* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Inflammatory Response
Adaptive immune system wikipedia , lookup
Immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Periodontal disease wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Inflammatory bowel disease wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Rheumatic fever wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Autoimmunity wikipedia , lookup
Atherosclerosis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Molecular mimicry wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Innate immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
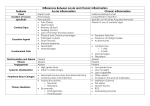
The Inflammatory Response A review The 3 Lines of Defense • FIRST line: Barrier protection – non-specific (treats each pathogen the same) – acts to prevent the pathogen from getting into the body – skin, mucous membranes, tears, sweat • SECOND line: Acts to destroy/inactivate a pathogen if it breaks the barriers of the first line – non-specific -phagocytic leukocytes – neutrophils and macrophages • THIRD line: Acts to destroy specific pathogens that are not destroyed/inactivated by the second line – specific – Lymphocytes – T cells, B cells The Inflammatory Response • Part of the second line of defense – The pathogen has gotten through the barrier protections and is in the tissues. Uh…oh! Splinter!!!! What’s happening? • Splinter (or pin) has broken through the barrier, carrying bacteria into the tissue. • Mast cells release histamine. • Macrophages that are in the tissue secrete chemical signals (cytokines) causes nearby capillaries to dilate and makes them more permeable (leaky). What’s happening? • Histamine released from mast cells cause more macrophages to enter from the blood stream. • Cytokines released from macrophages increase the blood flow to the site and “call” more neutrophils and antimicrobial peptides to the site. – now arrive and pass through the leaky capillaries into the tissue – ingest and kill the invader by phagocytosis and then fusion w/lysosomes • More blood redness, increase in temp, fluid leaks from the vessel into the tissue swelling What’s happening? • Neutrophils continue to digest the bacteria and cell debris. • Inflammation subsides and tissue begins to heal. Hooray for the Inflammatory Response!!! The Inflammatory Response is a GOOD thing, because it: • Prevents the spread of infection. • Helps remove pathogens and damaged tissues. But….there’s a dark side • What if the inflammatory response of the immune system is continually stimulated? …too much of a good thing For example, there can be different types of stimulants: 1)Infectious: unresolved viral or bacterial infection 2)Noninfectious: pollen, smoking, autoimmune reaction, obesity and tissue damage from wounds, tumors, heart disease, atherosclerosis and autoimmune disease This can lead to… Chronic Inflammation Chronic Inflammation is NOT a good thing: CI can lead to: Development of Type 2 diabetes, exacerbation of heart, liver and kidney disease, Alzheimer’s, some cancers (perhaps from increased mutational rate and enhanced angiogenesis), fibrosis What’s the difference between Acute Inflammation and Chronic inflammation? Acute inflammation: the normal Inflammatory response ●neutrophils dominate. ●you feel and see it (pain, redness, swelling, heat). ●Inflammatory cytokines are expressed and do their job and resolution occurs relatively quickly –it’s over and done with. Chronic inflammation (CI): ● macrophages dominate. ●T cells and B cells become involved. ●CI is silent—progresses without one even knowing it’s happening ●Persistent, increased expression of inflammatory cytokines. What are these cytokines? A trio of 3 proinflammatory cytokines always predominates. • IL-1 (interleukin -1) • IL-6 (interleukin -6) • TNF-α (tumor necrosis factor-alpha) What happens because of these cytokines? ● IL-1 – stimulated very early by macrophages – increases the permeability of capillaries – calls more neutrophils to the tissue ●IL-6 – secreted by T cells and macrophages – stimulates the inflammatory response – increases the production of neutrophils in the bone marrow ● TNF-α – activates macrophages – increases permeability of capillaries So secretion of these cytokines just continues the inflammatory process Reminder Why are we concerned about chronic inflammation? Recent studies have suggested that the constant secretion of these cytokines and stimulation of the inflammatory response can lead to…. • • • • • Type 2 diabetes Exacerbation of heart, liver and kidney disease Alzheimer’s disease Fibrosis of some tissues Some cancers HOW????? • Let’s briefly review how cells communicate with each other cell-signaling Three stages of Cell Signaling 1. RECEPTION – a signaling molecule binds to a SPECIFIC receptor protein molecule 2. TRANSDUCTION – This causes the receptor protein to change shape. Now the signal is changed into another form that the cell can recognize that will cause it to respond in a specific way. – This may occur in multiple steps called a CASCADE. 3. RESPONSE – The cell responds in a specific way and maybe the production of a particular protein. Reminder: Causes of chronic inflammation can be infectious or non-infectious Infectious: such as an unresolved viral or microbial infection, which results in continual immune stimulation • Example: Periodontitis from persistent dental infections • HOW?? -there is a constant source of bacteria – the immune system is constantly being required to try to rid the body of these bacteria constant inflammation Non infectious causes • pollen, smoking, pollution, autoimmune reaction and tissue damage from wounds that don’t heal, tumors, heart disease and atherosclerosis …… and……obesity! • Pollen and particles from smoking and pollution can constantly irritate certain tissues • Tissue damage from atherosclerosis, heart disease and wounds that don’t heal can constantly irritate certain tissues, as well. Huh?…OBESITY??? How can having too many adipocytes (fat cells) lead to a state of chronic inflammation? 1) Adipocytes can secrete IL-6 ..but that’s not the end of the story….. 2) excess free fatty acids bind to receptors on the adipocytes 3) cell signaling now leads to increase of the release of IL-6 So what can happen now? IL-6 then binds to receptors on the pancreatic beta cell …….. this prevents the cell from getting the signal to make insulin Result???? Type 2 Diabetes! If CI is “silent”, but dangerous, is there a way for someone to know if it’s happening in their body? Reminder: Inflammatory markers: • 1) IL-6 • 2) IL-1 • 3) TNF-α CI can be determined by measuring one of the inflammatory markers in a sample of their blood. THE ELISA We can determine if too much of the protein IL-6 is in someone’s blood by doing a laboratory test called an ELISA