heart b. 5 identifiable deflections: a. P wave: first waveform - depolarization of the atria b. Q,R,S complex is the next waveform: depolarization of the ventricles c. T wave: repolarization of the ventricles. Interpretation: By looking at time intervals between cardiac events and comparing them to standard values, one can determine if a person’s heart has sustained any damage that will alter the muscle cells ability to conduct an electrical signal. Ex. In first degree heart block, impulse propagation through the AV node is impeded, resulting in an abnormally long P-R interval. In order for a problem to be detected by an EKG, the disease must alter the cardiac muscle cell’s ability to conduct an impulse. Many diseases affect the heart without altering its electrical properties. A physical defect such as a faulty pulmonary or aortic valve is going to disturb the mechanical action of the heart, but not the electrical information that would show up on an EKG. The most common problems that can be diagnosed from an EKG are heart block, atrial fibrillation, and ventricular fibrillation. Ventricular fibrillation is the most severe and is often the result of a myocardial infarction or heart attack. During ventricular fibrillation, there is an abnormality in impulse conduction in the ventricles, resulting in continuous disorganized contractions inadequate to produce blood flow.