* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download SMU-DDE-Assignments-Scheme of Evaluation PROGRAM Bachelor
Adenosine triphosphate wikipedia , lookup
Catalytic triad wikipedia , lookup
Nicotinamide adenine dinucleotide wikipedia , lookup
Enzyme inhibitor wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Proteolysis wikipedia , lookup
Metalloprotein wikipedia , lookup
Peptide synthesis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Genetic code wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Citric acid cycle wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Amino acid synthesis wikipedia , lookup
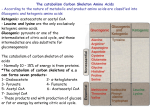
SMU-DDE-Assignments-Scheme of Evaluation PROGRAM SEMESTER SUBJECT CODE & NAME BK ID SESSION MARKS Q. No 1. A Bachelor/Diploma in Medical Imaging Technology II BMI 201 – Basics of Biochemistry B1947 WINTER 2015 60 Criteria (Unit 2, Page No. 29 - 32 ) 1 10 Define Amino acids. Amino acids are a group of organic compounds containing two functional groups namely amino and carboxyl. Amino group is basic while carboxyl group is acidic in nature. 9 Discuss the classification of amino acids: Classification based on structure: amino acids with aliphatic side (3+2+2+2) chains, amino acids containing hydroxyl group, sulphur containing amino acids, acidic amino acids, basic amino acids, aromatic amino acids and imino acids. Classification based on polarity: non polar amino acids, polar amino acids with no charge on R group, polar amino acids with positive R group, polar amino acids with negative R group. Nutritional classification: Essential or indispensable amino acids, Nonessential or dispensable amino acids. Classification based on their metabolic fate: glucogenic and ketogenic amino acids. List and explain the colour reaction of carbohydrates. A List the color reactions of carbohydrates : Molisch test Benedict’s test Benedict’s test after hydrolysis Barfoed’s test Selwinoff’s test Osazone formation Iodine formation Explain the color reactions of carbohydrates: Any four reactions A Total Marks Define Amino acids. Discuss the classification of amino acids. 2. 3. Marks (Unit 3, Page No. 65-70) 2 10 8 Discuss the classification of enzymes. Add a note on enzyme specificity. (Unit 5, Page No. 98-100) 6 10 Classification enzymes: Based on the chemical reaction catalyzed, enzymes are classified into six classes: SMU-DDE-Assignments-Scheme of Evaluation 4. A Oxidoreductases: catalyze the oxidation reduction reaction. Eg: LDH Trnasferases: catalyze the transfer of groups from one substrate into another. Eg: AST Hydrolases: catalyzes the breakdown of compounds by utilizing a molecule of water. Eg: Trypsin Lyases: catalyze the removal of a group from a substrate without using a molecule of water or combine two molecules to form a new molecule without using energy. Eg: Fumarase Isomerases: catalyze the isomerization of substrate. Eg: phosphohexose isomerase. Ligases: catalyse the reactions involving the joining together of two substrate using ATP as the energy source. Eg: DNA ligases 4 Specificity of enzymes: Stereospecificity: in this, enzyme exhibit steros specificity i.e., act only one isomer. Reaction specificity: same substance can undergo different types of reactions and each reaction is catalyzed by different enzymes. Substrate specificity: absolute substrate specificity: certain enzyme act only on one type of substrate. Relative substrate specificity: some enzyme act on structurally related substances. Broad specificity: certain enzyme act on closely related compounds. Explain the different glycogen storage disorders. Add a note on significance of glycogen metabolism. (Unit 8, Page No. 157 ) 7 10 Glycogen storage disorders: Type I: Von Gierke’s disease: The defective enzyme is glucose 6 phosphatase. The primary organ involved is liver. Features of this disease are hypoglycemia, lactic acidosis, hyperlipidemia, hyperuricemia and ketosis. Type II: Pompe’s disease: The defective enzyme is lysosomal acid maltase. All organs with lysosomes are affected. The main features are accumulation of glycogen in the lysosomes, cardiac failure and death in early life. Type III: Cori’s/ Forbes disease/ limit dextrinosis: The defective enzyme is debranching enzyme and the affected organs are mainly liver, skeletal and heart muscle. The features are hypoglycemia, accumulation of abnormal glycogen having short outer chains. Type IV: Andersen’s disease/ amylopectinosis: The defective enzyme is branching enzyme. The primary organ involved are liver, kidney and heart muscle. The features are accumulation of abnormal glycogen having a few branches, death due to cardiac and liver failure within 1 year of life. Type V: McArdle’s disease: the defective enzyme is muscle glycogen phosphorylase. The primary organ involved is skeletal muscle. The feature are exercise induced muscular pain, cramps, and decreased serum lactate after exercise. SMU-DDE-Assignments-Scheme of Evaluation 5. A Type VI: Her’s disease: The defective enzyme is liver glycogen phosphorylase. The primary organ involved is liver. The features are high content of liver glycogen, mild hypoglycemia and ketosis. Type VII: Tarui’s disease: The defective enzyme is phosphofructokinase in muscle and erythrocytes. The organs involved are muscle and RBCs. The features are exercise induced muscular pain, cramps, decreased serum lactate after exercise, hemolytic anemia. 3 Significance of glycogen metabolism: Liver glycogen functions to store and export glucose to maintain blood glucose level between meals. After 12-18 hours of fasting, liver glycogen is almost totally depleted. Muscle glycogen serves as a fuel reserve for the supply of ATP during muscle contraction. Although muscle glycogen doesn’t yield free glucose, pyruvate formed by glycolysis in muscle can undergo transamination to alanine, which is exported from muscle and used for gluconeogenesis in liver. Discuss the ketone body metabolism. (Unit 9, Page No. 222-225) 10 10 Ketone body metabolism: Ketone bodies are the water soluble compounds, which are produced as the by-products when fatty acids are broken down for energy. When the carbohydrate levels are too low, such as in the periods of prolonged fasting, the fat cells are utilized for the generation of energy. During this process, ketone bodies are produced as the byproducts. The compounds categorized as ketone bodies are acetone, acetoacetate and beta hydroxy butyrate. Ketone bodies are important sources of energy for the peripheral tissues because they are soluble in aqueous solution, and therefore, do not need to be incorporated into lipoproteins or carried by albumin as do the other lipids; they are produced in the liver during periods when the amount of acetyl CoA present exceeds the oxidative capacity of the live and they are used in proportion to their concentration in the blood by extra hepatic tissues, such as the skeletal and cardiac muscle and renal cortex. Formation of ketone bodies: The synthesis of ketone bodies occurs in the liver. The enzymes required for their synthesis are located in the liver mitochondria. During a fast, the liver is flooded with fatty acids mobilized from adipose tissue. The resulting elevated hepatic acetyl CoA produced primarily by fatty acid degradation inhibits pyruvate dehydrogenase, and activates pyruvate carboxylase. The OAA thus produced is used by the liver for gluconeogenesis rather than for the TCA cycle. Therefore, acetyl CoA is channeled into ketone body synthesis. Synthesis of 3-hydroxy-3-methylglutaryl (HMG) CoA: the SMU-DDE-Assignments-Scheme of Evaluation 6. A first synthetic step, formation of acetyl CoA, occurs by reversal of the thiolase reaction of fatty acid oxidation. Mitochondrial HMG CoA synthase combines a third molecule of acetyl CoA with acetoacetyl CoA to produce HMG CoA. HMG CoA synthase is the rate limiting step in the synthesis of ketone bodies, and is present in significant quantities only in the liver. Synthesis of the ketone bodies: HMG CoA is cleaved to produce acetoacetate and acetyl CoA. Acetoacetate can be reduced to form 3-hydroxybutyrate with NADH as the hydrogen donor. Acetoacetate can also spontaneously decarboxylate in the blood to form acetone- a volatile, biologically non-metabolized compound that can be released in the breath. The equilibrium between acetoacetate and 3hydroxybutyrate is determined by the NAD+/NADH ratio. Because this ratio is low during fatty acid oxidation, 3hydroxybutyrate synthesis is favored. Utilization of ketone bodies: 3-hydroxybutyrate is oxidized to acetoacetate by 3-hydroxybutyrate dehydrogenase, producing NADH. Acetoacetate is then provided with a CoA molecule taken from succinyl CoA by succinyl CoA: acetoacetate CoA transferase. This reaction is reversible, but the product acetoacetyl CoA, is actively removed by its conversion to two acetyl CoAs. Extra hepatic tissues, including the brain but excluding cells lacking mitochondria, efficiently oxidize acetoacetate and 3-hydroxybutyrate in this manner. In contrast, although the liver actively produces ketone bodies, it lacks thiophorase and, therefore, is unable to use ketone bodies as fuel. Excessive production of ketone bodies in diabetes mellitus: when the rate of formation of ketone bodies is greater than the rate of their use, their levels begin to rise in the bloodketonemia and eventually in the urine- ketonuria. These two conditions are seen most often in cases of uncontrolled, type I diabetes mellitus. In such individuals, high fatty acid degradation produces excessive amounts of acetyl CoA. It also depletes the NAD+ pool and increases the NADH pool, which slows the TCA cycle. This forces the excess acetyl CoA into the ketone body pathway. In diabetic individuals with severe ketosis, urinary excretion of the ketone bodies may be as high as 5000 mg/24 hr, and the blood concentration may reach 90 mg/dl. A frequent symptom of diabetic ketoacidosis is a fruity odour on the breath, which results from increased production of acetone. An elevation of the ketone body concentration in the blood results in academia. Explain the metabolic fate of ammonia. List the various genetic disorders associated with the urea cycle. (Unit 10,Page No. 241-244) 6 10 Metabolic fate of ammonia: Being highly toxic, ammonia should be eliminated or SMU-DDE-Assignments-Scheme of Evaluation detoxified from the body. Even a slight increase in the blood ammonia concentration is harmful to the brain. In human and primates, ammonia is transferred to liver, and converted to urea through urea cycle. Urea cycle: urea cycle is the process by which ammonia, a highly toxic substance is converted to a less toxic excretory waste product urea in liver. In the first step, ammonia is activated by ATP and it combines with CO2 to form carbamoyl phosphate. This reaction is catalyzed by carbamoyl phosphate synthetase-I enzyme, which requires N-acetyl glutamate as an allosteric activator. Ornithine transcarbamoylase transfers the carbamoyl group from carbamoyl phosphate to ornithine and produces citrulline. These first two reactions occur in the mitochondria. Rest of the reactions proceed in the cytosol. In the presence of argininosuccinate synthetase enzyme and ATP, citrulline combines with L-aspartate to form argininosuccinic acid. Subsequently, argininosuccinate lyase hydrolyses argininosuccinic acid to liberate arginine and fumaric acid. In the last step, arginine is hydrolyzed by arginase to form ornithine and urea. Ornithine again enters the urea cycle. The overall reaction of Urea cycle can be summarized as : NH3 + CO2 + Aspartate Urea + Fumarate Genetic disorders associated with urea cycle: Hyper ammonemia type I due to carbamoyl phosphate synthetase deficiency. Hyperammonemia type II due to ornithine transcarbamoylase Citrullinemia due to argininosuccinic acid synthetase Argininosuccinic aciduria due to argininosuccinase Hyperarginemia due to arginase. 4 *A-Answer Note –Please provide keywords, short answer, specific terms, specific examples (wherever necessary) ***********