* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hemoglobin
Minimal genome wikipedia , lookup
Genome evolution wikipedia , lookup
Biology and consumer behaviour wikipedia , lookup
Genetic engineering wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
X-inactivation wikipedia , lookup
Gene therapy wikipedia , lookup
Gene expression programming wikipedia , lookup
History of genetic engineering wikipedia , lookup
Epigenetics of human development wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Gene expression profiling wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Genome (book) wikipedia , lookup
Microevolution wikipedia , lookup
Designer baby wikipedia , lookup
Organisms at high altitude wikipedia , lookup
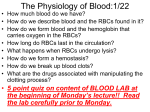
Hemoglobin Structure & Function HMIM224 Objectives of the Lecture 1- Understanding the main structural & functional details of hemoglobin as one of the hemoproteins. 2- Identify types & relative concentrations of normal adult hemoglobin with reference to HBA1c with its clinical application. 3- Recognize some of the main genetic & biochemical aspects of methemoglobinopathies with some implications on clinical features (with focusing on thalassemias). Hemoglobin is a globular hemoprotein • Hemeproteins are a group of specialized proteins that contain heme as a tightly bound prosthetic group. • Heme is a complex of protoporphyrin IX and ferrous iron (Fe2+) . • The iron is held in the center of the heme molecule by bonds to the four nitrogens of the porphyrin ring. • The heme Fe2+ can form two additional bonds, one on each side of the planar porphyrin ring. In myoglobin and hemoglobin, one of these positions is coordinated to the side chain of a histidine residue of the globin molecule, whereas the other position is available to bind oxygen Globin of hemoglobin is a globular protein with a quaternary structure Structure of heme Heme is a complex of protoporphyrin IX and ferrous iron (Fe2+). The iron is held in the center of the heme molecule by bonds of the four nitrogens of the protoporphrin ring. Heme F2+ can form two additional bonds, one on each side of the porphyrin ring. One of these positions is coordinated to the Side chain of histidine residue of the globin molecule, whereas the other position is available to bind oxygen. Structure & function of hemoglobin • Hemoglobin is found exclusively in RBCs. • Each day 6-7 g of Hb is synthesized to replace the heme lost through the normal turnover of erythrocytes . • Its main function is to transport oxygen from lungs to the tissues & carbon dioxide & hydrogen protons from tissues to lungs. • Hemoglobin A is the major hemoglobin in adults, is composed of four polypeptide chains, 2 alpha (a) & 2 beta (b) chains, held together by non-covalent interactions • Each subunit has stretches of a-helical structure & a heme binding pocket. Structure & function of hemoglobin (cont.) Structure & function of hemoglobin (cont.) Quaternary structure of hemoglobin: • The hemoglobin tetramer can be envisioned as being composed of two identical dimers, (αβ)1 and (αβ)2, in which the numbers refer to dimers one and two. • The two polypeptide chains within each dimer are tightly held together, primarily by hydrophobic interactions • In contrast, the two dimers are able to move with respect to each other, being held together primarily by polar bonds. • The weaker interactions between these mobile dimers result in the two dimers occupying different relative positions in deoxyhemoglobin as compared with oxyhemoglobin oxygenation & deoxygenation of hemoglobin (oxyhemoglobin & deoxyhemoglobin) Deoxyhemoglobin Taut structure Oxyhemoglobin Relaxed structure Types of adult hemoglobin 3–6 % HBA: HBA2: HBF: HBA1C : the major hemoglobin in humans first appears 12 weeks after birth- a minor component of normal adult HB normally synthesized only during fetal development has glucose residues attached to b-globin chains – increased amounts in DM Hemoglobin A1c (HBA1c) Some of hemoglobin A is glycosylated Extent of glycosylation depends on the plasma concentration of a particular hexose (as glucose). The most abundant form of glycosylated hemoglobin is HBA1c which has a glucose residues attached to b-globin chains in hemoglobin RBCs. Increased amounts of HBA1c are found in RBCs of patients with diabetes mellitus (DM). HbA1c could be used as a monitor for the control of the blood glucose level during the last 2 months for diabetic patients Hemoglobinopathies Hemoglobinopathies are members of a family of genetic disorders caused by: 1- Production of a structurally abnormal hemoglobin molecule (Qualitative hemoglobinopathies) Or: 2- Synthesis of insufficient quantities of normal hemoglobin (Quantitative hemoglobinopathies) Or: 3- both (rare). Thalassemias • Thalassemias are hereditary hemolytic diseases in which an imbalance occurs in the synthesis of globin chains. • They are most common single gene disorders in humans. • Normally, synthesis of a- and b- globin chains are coordinated, so that each a-globin chain has a b-globin chain partner. This leads to the formation of a2b2 (HbA). • In thalassemias, the synthesis of either the a- or b-globin chain is defective. Thalassemias (cont.) Thalassemia can be caused by a variety of mutations, including: 1- Entire gene deletions (whole gene is absent) Or: 2- Substitutions or deletions of one or more nucleotides in the DNA. Each thalassemia can be classified as either: 1- A disorder in which no globin chains are produced (ao- or bo -thalassemia) Or: 2- Some b-chains are synthesized, but at a reduced rate. (a+- or b+- thalassemia). Thalassemias (cont.) 1- b-thalassemias: Synthesis of b-globin chains are decreased or absent, whereas aglobin chain synthesis is normal. a-globin chains cannot form stable tetramers, and therefore a-chain precipitate causing premature death of RBCs. Accumulation of a2g2(HbF), a22 (Hb A2) also occurs. These factors end result in development of chronic anemia (hemolytic). Thalassemias (cont.) Some genetic aspects of thalassemia: There are only two copies of the b -globin gene in each cell (one on each chromosome 11). So, individuals with b -globin gene defects have either: 1- b-thalassemia minor (b -thalassemia trait): if they have only one defective b-globin gene. 2- b- thalassemia major (Cooley anemia): if both genes are defective. Thalassemias (cont.) Mutation in one of b-globin genes Mutation in both b-globin genes b-thalassemia minor b-thalassemia major Thalassemias (cont.) Some clinical aspects of thalassemias: 1- As b-globin gene is not expressed until late fetal gestation, the physical manifestations of b- thalassemias appear only after birth. 2- Individuals with b - thalassemias minor, make some b-chains, and usually require no specific treatment. 3- Infants born with b - thalassemias major seem healthy at birth, but become severely anemic during the first or second years of life. They require regular transfusions of blood. In these cases, bone marrow replacement therapy is recommended. Thalassemias (cont.) 2- a-thalassemia: Synthesis of a-globin chains is decreased or absent. Each individual's genome contains four copies of the a-globin (two on each chromosome 16), there are several levels of a-globin chain deficiencies Thalassemias (cont.) Types: If one of the four genes is defective the individual is termed a silent carrier of a- thalassemia as no physical manifestations of the disease occur. If two a-globin genes are defective, the individual is designated as having a-thalassemia trait. If three a-globin genes are defective; the individual has hemoglobin H (HbH) disease which is a mildly to moderately hemolytic anemia. Synthesis of unaffected g- and then b- globin chains continues, resulting in the accumulation of g tetramer in the newborn (g4, Hb Bart's) or b-tetramers (b4, HbH). The subunits do not show heme-heme interactions. So, they have very high oxygen affinities. Thus, they are essentially useless as oxygen carriers to tissues If four a-globin genes are defective, Hydrops fetalis & fetal death (death at birth), occurs as a-globin chains are required for the synthesis of HbF Thalassemias (cont.) Types of a-thalassemias Biochemistry of hemoglobin II Sickle cell anemia Definition: Sickle cell anemia is a genetic disorder of the blood caused by a single nucleotide alteration (a point mutation) in the b-globin gene. Inheritance of sickle cell anemia: Homozygous recessive disorder: Occurs in individuals who have inherited two mutant genes (one from each parent) that code for synthesis of the b chains of the globin molecule. RBCs of homozygous is totally HB S (a2bs2 ) Heterozygotes individuals: Have one normal and one sickle cell gene. RBCs of heterozygotes contain both HB S (a2bs2 ) & HB A (a2b2 ) Clinical manifestations of sickle cell anemia Homozygous individuals Clinical manifestations begin early in childhood With - Chronic hemolytic anemia - Lifelong episodes of pain & increased - Susceptibility to infection. - Acute chest syndrome - Stroke - Splenic & renal dysfunction - Bone changes due to bone marrow hyperplasia Heterozygote individuals Usually do not show clinical symptoms Amino acid substitution in HB S b chains HB S contains two mutant b-globin chains (bs ). In mutant chains, glutamate (polar) at position 6 is replaced with valine (nonpolar) resulting in: Formation of a protrusion on the b-globin that fit into a complementary site on the a chain of another hemoglobin molecule in the cell. In low oxygen tension, deoxy HB S polymerize inside the red blood cell leading to stiffening & distorting of the cell ending in production of rigid misshapen RBCs. Sickle cells block the flow of blood in narrow capillaries resulting in interruption of oxygen supply (localized anoxia) in tissues causing pains. Finally, cell death occurs due to anoxia (infarction) Also, RBCs of HB S have shorter life span than normal RBCs (less than 20 days, compared to 120 of normal) Hence, anemia is a consequence of HB S. Factors that increase sickling The extent of sickling is increased by any factor that increases the proportion of HB S in the deoxy state as in cases of 1- Decreased oxygen tension: in high altitudes flying in a nonpressurized plane 2- Increased pCO2 3- Decrease pH 4- Increased 2,3- BPG in RBCs Diagnosis of HB S Hemoglobin Electrophoresis HB S migrates more slowly towards anode (+ve electrode) than normal hemoglobin due to absence of negatively charged glutamate resulting in decrease of negativity of hemoglobin Selective advantage of the heterozygote state Heterozygotes individuals for sickle cell anemia are less susceptible to malaria caused by the parasite Plasmodium falciparum as their RBCs have shorter lifespan than normal , the parasite cannot complete its natural stage of development in RBCs. HB S gene is highly frequent in Africa in which malaria is also highly frequent. Methemoglobinemia • • • Methemoglobin results from oxidation of the ferrous ion (Fe2+) of heme of hemoglobin to ferric (Fe3+) ion. Methemoglobinemia is characterized by “chocolate cyanosis” i.e. brown-blue coloration of skin & membranes & chocolate colored blood. Causes of oxidation of ferrous ions: 1- Drugs as nitrates 2- Endogenous products (as reactive oxygen species ) 3- Inherited defects (as in certain mutations of a or b chains) 4- Deficiency of NADH-Met HB reductase :enzyme for reduction of Fe3+ of Met HB • RBCs of newborns have ½ capacity of adults to reduce Met HB & therefore they are more susceptible to Met HB formation by previous factors. • • Clinically, symptoms are due to tissue hypoxia Treatment: Methylene blue (to reduce the ferric ions) Assignments Methemoglobin Sickle cell anemia (Genetic, Biochemical & Clinical Aspects)