* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Curr.Med. Chem._Martínez, A._2015 - digital
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Orphan drug wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
NMDA receptor wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of direct Xa inhibitors wikipedia , lookup
Prescription costs wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Psychopharmacology wikipedia , lookup
Nicotinic agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Drug design wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Drug discovery wikipedia , lookup
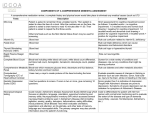
From bitopic inhibitors to multitarget drugs for the future treatment of Alzheimer’s disease Running title: From bitopic to multitarget Daniel I. Pérez, Ana Martínez, Carmen Gil* and Nuria E. Campillo* Centro de Investigaciones Biológicas (CIB-CSIC). C/ Ramiro de Maeztu 9, 28040 MadridSpain Correspondence: Dr. Nuria E. Campillo and Dr. Carmen Gil Centro de Investigaciones Biológicas (CIB-CSIC) C/ Ramiro de Maeztu 9, 28040 Madrid- Spain [email protected]; [email protected] Abstract Dementia is one of the main causes of the disease burden in developed regions. According to the World Health Organization (WHO), it will become the world’s second leading cause of death by the middle of the century, overtaking cancer. This will have a dramatic impact on medical care, and have important social and economic implications, unless more effective preventive procedures or treatments become available. Alzheimer’s disease (AD) is the most common cause of dementia, accounting for approximately 50–75% of all dementias worldwide, followed by vascular dementia, mixed dementia, and Lewy body dementia. Currently, acetylcholinesterase (AChE) inhibitors, such as donepezil, rivastigmine and galantamine are used to treat mild to moderate AD. An alternative therapy for severe AD is memantine, an antagonist of the NMDA-subtype of glutamate receptors. However, these drugs provide only temporary symptom improvement, and do not alter disease progression, except temporarily in some patients. In recent years different approaches have been developed to provide a more effective treatment for AD. These approached include the discovery of emerging targets and new drugs aiming at a single target, but given the complexity of the disease, different targets may need to be engaged simultaneously. New strategies have explored bitopic inhibitors, for example a single drug that acts on different sites of the acetylcholinesterase enzyme to produce at least two different activities, and multitarget drugs that act on multiple therapeutic targets. In this review, we explore the journey from a bitopic inhibitor strategy to multitarget drugs for the future treatment of AD. Keywords: Alzheimer’s disease, bitopic drugs, multitarget, BACE-1, cannabinoids, GSK3β, AChE, BuChE 1. INTRODUCTION Dementia primarily affects older people, although there is growing awareness of cases that start before the age of 65. Exact estimates of the prevalence of dementia depend on the definition and specific diagnostic threshold used. The syndrome affects approximately 5–8% of individuals over age 65, 15–20% of individuals over age 75, and 25–50% of individuals over age 85. Alzheimer’s disease (AD) is the most common dementia, accounting for 50–75% of the total (Table 1), with a greater proportion in the higher age ranges. The remaining types of dementia account for a much smaller fraction of the total [1]. Table 1. Characteristics of the different dementias. Dementia Symtpoms Neuropathology Alzheimer’s disease - Marked memory loss, apthy and depression - Language difficulties - Cortical amyloid plaques, neuronal neurofibrillary tangles Vascular dementia - Smooth memory loss, mood fluctuations - Physical frailty - Cerebrovascular disease, Single infarct in critical regions Dementia with Lewy bodies - Marked fluctuation in cognitive ability - Hallucinations - Tremor and rigidity - Cortical Lewy bodies Frontotemporal dementia - Personality changes - Mood changes - Language difficulties - Degeneration of the frontal and temporal lobes % of dementia cases 50 –75% 20 –30% <5% 5 –10% AD was identified more than 100 years ago, but research into its symptoms, causes, risk factors and treatment has gained momentum only in the last 30 years. Although research has revealed a great deal about AD, much is yet to be discovered about the precise biologic changes that cause this neurological disorder, why it progresses at different rates among affected individuals, and how the disease can be prevented, slowed or stopped. AD is a neurodegenerative disorder characterized by an insidious onset that progresses in a complex, chronic, multi-factorial way, affecting hippocampus and frontal cortex (Fig. 1). The symptoms that characterize this disease are severe memory loss, decline in language skills, as well as other cognitive impairments, and dramatic behavioral changes. It is estimated that AD affects more than 4.5 million people in the US and 18 million worldwide [2]. The disease is characterized by neuropathological lesions manifested as protein deposits. They consist of neuritic plaques composed of extracellular deposits of beta-amyloid peptide (A plaques) and interneuronal tangles formed by neurofibres of coiled filaments of tau protein [3, 4]. Fig. (1). Main pathogenic hallmarks (red) and some of the current drug targets (blue) in AD. Figure adapated from references [5] and [6]. To date, the established treatments offer only symptomatic relief, aiming to counterbalance the neurotransmitter disturbance in the disease [7-9]. The marketed drugs can be grouped into two therapeutic strategies. The first is aimed at treating a cholinergic deficit. Choline acetyltransferase (ChAT) and acetylcholinesterase (AChE) are involved in the synthesis and degradation of acetylcholine, respectively. The observed reduction of this neurotransmitter in AD suggests a selective destruction of cholinergic neurons. The second strategy is treatment of glutamate-mediated neurotoxicity. Glutamate excitotoxicity mediated through excessive activation of N-methyl-D-Aspartate (NMDA) receptors is believed to play a role in the neuronal death observed in AD and other neurodegenerative conditions. Glutamate is the main excitatory neurotransmitter in the central nervous system and physiological levels of glutamate-receptor activity are essential for normal brain function [10, 11]. Generally speaking, all these medications are symptomatic therapies that do not cure the disease. There is a clear need for improved drugs. During the past two decades, drug discovery has mainly focused on the single-target paradigm (single keys for specific locks), in order to develop a drug with high potency and high selectivity of action. However, the traditional single-target approach provides limited success to treat complex and multifactorial diseases [12]. During recent decades, alternative strategies have been explored that ranged from bitopic drugs acting on different sites of the same target and producing at least two different activities [13-16] to multitarget drugs acting on different therapeutic targets [17-22]. These strategies are particulary suitable for complex diseases with multiple pathogenic factors, such as neurodegenerative disorders, cancers and cardiovascular diseases. The rationale behind these bitopic inhibitors together with their development of multitarget drugs is described. The main goal of this review is to describe the evolution from the first dual binding site AChE inhibitors to molecules where an AChE inhibitor is linked to other active compounds and finally to compounds able to interact simultaneously with two targets involved in AD. The importance of the multitarget strategy in complex diseases as neurodegenartive ones, especially Alzheimer disease, will be here described. 2. BITOPIC INHIBITION STRATEGY Since the cholinergic hypothesis of memory dysfunction was first reported, many efforts have been made in the discovery and development of different cholinergic drugs for the treatment of cognitive deficits. However, only AChE inhibitors are clinically approved drugs. Although they failed to address the wide variety of symptoms that characterize these disorders, the use of AChE inhibitors for AD palliative treatment lead to the discovery of non-cholinergic functions of the cholinergic enzyme AChE [23, 24]. Among others, AChE may work as a chaperone involved in the conformational change of A [25]. In fact, it was shown that AChE is able to promote A plaques in the cerebral cortex in transgenic models [26]. AChE chaperone activity is mediated by Trp 279 located in the entrance to the catalytic gorge, in the peripheral anionic site (PAS) of AChE [27, 28]. This discovery suggested the design of bitopic inhibitors that simultaneously modulate the catalytic (CAS) and peripheral sites (PAS) of AChE. The idea behind these bitopic compounds, also called dual binding site AChE inhibitors, is not only to slightly improve cognition by targeting the catalytic site of AChE, but also to interfere with disease progression by decreasing toxicity and/or aggregation of A [29]. In that way, compounds designed specifically to interact simultaneously with Trp 86 located in the CAS, and with Trp 279 in the PAS were proposed [30] (Fig. 2). Some years later, these compounds have been shown to induce not only an improvement in cognitive function but also cause a potent modulation of A pathology in animal models [31]. These data demonstrate that it is possible, at least in animal models, to modulate A pathology through targeting AChE [32]. Fig. (2). Cartoon depicting the two binding sites (CAS and PAS) of AChE and their function in the pathology of AD. The concept of a dual binding site or bitopic AChE inhibitor is also shown. Many different compounds have been designed and synthesized following this strategy [33]. In general, the pattern shows in Fig.3 is followed for the design of bitopic inhibitors. The design contains three different chemical features: a known and small AChE inhibitor to interact with the catalytic site, a linker of different length and nature located along the gorge of the enzyme, and a chemical framework able to interact efficiently in the peripheral site, mainly with the Trp 279 (Fig. 3). Common fragments used in these bitopic ligands to gain interaction with the catalytic site are tacrine, huperzine A, huprine (hybrid AChE inhibitor comprising chemical features from huperzine A and tacrine) [34], and benzylpiperidine (one of the privileged scaffolds present in donepezil) [35]. In regard to the linker, different polymethylene chains have been used to optimize the length for each compound class, although the introduction of an amide bond increases positive electrostatic interactions along the gorge, increasing the inhibitory potency of the compounds [36]. Polyamines have also been used frequently as biologically active spacers in these bitopic compounds [37]. Some hydrophobic interactions may be gained in this part of the molecule by using 1,4-disubstituted phenyl rings as spacers, such is the case for the dual binding site AChE inhibitor AP2238 [38]. Finally, the interaction in the peripheral site is usually achieved by taking advantage of the potential interaction between Trp 279 and the chemical scaffold present in the ligand. Thus, the better this interaction is, the more potency is gained by the inhibitor. The most potent compound reported until now is a dimer of 6-chlorotacrine and indol moiety, called NP-61, that has a picomolar inhibition potency on human AChE (IC50 = 70 pM), two orders of magnitude of selectivity regarding BuChE and great in vitro inhibition of AChE induced A aggregation (IC50 = 2 M) [39]. Chronic oral treatment with NP-61 in a hAPP transgenic model for three months lead to an increase in cognitive learning measured by the Morris water maze test, together with a decrease of the plaque load in both cortex and hippocampus [31]. These results suggest that NP-61 is a potent Aβ modulator able to reverse the AD-like neurodegenerative phenotype in transgenic mice, indicating that bitopic inhibitors or dual binding site AChE inhibitors are promising disease-modifying agents for clinical application. In fact, clinical trials in humans are needed to assess the efficacy of these new drugs in AD patients. Fig. (3). Structural schematic followed for the design of dual binding site AChE inhibitors. Chemical structure of AP2238 and NP-61. In the past decade, improvements in this field were focused on the development of new assays able to determine binding and inhibition at the peripheral AChE site [40]. Thus, thioflavin T was reported to be a more sensititve and versatile fluorescent reporter of ligand interactions with the PAS than propidium, the classical standard reference. Moreover, dual binding site AChE inhibitors have recently emerged as multitarget compounds by their general additional inhibition of BACE-1. Recently, a study of the structural motifs conveying this polypharmacological profile [41] pointed to the complementary shape of some chemical fragments with the big catalytic site of BACE-1. In addition, the synthetic methodology developed for coupling different AChE inhibitor fragments to other molecules has been applied to the design of multitarget compounds that simultaneously inhibit not only AChE but also other targets involved in AD pathology that are described in the following sections. It is also worthwhile to mention that new structural motifs in the N-terminal region of AChE recently have been identified as involved in Aβ aggregation, which may open up new directions for bitopic ligand design in the coming years [42]. Finally, the concept of bitopic drugs has been applied recently to a new generation of specific M1 muscarinic acetylcholine receptor (M1 mAChR) agonists[43]. The development of M1 mAChR-selective agents has been hampered until now by high orthosteric site sequence homology among the five muscarinic receptor subtypes, and the wide distribution of this receptor family in both the central nervous system (CNS) and the periphery. In recent months, a second generation of M1 mAChR-specific ligands able to bind simultaneously to the orthosteric site and the less structurally conserved allosteric site of the M1 mAChR have emerged[44]. This approach revealed a new future for this class of bitopic cholinergic drugs[13]. 3. MULTITARGET-DRUG STRATEGY The aim of a multitarget drug is to act selectively on multiple targets of therapeutic interest. Within the multitarget strategy it is possible to identify two categories of multitarget therapeutics [45], in one of them, the drug acts on two or more targets that can be within individual signalling pathways or across pathways within a cell. In the other one, the response of one target to a drug could modulate a different target. Different approaches toward multitarget drugs have been used during the last decade to fight against multifactorial diseases [19, 46, 47] with special emphasis in the neurodegenerative field, since many involve multiple targets with pathological functions in complex neurotoxic cascades [48-50]. Recent studies in the neurodegenerative field according to this strategy have led to the synthesis of several chemically diverse structures with dual or multiple biological profiles for the treatment of AD. The first group of compounds maintained the inhibition of a cholinergic enzyme such as AChE or butyrylcholinesterase (BuChE), but added different scaffolds to interact with BACE-1 and/or NMDA, CB2 or histamine H3 receptors [17, 50], while a second group have been designed with the aim of finding non-cholinergic drugs with combined activities such as metal chelator properties or tau kinase inhibition. 3.1. Drugs targeting both AChE and NMDA receptors Tacrine was the first drug approved for AD treatment (1993), followed by donepezil (1996), rivastigmine (2000) and galantamine (2001). Each of these are inhibitors of AChE, and produce an increase of acetylcholine neurotrasmission in the synaptic cleft, improving cognitive deficits in the early stages of AD. These AChE inhibitors together with the NMDA receptor antagonist memantine (2003), which regulates the activity of glutamate, an important neurotransmitter in the brain involved in learning and memory, represent the only palliative treatments for AD. In AD, excess glutamate can be released from damaged cells, leading to chronic overexposure to calcium, which can speed up cell damage. Memantine helps to prevent this destructive chain of events by partially blocking the NMDA receptors. Considering the efficacy of the multitarget ligand strategy [51], combination of these two therapeutic approaches could lead to a synergistic pharmacological outcome. However, there are different results in the literature regarding this synergistic effect. Multiple studies suggest combination therapy with memantine and an AChE inhibitor in moderate to severe AD produces consistent benefits beyond the effects of AChE inhibitor treatment alone [52, 53]. Nevertheless, in other trial, memantine did not show an advantage over placebo in patients with stable AChE inhibitor regimens [54]. Today, an investigation of the safety and effectiveness of donepezil and memantine combination therapy in patients with AD is ongoing (www.clinicaltrials.gov, NCT02162251). Additionally, a commercially available fixed-dose combination of controlled-release memantine and donepezil is on the market after the benefits provided in thinking, daily functioning, and behavior in people with moderate to severe AD were shown [52, 55, 56]. One of the main drawbacks to combining two drugs in the same formulation is the different pharmacokinetic, metabolism and bioavailability of the drugs. For this reason the multi-target drug ligand (MTDLs) design strategy consists on developing a single chemical compound which are able to modulate multiple targets simultaneously with superior efficacy and safety profiles [6]. Several multitarget ligands based on AChE inhibitors and NMDA antagonists have been reviewed recently [57]. The first hybrid molecule, called carbacrine (Fig. 4), was designed using a tacrine derivative (6-chlorotacrine) as the AChE inhibitor and carvedilol as the NMDA antagonist [58]. Carvedilol presents a privileged structure as a building block in the search for new rationally designed multitarget drugs for AD treatment. On one hand it has neuroprotective efficacy because of its modulatory action at NMDA receptors as a low-affinity antagonist [59] and on the other hand because it is an efficient inhibitor of A formation [60]. The synthesis of the carbacrine hybrid structure was done employing different linkers/spacers between the tacrine and carbazole in order to improve the interaction with the catalytic and peripheral anionic sites of AChE (Fig. 4) leading to a single compound with nanomolar AChE inhibition, efficient NMDA antagonism, and antioxidant and Aaggregation reducing properties. Fig. (4). Design of multitarget compounds with cholinergic activity and NMDA receptor antagonism. Another example is memagal (Fig. 4) that was designed employing galantamine (AChE inhibitor) and memantine (NMDA antagonist), taking into account the dual binding approach to reach the catalytic and peripheral sites of AChE [61]. It was reported that the combination of galantamine and memantine might provide a more effective treatment for memory impairment in cognitive disorders than either drug used alone [62]. From the series of compounds synthesized, the optimal spacer between the two molecules consisted of six methylene groups. Memagal was shown to be a nanomolar potency AChE inhibitor that also inhibited the induced NMDA neurotoxicity in neuroblastoma cells in the micromolar range. This neuroprotective effect of galantamine was shown by blocking the α7 and/or α4β2 nicotinic receptors [63]. Dimebon (latrepirdine) was reported to have micromolar inhibition of AChE (IC 50 = 42 µM) and NMDA receptor antagonism (IC50 = 10 µM) [64]. Although a preliminary clinical trial (www.clinicaltrials.gov, NCT00377715) reported that dimebon was safe, well-tolerated, and significantly improved the clinical course of patients with mild-to-moderate Alzheimer's disease [65], a more recent multinational phase III study showed no difference between the two drug-treated groups and the placebo group [66], probably because the brain concentration after acute oral administration was lower than necessary to affect AChE and NMDA [67]. In order to improve these activities, a bivalent ligand strategy was employed to design new dimebon derivatives. Two pharmacophoric groups were connected with a linker following the requirements of dual binding sites in AChE. Docking studies were carried out with the new derivatives, pointing out the importance of the γ-carboline moiety of dimebon for AChE recognition (Fig. 4). Dimebon derivatives in which the spacer was formed by 6 and 7 methylene groups showed improved AChE inhibition (<1 µM) while mainting the same NMDA receptor inhibition [68]. Additionally, these compounds were able to reduce Aβ aggregation at 50 µM between 37–73% whereas dimebon showed only 10% inhibition. Other AChE inhibitors and NMDA antagonist compounds have been described in the literature such as bis-7 tacrine [69, 70] and bivalent β-carbolines [71]. These compounds were tested as NMDA antagonists after the discovery of their AChE inhibition. 3.2. Drugs targeting both AChE and histamine H 3 receptors Another drug target combination that can promote a synergistic effect is AChE and histamine H3 receptor inhibition. Histamine H3 receptor inhibits histamine release in the brain and inhibits the release of other neurotransmitters such as acetylcholine, glutamate, serotonin, dopamine, etc. via a parallel role as a heteroreceptor [72]. Thus, blocking the central histamine H3 receptor will raise acetylcholine levels in the brain. Combining AChE inhibitors and histamine H3 receptor antagonists in a single molecule will enhance cholinergic neurotransmission in the cortex. There are several H3 receptor antagonists described in the literature, and the scaffold of compound JNJ-5207852 [73] was employed in the design of multitarget ligands for AChE inhibition/H3 receptor antagonism [74]. Tacrine displayed nanomolar affinity not only for AChE but also for histamine N-methyltransferase, therefore, the combination of the H3 receptor pharmacophore and an acridine-framework was originally proposed in 2002 [75]. The resulting multitarget drug, namely FUB 833 [75], displays nanomolar inhibition for AChE and for the H 3 receptor (human H3 Ki = 0.33 nM) (Fig. 5). Fig. (5). Different drug design strategies for simultaneous targeting of AChE and H3 receptors. New multitarget drugs were designed employing a series of novel non-imidazole H3 ligands from the chemical manipulation of 1,1’-octa-, -nona-, and -decamethylene-bis-piperidines—H3 antagonists with tacrine (Fig. 5). Within the compounds synthesized, the tetrahydroaminoacridine hybrid depicted in Fig. 5 stands out as one of the most attractive molecules, synergistically combining nanomolar potency and selective H3 antagonism (antagonist potency at human histamine H3 receptors expressed in SK-N-MC cells, human H3 pKB = 8.93) with remarkable AChE activity (pIC50 = 7.57) even more potent than that shown by the simple molecule of tacrine on rat brain cholinesterase (pIC50 = 6.54) [76]. A new family of dual AChE/H3 receptor inhibitor compounds was recently published. They were designed based on previous structure activity relationship studies on H 3 ligands [77, 78], which showed that phenol ethers in the meta position to the tertiary benzyl amine possess high antagonist potency at the H3 receptor (Fig. 5). Compound 1 [79], showed a nanomolar inhibition of AChE and was a human H3 receptor antagonist with Ki = 76.2 nM. There are other examples of AChE/H3 receptor inhibitors described in the literature synthesised using different methodologies such as the use of crystal structure, pharmacophore modelling and docking techniques that lead to the identification of an AChE inhibitor/H3 receptor antagonist [80], but they were found to inhibit these targets in a moderate way. 3.3. Drugs targeting AChE and having antioxidant properties Nowadays it is accepted that oxidative damage can be involved in the course of AD and can act as a risk factor for its initiation and progression [81]. Therefore, an antioxidant-based therapy could be a helpful approach to ameliorate the deleterious effects of oxidative stress in this disease. Moreover, the design of multitarget ligands able to combine cholinergic activities with antioxidant properties has been successfully tackled by different research groups. Although the clinical use of tacrine, the first approved drug for AD, has been restricted due to hepatotoxicity, it is widely used as a starting point in drug discovery programs. Thus several tacrine hybrids have been described in which the tacrine core is linked to another moiety with interesting properties [82]. Regarding bifunctional molecules with cholinergic and antioxidant properties, tacrine has been linked with well-known antioxidant scaffolds such as melatonin [83], clioquinol [84], flavonoids [85], quinone [86] or ferulic acid [87]. Melatonin is a neurohormone, whose levels decrease during aging, that has been reported to possess strong antioxidant actions and free radical scavenger properties [88]. The development of melatonintacrine hybrids (Fig. 6a) yields derivatives able to inhibit AChE in the sub-nanomolar to picomolar range that also have antioxidant properties [83]. As a matter of fact, the new hybrids show better AChE inhibitory and antioxidant properties than their separate structures, can cross the blood brain barrier (BBB) and display neuroprotective properties against cell death induced by various toxic insults in a human neuroblastoma cell line [89]. Fig. (6). Drug design strategies to generate compounds with AChE inhibition and antioxidant properties. Modulation of redox metal ions such as Cu and Fe has been proposed as a potential therapeutic strategy for the treatment of AD as a way to reduce the production of reactive oxygen species (ROS) and oxidative stress [90]. As clioquinol is a well-known metal chelator able to reduce oxidation and the A burden [91], it was selected to be combined with the tacrine scaffold to obtain hybrids of tacrine-8-hydroxyquinoline (Fig. 6a), which have been shown to have not only cholinergic, antioxidant and copper-complexing properties but also neuroprotective properties in damaged human neuroblastoma cells [84]. The flavonoids have well-recognised properties as free-radical scavengers [92] and also hybrids with tacrine have been described (Fig. 6a). The resulting molecules have proved to be not only efficient antioxidants and cholinergic agents, but also potent BACE-1 inhibitors [85]. The design strategy employed for the discovery of memoquin [93] (Fig. 6b) was based on the incorporation of a 1,4-benzoquinone functionality as a radical scavenger into the polyamide skeleton of a previously reported cholinergic derivative named caproctamine [94]. Memoquin is able to interfere with different key target points of AD neurodegeneration such as AChE, oxidative stress, BACE-1 and A aggregation, showing not only an interesting in vitro profile, but also suitable in vivo activity in animal models [95]. The memoquin scaffold also has been employed as a template for the design of new multitarget ligands [86, 96]. The AChE inhibitor AP2238 (Fig. 6c), was chosen to be hybridised with melatonin in order to obtain new potent cholinergic and antioxidant agents [97]. Additionally, these kinds of compounds have shown neurogenic properties, which adds significant value for their use in AD treatment. 3.4. Drugs targeting both AChE and BACE-1 Inhibition of AChE activity would alleviate clinical symptoms in short-term therapy, and inhibition of BACE-1 would have an additive effect by preventing the formation of Aβ and further slowing the progression of the long-term disease, since BACE-1 catalyzes the first and rate-limiting step of the biosynthesis of Aβ from the amyloid precursor protein (APP). This therapy likely may result in a comprehensive suppression of AD in a synergistic manner and obtain higher therapeutic effectiveness [98]. The first multitarget AChE/BACE-1 inhibitors were published by Piazzi et al. [99]. They reported a new amidic nonpeptidic derivative family in which the framework of AP2243, a dual binding site acetylcholinesterase inhibitor, was maintained, whereas the methoxy groups of the coumarin moiety were alternately substituted by an amidic chain to extend the activity to BACE-1. Therefore, they introduced halophenylalkylamidic functions in positions 6 or 7 of the coumarin moiety, choosing a dihalophenyl acid because this moiety emerged as a leitmotif in different BACE-1 inhibitors. Following this rationale, a new series of potential multi-target compounds was synthesized (Fig. 7). The most potent compound 2 exhibited an IC50 of 99 nM for BACE-1 and 7.16 M for human AChE. Fig. (7). Dual inhibitors of AChE and BACE-1. Zhu and co-workers [98] combined pharmacophores of AChE and BACE-1 inhibitors through a suitable common scaffold to develop a new family of multitarget compounds. As inhibitor of AChE they used the N-benzylpiperdine pharmacophoric group of donepezil and an isophthalamide fragment derived from a known BACE-1 inhibitor (3). These fragments are joined through a classic transition state isostere for aspartyl protease inhibitors such as statine, homostatine (HE), nostratine (HMC) and hydroxyethyl-amine (HEA) (Fig. 8). Fig.(8). a) Structure of known BACE-1 and AChE inhibitors. b) Structure of the linkers. c) Dual inhibitors of AChE and BACE-1. Of the three families developed based on the common framework, HE, HMC and HEA, the family of HEcontaining compounds are described as strong BACE-1 inhibitors and weak AChE inhibitors, while the HMC derivatives show increased potency against AChE along with reduced potency against BACE-1. The last series, with the HEA motif, showed good inhibition of both AChE and BACE-1. Among this series, compounds 4 and 5 were the most potent dual-acting inhibitors, with AChE IC50 = 1.83 μM and BACE-1 IC50 = 0.57 μM for 4, and AChE IC50 = 1.35 μM and BACE-1 IC50 = 0.22 μM for 5 (Fig. 8). In addition, both compounds demonstrated excellent inhibition of A formation in a cell-based assay (4 IC50 = 54.6 nM, 5 IC50 = 98.7 nM) and also displayed antioxidant properties. Preliminary in vivo studies (intracerebroventicular dosing to APP transgenic mice) revealed A anti-aggregation properties, with reduced endogenous A 1-40 production in the 23 –29% range. Bolognesi et al. [100] reported eight monomeric congeners related to the lead compound memoquin that showed a polypharmacological profile against AD [93]. This new family of memoquin derivatives was achieved by cutting the dimeric structure of memoquin into two monomers (Fig. 9). Fig. (9). Design of monovalent ligands from memoquin structure. Most of the compounds show a worse profile than memoquin in terms of AChE and BACE-1 activity. The most potent monovalent ligand is compound 6 that shows nanomolar AChE inhibition and approximately 60% inhibition of BACE-1. Docking studies of 6 with AChE and BACE-1 showed that 6 was able to interact with the catalytic site and at the same time to protrude toward the solvent-exposed gorge entrance of AChE. Regarding BACE-1, the reported conformation of 6 produces contact with Asp 32, which belongs to the catalytic dyad through hydrogen bond with several subsites of BACE-1. The group of Rosales-Hernández has recently published a family of hydroxyphenyl derivatives as multitarget compounds [101]. This new family, derived from an antioxidant hydroxyphenol compound (5-ASA), was designed by including two pharmacophore groups reported as AChE [102] and BACE-1 [103] inhibitors (Fig. 10). The best two compounds (7 and 8) (Fig. 10) show activity values ranging from 5.74 µM and 3.19 µM regarding AChE, respectively, and 10.1 nM and 15.1 nM at BACE-1, respectively. They also inhibit Aβ oligomerization and exhibit antioxidant activity. Fig. (10). Design of multitarget ligands employing the pharmacophore hypothesis for AChE and BACE-1 inhibitors. Adapted from [100, 101]. Based on a previous work where Viayna et al. developed novel huprine derivatives with inhibitory activity toward Aβ aggregation and formation [104], the authors recently have published a new family of rhein-huprine hybrids (Fig. 11) as dual inhibitors of AChE and inhibitors of BACE-1 [105]. These hybrids are composed of one unit of huprine and one unit of a natural product, rhein, structurally related with hydroxyanthraquinone derivatives such as emodin and PHF16 (Fig. 11). The most interesting compound (9) is racemic and acts as an inhibitor of human AChE (IC 50 = 2.39 nM) and BACE-1 (IC50 = 80 nM). In vivo studies in APP-PSI transgenic mice have shown that this compound has a central soluble Aβ lowering effect, accompanied by an increase in the levels of mature amyloid precursor protein (APP). Fig. (11). Structure of the multitarget rhein-huprine derivative. Very recently, Domínguez et al. have reported the existence of a pharmacophore for a multitarget approach to AD that displays some of the features of the known lead compounds that binds AChE and BACE-1. [106] The authors propose as pharmacophore the presence of a functional group such as hydroxyethylether, hydroxyethlylamine, guanidium, etc., that can interact through hydrogen bonds and ion pair with the Asp dyad of BACE-1. and one or two aromatic moieties that interact through π–stacking with aromatic residues in both the catalytic site (CAS) and peripheral site of AChE and/or BuChE (Fig. 12a). Fig. (12). a) Schematic representation of a multitarget pharmacophore. b) Structure and experimental results for indole-based compounds. Thanks to this pharmacophore together with an iterative protocol of docking and screening, the authors have identified three compounds (10-12) with interesting multitarget profiles (Fig. 12b). 3.5. Drugs targeting both AChE and MAO Ladostigil (TV3326), a dual acetylcholine-butyrylcholinesterase and brain selective monoamine oxidase (MAO)-A and -B inhibitor (Fig. 13) that has reached phase II clinical trials [107, 108] was designed and synthesized using the multitarget strategy. Fig. (13). Structure of ladostigil. Ladostigil was designed using rasagiline (Azilect), a potent MAO-B inhibitor, and a pharmacophoric carbamoyl moiety derived from rivastigmine (Fig. 13). Based on the linking of MAO inhibitors that possess a propargylamine moiety with different kinds of AChE inhibitors such as donepezil [109-111] or tacrine [112], new hybrids have been developed in recent years. 3.6. Drugs targeting both AChE and 5-HT4R During the last year various studies have validated the 5-HT4 serotonin receptor as a valuable target for AD treatment [113-115]. Recently, Dallemagne et al. published a novel multitarget family (Fig. 14) based on the combination of the frameworks of two compounds, donepezil, an AchE inhibitor, and RS67333 [116], a 5-HT4 receptor agonist, which displays both AChE inhibitory effects and partial 5-HT4R agonist activity in vitro with nanomolar potencies. [117, 118] One of the compounds, donecopride, shows in vivo procognitive and anti-amnesic effects in NMRI mice, and is able to promote the release of sAPP in C57BL/6J mice in vivo [118]. Fig. (14). Hybrids of AChE and 5- HT4R 3.7. Drugs targeting BACE-1 with metal chelating properties The aggregation of Aβ is mediated by interaction with metals, as Zn, Cu or Fe. An alteration in the homeostasis of these metals may contribute to AD pathogenesis. Therefore other interesting approach is multi-target ligands able to inhibit BACE-1 and chelate metal ions [119]. The resulting 1,3-diphenylurea derivatives combined the metal chelator LR-90 with a BACE-1 inhibitor (Fig. 15). All of the new compounds showed the ability to chelate metal and possessed discrete BACE-1 inhibitory properties. Fig. (15). Hybrids of BACE-1 inhibitors and metal chelators. 3.8. Drugs targeting both BuChE and CB2 receptors Alzheimer’s disease is characterized by a significant reduction in AChE activity and an increase in butyrylcholinesterase (BuChE) activity (about 120%). This increase of BuChE activity, especially found in the hippocampus, has been suggested to be related to the loss of episodic memory. During recent years, several studies have shown that BuChE can also hydrolyse acetylcholine in the brain and may play a role in cholinergic transmission [120, 121]. Likewise, it has been reported that BuChE might facilitate the transformation of an initial benign form of senile plaque to a malignant form associated with AD. Therefore, BuChE plays an important role in AD progression that makes it an interesting target for research in the field [122]. Cannabinoid compounds are very attractive candidates that fit into the multitarget paradigm since they could act on different pharmacological targets within the so-called endocannabinoid signaling system, but also on other targets not related to this system [122]. It has been reported that the cannabinoid system is dramatically altered in brains of AD patients [123, 124]. In 2010 a new family of indazole ethers that possess dual activity as both cannabinoid agonists of CB2 and inhibitors of BuChE was registered [125]. Using computational tools, Gonzalez-Naranjo et al. designed this new multitarget family. The results of pharmacological tests with these compounds revealed that three of these derivatives behaved as CB2 cannabinoid agonists and simultaneously showed BuChE inhibition. In particular, compounds 13 and 14 have emerged as promising candidates as novel cannabinoids that inhibit BuChE by a non-competitive or mixed mechanism, respectively. Additionally, both molecules showed antioxidant properties (Fig. 16) [126]. Fig. (16). Design of multitarget ligands. CB2 agonist and BuChE inhibitors. 3.9. Drugs targeting BACE-1 and GSK-3 BACE-1 and glycogen synthase kinase (GSK-3) are two enzymes thought to play a role in AD [127]. GSK-3 is upregulated in AD patients' brains and plays a key role in tau hyperphosphorylation [128, 129]. Recently, molecules able to modulate simultaneously BACE-1 and GSK-3 have been designed based on a fragment-based strategy. By combining the pharmacophoric features responsible for binding to BACE-1 and GSK-3, such as guanidinio and cyclic amide groups, respectively, a 6-amino-4-substituted triazinone scaffold has emerged as a new dual-target inhibitor with a promising profile in terms of neuroprotection and neurogenesis in cells (Fig. 17) [130]. Fig. (17). Dual inhibitors BACE-1/GSK-3. 4. Future work and conclusions Research to develop effective treatments for AD has evolved over the last decade. Anti-AD drug research started with the traditional single-target approach (one-to-one) where one selective drug acts on one specific target, for example, tacrine or donepezil as selective drugs for AChE inhibition. The next step was the development of bitopic drugs, in which one drug acts simultaneously at two binding sites of the same target. This strategy, where a unique drug takes advantage of interacting with one enzyme (AChE) at two different blocking sites and producing two different biological activities, may be considered the basis of the subsequent multitarget drug approach (one-to-two) where one drug acts on two or more targets. The single-target strategy (one drug-one target) shows several limitations, specifically in multifactorial diseases like cancer or neurodegenerative diseases, since complex diseases involve several aspects. This traditional strategy does not always produce the desired effect on the entire biological system probably because organisms can modulate a drug's effectiveness through compensatory changes. In this sense, a multitarget drug can be more efficacious and less vulnerable to a compensatory response since it is more difficult for a biological system to counteract the effects on several targets at the same time. Another important issue regards the constraints of druggability due to the need to develop drugs with high affinity and selectivity. Multitarget drugs usually have a low affinity towards their targets but there is evidence that low affinity does not necessarily mean low efficiency [131] and low affinity can reduce side effects. The multitarget strategy has emerged as a very interesting and attractive approach in order to develop effective drugs for neurodegenerative diseases. Different approaches have been developed in order to design and discover multitarget drugs for AD. Among these approaches, several have been highlighted here including the hybrid approach, using two molecules with different target profiles [35, 132], fragment-based [19, 133], multitargeted pharmacophore [101, 106] and multitargeted QSAR [5]. In addition, multitarget ligands have been identified by means of library screening against two or more targets [134]. It is important to mention that the first synthetic molecules that combined cholinergic activities with other non-cholinergic ones took advantage of the previous bitopic cholinergic pharmacophore strategy, with tacrine being one of the most used scaffold. More recently, the multitarget approach has been expanded to several non-cholinergic drugs, combining different activities in one molecule, without targeting AChE. Examples of the efficacy of this strategy are NP-61, a bitopic AChE inhibitor that reached clinical trial phase I, and ladostigil (TV3326), a dual acetylcholine-butyrylcholinesterase and brain selective MAO-A and -B inhibitor that is in phase II clinical trials [107, 108]. Clinical studies in AD patients will assess the value of multitarget compounds for AD pharmacological treatment in the near future. 4. References [1] Duthey, B. Background Paper 6.11 Alzheimer Disease and other Dementias. Update on 2004 Background Paper 2013. [2] 2014 Alzheimer’s Disease.Facts and Figures. Alzheimer’s Association. [3] De-Paula, V.J.; Radanovic, M.; Diniz, B.S.; Forlenza, O.V. Alzheimer's disease. Subcell Biochem, 2012, 65, 329-352. [4] Imtiaz, B.; Tolppanen, A.M.; Kivipelto, M.; Soininen, H. Future directions in Alzheimer's disease from risk factors to prevention. Biochem Pharmacol, 2014, 88, 661-670. [5] Fang, J.; Li, Y.; Liu, R.; Pang, X.; Li, C.; Yang, R.; He, Y.; Lian, W.; Liu, A.L.; Du, G.H. Discovery of Multitarget-Directed Ligands against Alzheimer's Disease through Systematic Prediction of Chemical-Protein Interactions. J Chem Inf Model, 2014, 149-164. [6] Agis-Torres, A.; Solhuber, M.; Fernandez, M.; Sanchez-Montero, J.M. Multi-Target-Directed Ligands and other Therapeutic Strategies in the Search of a Real Solution for Alzheimer's Disease. Curr Neuropharmacol, 2014, 12, 2-36. [7] Yiannopoulou, K.G.; Papageorgiou, S.G. Current and future treatments for Alzheimer's disease. Ther Adv Neurol Disord, 2013, 6, 19-33. [8] Corbett, A.; Smith, J.; Ballard, C. New and emerging treatments for Alzheimer's disease. Expert Rev Neurother, 2012, 12, 535-543. [9] Schaeffer, E.L.; Gattaz, W.F. Cholinergic and glutamatergic alterations beginning at the early stages of Alzheimer disease: participation of the phospholipase A2 enzyme. Psychopharmacology (Berl), 2008, 198, 1-27. [10] Butterfield, D.A.; Pocernich, C.B. The glutamatergic system and Alzheimer's disease: therapeutic implications. CNS Drugs, 2003, 17, 641-652. [11] Revett, T.J.; Baker, G.B.; Jhamandas, J.; Kar, S. Glutamate system, amyloid ss peptides and tau protein: functional interrelationships and relevance to Alzheimer disease pathology. J Psychiatry Neurosci, 2013, 38, 6-23. [12] Medina-Franco, J.L.; Giulianotti, M.A.; Welmaker, G.S.; Houghten, R.A. Shifting from the single to the multitarget paradigm in drug discovery. Drug Discov Today, 2013, 18, 495-501. [13] Davie, B.J.; Christopoulos, A.; Scammells, P.J. Development of M1 mAChR allosteric and bitopic ligands: prospective therapeutics for the treatment of cognitive deficits. ACS Chem Neurosci, 2013, 4, 1026-1048. [14] Nickols, H.H.; Conn, P.J. Development of allosteric modulators of GPCRs for treatment of CNS disorders. Neurobiol Dis, 2014, 61, 55-71. [15] Lane, J.R.; Sexton, P.M.; Christopoulos, A. Bridging the gap: bitopic ligands of G-protein- coupled receptors. Trends Pharmacol Sci, 2013, 34, 59-66. [16] Mohr, K.; Schmitz, J.; Schrage, R.; Trankle, C.; Holzgrabe, U. Molecular alliance-from orthosteric and allosteric ligands to dualsteric/bitopic agonists at G protein coupled receptors. Angew Chem Int Ed Engl, 2013, 52, 508-516. [17] Bajda, M.; Guzior, N.; Ignasik, M.; Malawska, B. Multi-target-directed ligands in Alzheimer's disease treatment. Curr Med Chem, 2011, 18, 4949-4975. [18] Guzior, N.; Wieckowska, A.; Panek, D.; Malawska, B. Recent development of multifunctional agents as potential drug candidates for the treatment of Alzheimer's disease. Curr Med Chem, 2015, 22, 373-404. [19] Bottegoni, G.; Favia, A.D.; Recanatini, M.; Cavalli, A. The role of fragment-based and computational methods in polypharmacology. Drug Discov Today, 2012, 17, 23-34. [20] Costantino, L.; Barlocco, D. Designed multiple ligands: basic research vs clinical outcomes. Curr Med Chem, 2012, 19, 3353-3387. [21] Cavalli, A.; Bolognesi, M.L.; Minarini, A.; Rosini, M.; Tumiatti, V.; Recanatini, M.; Melchiorre, C. Multi-target-directed ligands to combat neurodegenerative diseases. J Med Chem, 2008, 51, 347-372. [22] Bolognesi, M.L.; Simoni, E.; Rosini, M.; Minarini, A.; Tumiatti, V.; Melchiorre, C. Multitarget- directed ligands: innovative chemical probes and therapeutic tools against Alzheimer's disease. Curr Top Med Chem, 2011, 11, 2797-2806. [23] Olivera, S.; Rodriguez-Ithurralde, D.; Henley, J.M. Acetylcholinesterase promotes neurite elongation, synapse formation, and surface expression of AMPA receptors in hippocampal neurones. Mol Cell Neurosci, 2003, 23, 96-106. [24] Chacon, M.A.; Reyes, A.E.; Inestrosa, N.C. Acetylcholinesterase induces neuronal cell loss, astrocyte hypertrophy and behavioral deficits in mammalian hippocampus. J Neurochem, 2003, 87, 195204. [25] Alvarez, A.; Bronfman, F.; Perez, C.A.; Vicente, M.; Garrido, J.; Inestrosa, N.C. Acetylcholinesterase, a senile plaque component, affects the fibrillogenesis of amyloid-beta-peptides. Neurosci Lett, 1995, 201, 49-52. [26] Rees, T.; Hammond, P.I.; Soreq, H.; Younkin, S.; Brimijoin, S. Acetylcholinesterase promotes beta-amyloid plaques in cerebral cortex. Neurobiol Aging, 2003, 24, 777-787. [27] De Ferrari, G.V.; Canales, M.A.; Shin, I.; Weiner, L.M.; Silman, I.; Inestrosa, N.C. A structural motif of acetylcholinesterase that promotes amyloid beta-peptide fibril formation. Biochemistry, 2001, 40, 10447-10457. [28] Johnson, G.; Moore, S.W. The adhesion function on acetylcholinesterase is located at the peripheral anionic site. Biochem Biophys Res Commun, 1999, 258, 758-762. [29] Castro, A.; Martinez, A. Peripheral and dual binding site acetylcholinesterase inhibitors: implications in treatment of Alzheimer's disease. Mini Rev Med Chem, 2001, 1, 267-272. [30] Johnson, G.; Moore, S.W. The peripheral anionic site of acetylcholinesterase: structure, functions and potential role in rational drug design. Curr Pharm Des, 2006, 12, 217-225. [31] Garcia-Palomero, E.; Munoz, P.; Usan, P.; Garcia, P.; Delgado, E.; De Austria, C.; Valenzuela, R.; Rubio, L.; Medina, M.; Martinez, A. Potent beta-amyloid modulators. Neurodegener Dis, 2008, 5, 153-156. [32] Castro, A.; Martinez, A. Targeting beta-amyloid pathogenesis through acetylcholinesterase inhibitors. Curr Pharm Des, 2006, 12, 4377-4387. [33] Munoz-Torrero, D. Acetylcholinesterase inhibitors as disease-modifying therapies for Alzheimer's disease. Curr Med Chem, 2008, 15, 2433-2455. [34] Munoz-Torrero, D.; Camps, P. Huprines for Alzheimer's disease drug development. Expert Opin Drug Discov, 2008, 3, 65-81. [35] Rodrigues Simoes, M.C.; Dias Viegas, F.P.; Moreira, M.S.; de Freitas Silva, M.; Riquiel, M.M.; da Rosa, P.M.; Castelli, M.R.; dos Santos, M.H.; Soares, M.G.; Viegas, C., Jr. Donepezil: an important prototype to the design of new drug candidates for Alzheimer's disease. Mini Rev Med Chem, 2013, 14, 219. [36] del Monte-Millan, M.; Garcia-Palomero, E.; Valenzuela, R.; Usan, P.; de Austria, C.; Munoz- Ruiz, P.; Rubio, L.; Dorronsoro, I.; Martinez, A.; Medina, M. Dual binding site acetylcholinesterase inhibitors: potential new disease-modifying agents for AD. J Mol Neurosci, 2006, 30, 85-88. [37] Melchiorre, C.; Bolognesi, M.L.; Minarini, A.; Rosini, M.; Tumiatti, V. Polyamines in drug discovery: from the universal template approach to the multitarget-directed ligand design strategy. J Med Chem, 2010, 53, 5906-5914. [38] Piazzi, L.; Rampa, A.; Bisi, A.; Gobbi, S.; Belluti, F.; Cavalli, A.; Bartolini, M.; Andrisano, V.; Valenti, P.; Recanatini, M. 3-(4-[[Benzyl(methyl)amino]methyl]phenyl)-6,7-dimethoxy-2H-2chromenone (AP2238) inhibits both acetylcholinesterase and acetylcholinesterase-induced beta-amyloid aggregation: a dual function lead for Alzheimer's disease therapy. J Med Chem, 2003, 46, 2279-2282. [39] Munoz-Ruiz, P.; Rubio, L.; Garcia-Palomero, E.; Dorronsoro, I.; del Monte-Millan, M.; Valenzuela, R.; Usan, P.; de Austria, C.; Bartolini, M.; Andrisano, V.; Bidon-Chanal, A.; Orozco, M.; Luque, F.J.; Medina, M.; Martinez, A. Design, synthesis, and biological evaluation of dual binding site acetylcholinesterase inhibitors: new disease-modifying agents for Alzheimer's disease. J Med Chem, 2005, 48, 7223-7233. [40] Rosenberry, T.L.; Sonoda, L.K.; Dekat, S.E.; Cusack, B.; Johnson, J.L. Monitoring the reaction of carbachol with acetylcholinesterase by thioflavin T fluorescence and acetylthiocholine hydrolysis. Chem Biol Interact, 2008, 175, 235-241. [41] Galdeano, C.; Viayna, E.; Arroyo, P.; Bidon-Chanal, A.; Blas, J.R.; Munoz-Torrero, D.; Luque, F.J. Structural determinants of the multifunctional profile of dual binding site acetylcholinesterase inhibitors as anti-Alzheimer agents. Curr Pharm Des, 2010, 16, 2818-2836. [42] Hou, L.N.; Xu, J.R.; Zhao, Q.N.; Gao, X.L.; Cui, Y.Y.; Xu, J.; Wang, H.; Chen, H.Z. A new motif in the N-terminal of acetylcholinesterase triggers amyloid-beta aggregation and deposition. CNS Neurosci Ther, 2014, 20, 59-66. [43] Matera, C.; Tata, A.M. Pharmacological approaches to targeting muscarinic acetylcholine receptors. Recent Pat CNS Drug Discov, 2014, 9, 85-100. [44] Keov, P.; Lopez, L.; Devine, S.M.; Valant, C.; Lane, J.R.; Scammells, P.J.; Sexton, P.M.; Christopoulos, A. Molecular mechanisms of bitopic ligand engagement with the M1 muscarinic acetylcholine receptor. J Biol Chem, 2014, 289, 23817-23837. [45] Zimmermann, G.R.; Lehar, J.; Keith, C.T. Multi-target therapeutics: when the whole is greater than the sum of the parts. Drug Discov Today, 2007, 12, 34-42. [46] Morphy, R.; Rankovic, Z. Designed multiple ligands. An emerging drug discovery paradigm. J Med Chem, 2005, 48, 6523-6543. [47] Geldenhuys, W.J.; Youdim, M.B.; Carroll, R.T.; Van der Schyf, C.J. The emergence of designed multiple ligands for neurodegenerative disorders. Prog Neurobiol, 2011, 94, 347-359. [48] Youdim, M.B. Why do we need multifunctional neuroprotective and neurorestorative drugs for Parkinson's and Alzheimer's diseases as disease modifying agents. Exp Neurobiol, 2010, 19, 1-14. [49] Speck-Planche, A.; Luan, F.; Cordeiro, M.N. Role of ligand-based drug design methodologies toward the discovery of new anti- Alzheimer agents: futures perspectives in Fragment-Based Ligand Design. Curr Med Chem, 2012, 19, 1635-1645. [50] Zheng, H.; Fridkin, M.; Youdim, M. From single target to multitarget/network therapeutics in Alzheimer's therapy. Pharmaceuticals (Basel), 2014, 7, 113-135. [51] Morphy, R.; Rankovic, Z. Designing multiple ligands - medicinal chemistry strategies and challenges. Curr Pharm Des, 2009, 15, 587-600. [52] Tariot, P.N.; Farlow, M.R.; Grossberg, G.T.; Graham, S.M.; McDonald, S.; Gergel, I.; Memantine Study, G. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA, 2004, 291, 317-324. [53] Gauthier, S.; Molinuevo, J.L. Benefits of combined cholinesterase inhibitor and memantine treatment in moderate-severe Alzheimer's disease. Alzheimers Dement, 2013, 9, 326-331. [54] Porsteinsson, A.P.; Grossberg, G.T.; Mintzer, J.; Olin, J.T. Memantine treatment in patients with mild to moderate Alzheimer's disease already receiving a cholinesterase inhibitor: a randomized, doubleblind, placebo-controlled trial. Curr Alzheimer Res, 2008, 5, 83-89. [55] Grossberg, G.T.; Manes, F.; Allegri, R.F.; Gutierrez-Robledo, L.M.; Gloger, S.; Xie, L.; Jia, X.D.; Pejovic, V.; Miller, M.L.; Perhach, J.L.; Graham, S.M. The safety, tolerability, and efficacy of once-daily memantine (28 mg): a multinational, randomized, double-blind, placebo-controlled trial in patients with moderate-to-severe Alzheimer's disease taking cholinesterase inhibitors. CNS Drugs, 2013, 27, 469-478. [56] Boinpally, R.; Chen, L.; Zukin, S.R.; McClure, N.; Hofbauer, R.K.; Periclou, A. A Novel Once- Daily Fixed-Dose Combination of Memantine Extended Release and Donepezil for the Treatment of Moderate to Severe Alzheimer's Disease: Two Phase I Studies in Healthy Volunteers. Clin Drug Investig, 2015. [57] Rosini, M.; Simoni, E.; Minarini, A.; Melchiorre, C. Multi-target design strategies in the context of Alzheimer's disease: acetylcholinesterase inhibition and NMDA receptor antagonism as the driving forces. Neurochem Res, 2014, 39, 1914-1923. [58] Rosini, M.; Simoni, E.; Bartolini, M.; Cavalli, A.; Ceccarini, L.; Pascu, N.; McClymont, D.W.; Tarozzi, A.; Bolognesi, M.L.; Minarini, A.; Tumiatti, V.; Andrisano, V.; Mellor, I.R.; Melchiorre, C. Inhibition of acetylcholinesterase, beta-amyloid aggregation, and NMDA receptors in Alzheimer's disease: a promising direction for the multi-target-directed ligands gold rush. J Med Chem, 2008, 51, 4381-4384. [59] Lysko, P.G.; Lysko, K.A.; Webb, C.L.; Feuerstein, G.; Mason, P.E.; Walter, M.F.; Mason, R.P. Neuroprotective activities of carvedilol and a hydroxylated derivative: role of membrane biophysical interactions. Biochem Pharmacol, 1998, 56, 1645-1656. [60] Howlett, D.R.; George, A.R.; Owen, D.E.; Ward, R.V.; Markwell, R.E. Common structural features determine the effectiveness of carvedilol, daunomycin and rolitetracycline as inhibitors of Alzheimer beta-amyloid fibril formation. Biochem J, 1999, 343 Pt 2, 419-423. [61] Simoni, E.; Daniele, S.; Bottegoni, G.; Pizzirani, D.; Trincavelli, M.L.; Goldoni, L.; Tarozzo, G.; Reggiani, A.; Martini, C.; Piomelli, D.; Melchiorre, C.; Rosini, M.; Cavalli, A. Combining galantamine and memantine in multitargeted, new chemical entities potentially useful in Alzheimer's disease. J Med Chem, 2012, 55, 9708-9721. [62] Busquet, P.; Capurro, V.; Cavalli, A.; Piomelli, D.; Reggiani, A.; Bertorelli, R. Synergistic effects of galantamine and memantine in attenuating scopolamine-induced amnesia in mice. J Pharmacol Sci, 2012, 120, 305-309. [63] Takada-Takatori, Y.; Kume, T.; Sugimoto, M.; Katsuki, H.; Sugimoto, H.; Akaike, A. Acetylcholinesterase inhibitors used in treatment of Alzheimer's disease prevent glutamate neurotoxicity via nicotinic acetylcholine receptors and phosphatidylinositol 3-kinase cascade. Neuropharmacology, 2006, 51, 474-486. [64] Bachurin, S.; Bukatina, E.; Lermontova, N.; Tkachenko, S.; Afanasiev, A.; Grigoriev, V.; Grigorieva, I.; Ivanov, Y.; Sablin, S.; Zefirov, N. Antihistamine agent Dimebon as a novel neuroprotector and a cognition enhancer. Ann N Y Acad Sci, 2001, 939, 425-435. [65] Doody, R.S.; Gavrilova, S.I.; Sano, M.; Thomas, R.G.; Aisen, P.S.; Bachurin, S.O.; Seely, L.; Hung, D.; dimebon, i. Effect of dimebon on cognition, activities of daily living, behaviour, and global function in patients with mild-to-moderate Alzheimer's disease: a randomised, double-blind, placebocontrolled study. Lancet, 2008, 372, 207-215. [66] Jones, R.W. Dimebon disappointment. Alzheimers Res Ther, 2010, 2, 25. [67] Giorgetti, M.; Gibbons, J.A.; Bernales, S.; Alfaro, I.E.; Drieu La Rochelle, C.; Cremers, T.; Altar, C.A.; Wronski, R.; Hutter-Paier, B.; Protter, A.A. Cognition-enhancing properties of Dimebon in a rat novel object recognition task are unlikely to be associated with acetylcholinesterase inhibition or Nmethyl-D-aspartate receptor antagonism. J Pharmacol Exp Ther, 2010, 333, 748-757. [68] Rosini, M.; Simoni, E.; Bartolini, M.; Soriano, E.; Marco-Contelles, J.; Andrisano, V.; Monti, B.; Windisch, M.; Hutter-Paier, B.; McClymont, D.W.; Mellor, I.R.; Bolognesi, M.L. The bivalent ligand approach as a tool for improving the in vitro anti-Alzheimer multitarget profile of dimebon. ChemMedChem, 2013, 8, 1276-1281. [69] Pang, Y.P.; Quiram, P.; Jelacic, T.; Hong, F.; Brimijoin, S. Highly potent, selective, and low cost bis-tetrahydroaminacrine inhibitors of acetylcholinesterase. Steps toward novel drugs for treating Alzheimer's disease. J Biol Chem, 1996, 271, 23646-23649. [70] Li, W.; Pi, R.; Chan, H.H.; Fu, H.; Lee, N.T.; Tsang, H.W.; Pu, Y.; Chang, D.C.; Li, C.; Luo, J.; Xiong, K.; Li, Z.; Xue, H.; Carlier, P.R.; Pang, Y.; Tsim, K.W.; Li, M.; Han, Y. Novel dimeric acetylcholinesterase inhibitor bis7-tacrine, but not donepezil, prevents glutamate-induced neuronal apoptosis by blocking N-methyl-D-aspartate receptors. J Biol Chem, 2005, 280, 18179-18188. [71] Rook, Y.; Schmidtke, K.U.; Gaube, F.; Schepmann, D.; Wunsch, B.; Heilmann, J.; Lehmann, J.; Winckler, T. Bivalent beta-carbolines as potential multitarget anti-Alzheimer agents. J Med Chem, 2010, 53, 3611-3617. [72] Berlin, M.; Boyce, C.W.; Ruiz Mde, L. Histamine H3 receptor as a drug discovery target. J Med Chem, 2011, 54, 26-53. [73] Barbier, A.J.; Berridge, C.; Dugovic, C.; Laposky, A.D.; Wilson, S.J.; Boggs, J.; Aluisio, L.; Lord, B.; Mazur, C.; Pudiak, C.M.; Langlois, X.; Xiao, W.; Apodaca, R.; Carruthers, N.I.; Lovenberg, T.W. Acute wake-promoting actions of JNJ-5207852, a novel, diamine-based H3 antagonist. Br J Pharmacol, 2004, 143, 649-661. [74] Celanire, S.; Wijtmans, M.; Talaga, P.; Leurs, R.; de Esch, I.J. Keynote review: histamine H3 receptor antagonists reach out for the clinic. Drug Discov Today, 2005, 10, 1613-1627. [75] Apelt, J.; Ligneau, X.; Pertz, H.H.; Arrang, J.M.; Ganellin, C.R.; Schwartz, J.C.; Schunack, W.; Stark, H. Development of a new class of nonimidazole histamine H(3) receptor ligands with combined inhibitory histamine N-methyltransferase activity. J Med Chem, 2002, 45, 1128-1141. [76] Incerti, M.; Flammini, L.; Saccani, F.; Morini, G.; Comini, M.; Coruzzi, M.; Barocelli, E.; Ballabeni, V.; Bertoni, S. Dual-acting drugs: an in vitro study of nonimidazole histamine H3 receptor antagonists combining anticholinesterase activity. ChemMedChem, 2010, 5, 1143-1149. [77] Keith, J.M.; Gomez, L.A.; Wolin, R.L.; Barbier, A.J.; Wilson, S.J.; Boggs, J.D.; Mazur, C.; Fraser, I.C.; Lord, B.; Aluisio, L.; Lovenberg, T.W.; Carruthers, N.I. Pyrrolidino-tetrahydroisoquinolines as potent dual H3 antagonist and serotonin transporter inhibitors. Bioorg Med Chem Lett, 2007, 17, 26032607. [78] Roche, O.; Rodriguez Sarmiento, R.M. A new class of histamine H3 receptor antagonists derived from ligand based design. Bioorg Med Chem Lett, 2007, 17, 3670-3675. [79] Darras, F.H.; Kling, B.; Heilmann, J.; Decker, M. Neuroprotective tri- and tetracyclic BChE inhibitors releasing reversible inhibitors upon carbamate transfer. ACS Med Chem Lett, 2012, 3, 914-919. [80] Bembenek, S.D.; Keith, J.M.; Letavic, M.A.; Apodaca, R.; Barbier, A.J.; Dvorak, L.; Aluisio, L.; Miller, K.L.; Lovenberg, T.W.; Carruthers, N.I. Lead identification of acetylcholinesterase inhibitorshistamine H3 receptor antagonists from molecular modeling. Bioorg Med Chem, 2008, 16, 2968-2973. [81] Aliev, G.; Priyadarshini, M.; Reddy, V.P.; Grieg, N.H.; Kaminsky, Y.; Cacabelos, R.; Ashraf, G.M.; Jabir, N.R.; Kamal, M.A.; Nikolenko, V.N.; Zamyatnin, A.A., Jr.; Benberin, V.V.; Bachurin, S.O. Oxidative stress mediated mitochondrial and vascular lesions as markers in the pathogenesis of Alzheimer disease. Curr Med Chem, 2014, 21, 2208-2217. [82] Minarini, A.; Milelli, A.; Simoni, E.; Rosini, M.; Bolognesi, M.L.; Marchetti, C.; Tumiatti, V. Multifunctional tacrine derivatives in Alzheimer's disease. Curr Top Med Chem, 2013, 13, 1771-1786. [83] Rodriguez-Franco, M.I.; Fernandez-Bachiller, M.I.; Perez, C.; Hernandez-Ledesma, B.; Bartolome, B. Novel tacrine-melatonin hybrids as dual-acting drugs for Alzheimer disease, with improved acetylcholinesterase inhibitory and antioxidant properties. J Med Chem, 2006, 49, 459-462. [84] Fernandez-Bachiller, M.I.; Perez, C.; Gonzalez-Munoz, G.C.; Conde, S.; Lopez, M.G.; Villarroya, M.; Garcia, A.G.; Rodriguez-Franco, M.I. Novel tacrine-8-hydroxyquinoline hybrids as multifunctional agents for the treatment of Alzheimer's disease, with neuroprotective, cholinergic, antioxidant, and copper-complexing properties. J Med Chem, 2010, 53, 4927-4937. [85] Fernandez-Bachiller, M.I.; Perez, C.; Monjas, L.; Rademann, J.; Rodriguez-Franco, M.I. New tacrine-4-oxo-4H-chromene hybrids as multifunctional agents for the treatment of Alzheimer's disease, with cholinergic, antioxidant, and beta-amyloid-reducing properties. J Med Chem, 2012, 55, 1303-1317. [86] Nepovimova, E.; Uliassi, E.; Korabecny, J.; Pena-Altamira, L.E.; Samez, S.; Pesaresi, A.; Garcia, G.E.; Bartolini, M.; Andrisano, V.; Bergamini, C.; Fato, R.; Lamba, D.; Roberti, M.; Kuca, K.; Monti, B.; Bolognesi, M.L. Multitarget drug design strategy: quinone-tacrine hybrids designed to block amyloid-beta aggregation and to exert anticholinesterase and antioxidant effects. J Med Chem, 2014, 57, 8576-8589. [87] Benchekroun, M.; Bartolini, M.; Egea, J.; Romero, A.; Soriano, E.; Pudlo, M.; Luzet, V.; Andrisano, V.; Jimeno, M.L.; Lopez, M.G.; Wehle, S.; Gharbi, T.; Refouvelet, B.; de Andres, L.; Herrera-Arozamena, C.; Monti, B.; Bolognesi, M.L.; Rodriguez-Franco, M.I.; Decker, M.; MarcoContelles, J.; Ismaili, L. Novel tacrine-grafted Ugi adducts as multipotent anti-Alzheimer drugs: A synthetic renewal in tacrine-ferulic acid hybrids. ChemMedChem, 2014. [88] Reiter, R.J.; Guerrero, J.M.; Garcia, J.J.; Acuna-Castroviejo, D. Reactive oxygen intermediates, molecular damage, and aging. Relation to melatonin. Ann N Y Acad Sci, 1998, 854, 410-424. [89] Fernandez-Bachiller, M.I.; Perez, C.; Campillo, N.E.; Paez, J.A.; Gonzalez-Munoz, G.C.; Usan, P.; Garcia-Palomero, E.; Lopez, M.G.; Villarroya, M.; Garcia, A.G.; Martinez, A.; Rodriguez-Franco, M.I. Tacrine-melatonin hybrids as multifunctional agents for Alzheimer's disease, with cholinergic, antioxidant, and neuroprotective properties. ChemMedChem, 2009, 4, 828-841. [90] Huang, X.; Moir, R.D.; Tanzi, R.E.; Bush, A.I.; Rogers, J.T. Redox-active metals, oxidative stress, and Alzheimer's disease pathology. Ann N Y Acad Sci, 2004, 1012, 153-163. [91] Bareggi, S.R.; Cornelli, U. Clioquinol: review of its mechanisms of action and clinical uses in neurodegenerative disorders. CNS Neurosci Ther, 2012, 18, 41-46. [92] Spencer, J.P. Beyond antioxidants: the cellular and molecular interactions of flavonoids and how these underpin their actions on the brain. Proc Nutr Soc, 2010, 69, 244-260. [93] Cavalli, A.; Bolognesi, M.L.; Capsoni, S.; Andrisano, V.; Bartolini, M.; Margotti, E.; Cattaneo, A.; Recanatini, M.; Melchiorre, C. A small molecule targeting the multifactorial nature of Alzheimer's disease. Angew Chem Int Ed Engl, 2007, 46, 3689-3692. [94] Melchiorre, C.; Andrisano, V.; Bolognesi, M.L.; Budriesi, R.; Cavalli, A.; Cavrini, V.; Rosini, M.; Tumiatti, V.; Recanatini, M. Acetylcholinesterase noncovalent inhibitors based on a polyamine backbone for potential use against Alzheimer's disease. J Med Chem, 1998, 41, 4186-4189. [95] Bolognesi, M.L.; Cavalli, A.; Melchiorre, C. Memoquin: a multi-target-directed ligand as an innovative therapeutic opportunity for Alzheimer's disease. Neurotherapeutics, 2009, 6, 152-162. [96] Bolognesi, M.L.; Cavalli, A.; Bergamini, C.; Fato, R.; Lenaz, G.; Rosini, M.; Bartolini, M.; Andrisano, V.; Melchiorre, C. Toward a rational design of multitarget-directed antioxidants: merging memoquin and lipoic acid molecular frameworks. J Med Chem, 2009, 52, 7883-7886. [97] Lopez-Iglesias, B.; Perez, C.; Morales-Garcia, J.A.; Alonso-Gil, S.; Perez-Castillo, A.; Romero, A.; Lopez, M.G.; Villarroya, M.; Conde, S.; Rodriguez-Franco, M.I. New melatonin-N,N-dibenzyl(Nmethyl)amine hybrids: potent neurogenic agents with antioxidant, cholinergic, and neuroprotective properties as innovative drugs for Alzheimer's disease. J Med Chem, 2014, 57, 3773-3785. [98] Zhu, Y.; Xiao, K.; Ma, L.; Xiong, B.; Fu, Y.; Yu, H.; Wang, W.; Wang, X.; Hu, D.; Peng, H.; Li, J.; Gong, Q.; Chai, Q.; Tang, X.; Zhang, H.; Shen, J. Design, synthesis and biological evaluation of novel dual inhibitors of acetylcholinesterase and beta-secretase. Bioorg Med Chem, 2009, 17, 1600-1613. [99] Piazzi, L.; Cavalli, A.; Colizzi, F.; Belluti, F.; Bartolini, M.; Mancini, F.; Recanatini, M.; Andrisano, V.; Rampa, A. Multi-target-directed coumarin derivatives: hAChE and BACE1 inhibitors as potential anti-Alzheimer compounds. Bioorg Med Chem Lett, 2008, 18, 423-426. [100] Bolognesi, M.L.; Chiriano, G.; Bartolini, M.; Mancini, F.; Bottegoni, G.; Maestri, V.; Czvitkovich, S.; Windisch, M.; Cavalli, A.; Minarini, A.; Rosini, M.; Tumiatti, V.; Andrisano, V.; Melchiorre, C. Synthesis of monomeric derivatives to probe memoquin's bivalent interactions. J Med Chem, 2011, 54, 8299-8304. [101] Hernandez-Rodriguez, M.; Correa-Basurto, J.; Martinez-Ramos, F.; Padilla, M., II; Benitez- Cardoza, C.G.; Mera-Jimenez, E.; Rosales-Hernandez, M.C. Design of multi-target compounds as AChE, BACE1, and amyloid-beta(1-42) oligomerization inhibitors: in silico and in vitro studies. J Alzheimers Dis, 2014, 41, 1073-1085. [102] Lu, S.H.; Wu, J.W.; Liu, H.L.; Zhao, J.H.; Liu, K.T.; Chuang, C.K.; Lin, H.Y.; Tsai, W.B.; Ho, Y. The discovery of potential acetylcholinesterase inhibitors: a combination of pharmacophore modeling, virtual screening, and molecular docking studies. J Biomed Sci, 2011, 18, 8. [103] John, S.; Thangapandian, S.; Sakkiah, S.; Lee, K.W. Potent BACE-1 inhibitor design using pharmacophore modeling, in silico screening and molecular docking studies. BMC Bioinformatics, 2011, 12 Suppl 1, S28. [104] Viayna, E.; Gomez, T.; Galdeano, C.; Ramirez, L.; Ratia, M.; Badia, A.; Clos, M.V.; Verdaguer, E.; Junyent, F.; Camins, A.; Pallas, M.; Bartolini, M.; Mancini, F.; Andrisano, V.; Arce, M.P.; RodriguezFranco, M.I.; Bidon-Chanal, A.; Luque, F.J.; Camps, P.; Munoz-Torrero, D. Novel huprine derivatives with inhibitory activity toward beta-amyloid aggregation and formation as disease-modifying antiAlzheimer drug candidates. ChemMedChem, 2010, 5, 1855-1870. [105] Viayna, E.; Sola, I.; Bartolini, M.; De Simone, A.; Tapia-Rojas, C.; Serrano, F.G.; Sabate, R.; Juarez-Jimenez, J.; Perez, B.; Luque, F.J.; Andrisano, V.; Clos, M.V.; Inestrosa, N.C.; Munoz-Torrero, D. Synthesis and multitarget biological profiling of a novel family of rhein derivatives as disease-modifying anti-Alzheimer agents. J Med Chem, 2014, 57, 2549-2567. [106] Dominguez, J.L.; Fernandez-Nieto, F.; Castro, M.; Catto, M.; Paleo, M.R.; Porto, S.; Sardina, F.J.; Brea, J.M.; Carotti, A.; Villaverde, M.C.; Sussman, F. Computer-aided structure-based design of multitarget leads for Alzheimer's disease. J Chem Inf Model, 2014, 55, 135-148. [107] Weinreb, O.; Amit, T.; Bar-Am, O.; Youdim, M.B. A novel anti-Alzheimer's disease drug, ladostigil neuroprotective, multimodal brain-selective monoamine oxidase and cholinesterase inhibitor. Int Rev Neurobiol, 2011, 100, 191-215. [108] Weinreb, O.; Amit, T.; Bar-Am, O.; Youdim, M.B. Ladostigil: a novel multimodal neuroprotective drug with cholinesterase and brain-selective monoamine oxidase inhibitory activities for Alzheimer's disease treatment. Curr Drug Targets, 2012, 13, 483-494. [109] Bolea, I.; Juarez-Jimenez, J.; de Los Rios, C.; Chioua, M.; Pouplana, R.; Luque, F.J.; Unzeta, M.; Marco-Contelles, J.; Samadi, A. Synthesis, biological evaluation, and molecular modeling of donepezil and N-[(5-(benzyloxy)-1-methyl-1H-indol-2-yl)methyl]-N-methylprop-2-yn-1-amine hybrids as new multipotent cholinesterase/monoamine oxidase inhibitors for the treatment of Alzheimer's disease. J Med Chem, 2011, 54, 8251-8270. [110] Bautista-Aguilera, O.M.; Esteban, G.; Bolea, I.; Nikolic, K.; Agbaba, D.; Moraleda, I.; Iriepa, I.; Samadi, A.; Soriano, E.; Unzeta, M.; Marco-Contelles, J. Design, synthesis, pharmacological evaluation, QSAR analysis, molecular modeling and ADMET of novel donepezil-indolyl hybrids as multipotent cholinesterase/monoamine oxidase inhibitors for the potential treatment of Alzheimer's disease. Eur J Med Chem, 2014, 75, 82-95. [111] Bautista-Aguilera, O.M.; Samadi, A.; Chioua, M.; Nikolic, K.; Filipic, S.; Agbaba, D.; Soriano, E.; de Andres, L.; Rodriguez-Franco, M.I.; Alcaro, S.; Ramsay, R.R.; Ortuso, F.; Yanez, M.; MarcoContelles, J. N-Methyl-N-((1-methyl-5-(3-(1-(2-methylbenzyl)piperidin-4-yl)propoxy)-1H-indol-2yl)methyl)prop-2-yn-1-amine, a New Cholinesterase and Monoamine Oxidase Dual Inhibitor. J Med Chem, 2014, 57, 10455-10463. [112] Samadi, A.; de los Rios, C.; Bolea, I.; Chioua, M.; Iriepa, I.; Moraleda, I.; Bartolini, M.; Andrisano, V.; Galvez, E.; Valderas, C.; Unzeta, M.; Marco-Contelles, J. Multipotent MAO and cholinesterase inhibitors for the treatment of Alzheimer's disease: synthesis, pharmacological analysis and molecular modeling of heterocyclic substituted alkyl and cycloalkyl propargyl amine. Eur J Med Chem, 2012, 52, 251-262. [113] Robert, S.; Maillet, M.; Morel, E.; Launay, J.M.; Fischmeister, R.; Mercken, L.; Lezoualc'h, F. Regulation of the amyloid precursor protein ectodomain shedding by the 5-HT4 receptor and Epac. FEBS Lett, 2005, 579, 1136-1142. [114] Cho, S.; Hu, Y. Activation of 5-HT4 receptors inhibits secretion of beta-amyloid peptides and increases neuronal survival. Exp Neurol, 2007, 203, 274-278. [115] Lezoualc'h, F. 5-HT4 receptor and Alzheimer's disease: the amyloid connection. Exp Neurol, 2007, 205, 325-329. [116] Freret, T.; Bouet, V.; Quiedeville, A.; Nee, G.; Dallemagne, P.; Rochais, C.; Boulouard, M. Synergistic effect of acetylcholinesterase inhibition (donepezil) and 5-HT(4) receptor activation (RS67333) on object recognition in mice. Behav Brain Res, 2012, 230, 304-308. [117] Lecoutey, C.; Hedou, D.; Freret, T.; Giannoni, P.; Gaven, F.; Since, M.; Bouet, V.; Ballandonne, C.; Corvaisier, S.; Malzert Freon, A.; Mignani, S.; Cresteil, T.; Boulouard, M.; Claeysen, S.; Rochais, C.; Dallemagne, P. Design of donecopride, a dual serotonin subtype 4 receptor agonist/acetylcholinesterase inhibitor with potential interest for Alzheimer's disease treatment. Proc Natl Acad Sci U S A, 2014, 111, E3825-3830. [118] Rochais, C.; Lecoutey, C.; Gaven, F.; Giannoni, P.; Hamidouche, K.; Hedou, D.; Dubost, E.; Genest, D.; Yahiaoui, S.; Freret, T.; Bouet, V.; Dauphin, F.; Sopkova de Oliveira Santos, J.; Ballandonne, C.; Corvaisier, S.; Malzert-Freon, A.; Legay, R.; Boulouard, M.; Claeysen, S.; Dallemagne, P. Novel multitarget-directed ligands (MTDLs) with acetylcholinesterase (AChE) inhibitory and serotonergic subtype 4 receptor (5-HT4R) agonist activities as potential agents against Alzheimer's disease: the design of donecopride. J Med Chem, 2015, 58, 3172-3187. [119] Huang, W.; Lv, D.; Yu, H.; Sheng, R.; Kim, S.C.; Wu, P.; Luo, K.; Li, J.; Hu, Y. Dual-target- directed 1,3-diphenylurea derivatives: BACE 1 inhibitor and metal chelator against Alzheimer's disease. Bioorg Med Chem, 2010, 18, 5610-5615. [120] Mufson, E.J.; Counts, S.E.; Perez, S.E.; Ginsberg, S.D. Cholinergic system during the progression of Alzheimer's disease: therapeutic implications. Expert Rev Neurother, 2008, 8, 1703-1718. [121] Terry, A.V., Jr.; Buccafusco, J.J. The cholinergic hypothesis of age and Alzheimer's disease- related cognitive deficits: recent challenges and their implications for novel drug development. J Pharmacol Exp Ther, 2003, 306, 821-827. [122] Gonzalez-Naranjo, P.; Campillo, N.E.; Perez, C.; Paez, J.A. Multitarget cannabinoids as novel strategy for Alzheimer disease. Curr Alzheimer Res, 2013, 10, 229-239. [123] Maroof, N.; Pardon, M.C.; Kendall, D.A. Endocannabinoid signalling in Alzheimer's disease. Biochem Soc Trans, 2013, 41, 1583-1587. [124] Aso, E.; Ferrer, I. Cannabinoids for treatment of Alzheimer's disease: moving toward the clinic. Front Pharmacol, 2014, 5, 37. [125] Páez, J.A., Campillo, N.E., González-Naranjo, P.; Pérez, C., Arán, V.J. Martín-Fontelles, M.I., Girón R., Sánchez, E.M. Preparation of 3-Indazolyl Ethers with Cannabinoid and/or Cholinergic Properties Useful for Treating Various Diseases. 2009. [126] Gonzalez-Naranjo, P.; Perez-Macias, N.; Campillo, N.E.; Perez, C.; Aran, V.J.; Giron, R.; Sanchez-Robles, E.; Martin, M.I.; Gomez-Canas, M.; Garcia-Arencibia, M.; Fernandez-Ruiz, J.; Paez, J.A. Cannabinoid agonists showing BuChE inhibition as potential therapeutic agents for Alzheimer's disease. Eur J Med Chem, 2014, 73, 56-72. [127] Preece, P.; Virley, D.J.; Costandi, M.; Coombes, R.; Moss, S.J.; Mudge, A.W.; Jazin, E.; Cairns, N.J. Beta-secretase (BACE) and GSK-3 mRNA levels in Alzheimer's disease. Brain Res Mol Brain Res, 2003, 116, 155-158. [128] Stamford, A.; Strickland, C. Inhibitors of BACE for treating Alzheimer's disease: a fragment- based drug discovery story. Curr Opin Chem Biol, 2013, 17, 320-328. [129] Martinez, A.; Perez, D.I.; Gil, C. Lessons learnt from glycogen synthase kinase 3 inhibitors development for Alzheimer's disease. Curr Top Med Chem, 2013, 13, 1808-1819. [130] Prati, F.; De Simone, A.; Bisignano, P.; Armirotti, A.; Summa, M.; Pizzirani, D.; Scarpelli, R.; Perez, D.I.; Andrisano, V.; Perez-Castillo, A.; Monti, B.; Massenzio, F.; Polito, L.; Racchi, M.; Favia, A.D.; Bottegoni, G.; Martinez, A.; Bolognesi, M.L.; Cavalli, A. Multitarget Drug Discovery for Alzheimer's Disease: Triazinones as BACE-1 and GSK-3beta Inhibitors. Angew Chem Int Ed Engl, 2015, 54, 1578-1582. [131] Korcsmaros, T.; Szalay, M.S.; Bode, C.; Kovacs, I.A.; Csermely, P. How to design multi-target drugs. Expert Opin Drug Discov, 2007, 2, 799-808. [132] Leon, R.; Marco-Contelles, J. A step further towards multitarget drugs for Alzheimer and neuronal vascular diseases: targeting the cholinergic system, amyloid-beta aggregation and Ca(2+) dyshomeostasis. Curr Med Chem, 2011, 18, 552-576. [133] Speck-Planche, A.; Kleandrova, V.V.; Luan, F.; Cordeiro, M.N. Multi-target inhibitors for proteins associated with Alzheimer: in silico discovery using fragment-based descriptors. Curr Alzheimer Res, 2013, 10, 117-124. [134] Hieke, M.; Ness, J.; Steri, R.; Dittrich, M.; Greiner, C.; Werz, O.; Baumann, K.; Schubert- Zsilavecz, M.; Weggen, S.; Zettl, H. Design, synthesis, and biological evaluation of a novel class of gamma-secretase modulators with PPARgamma activity. J Med Chem, 2010, 53, 4691-4700.