* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Role of inducible NO synthase in cell signalling
Extracellular matrix wikipedia , lookup
Tissue engineering wikipedia , lookup
Cell culture wikipedia , lookup
Cell encapsulation wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Cellular differentiation wikipedia , lookup
Signal transduction wikipedia , lookup
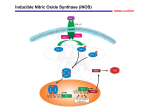
645 The Journal of Experimental Biology 202, 645–653 (1999) Printed in Great Britain © The Company of Biologists Limited 1999 JEB1881 REVIEW INDUCIBLE NO SYNTHASE: ROLE IN CELLULAR SIGNALLING KARL-FRIEDRICH BECK, WOLFGANG EBERHARDT, STEFAN FRANK, ANDREA HUWILER, UDO K. MEßMER, HEIKO MÜHL AND JOSEF PFEILSCHIFTER* Zentrum der Pharmakologie, Klinikum der Johann Wolfgang Goethe-Universität, Theodor-Stern-Kai 7, D-60590 Frankfurt am Main, Germany *e-mail: [email protected] Accepted 18 December 1998; published on WWW 17 February 1999 Summary The discovery of endothelium-derived relaxing factor intercellular messenger that acutely affects important and its identification as nitric oxide (NO) was one of the signalling pathways and, on a more long-term scale, most exciting discoveries of biomedical research in the modulates gene expression in target cells. These actions 1980s. Besides its potent vasodilatory effects, NO was will form the focus of the present review. found under certain circumstances to be responsible for the killing of microorganisms and tumour cells by activated macrophages and to act as a novel, Key words: nitric oxide synthase, cell signalling, isoform, inducible enzyme, apoptosis, nitric oxide, gene expression, guanylate cyclase, unconventional type of neurotransmitter. In 1992, Science protein kinase, protein phosphatase, transcription factor, redox picked NO as the ‘Molecule of the Year’, and over the past regulation. years NO has become established as a universal Introduction In mammals, the synthesis of NO is catalysed by nitric oxide synthase (NOS), which exists in at least three distinct isoforms (Nathan and Xie, 1994). NOS catalyses the oxidation of the amino acid L-arginine to give rise to citrulline and NO. Molecular cloning and sequence analysis has revealed the existence of three distinct NOS isotypes that are either constitutively expressed in endothelial cells (eNOS) and neurones (nNOS) or are induced (iNOS) by endotoxin and by inflammatory cytokines such as interleukin 1 (IL-1) or tumour necrosis factor α (TNF-α) in macrophages and many other cell types (Moncada et al., 1991; Nathan and Xie, 1994). iNOS requires a delay of 6–8 h before the onset of NO production but, once induced, this enzyme is active for hours to days and produces NO in 1000-fold larger quantities than the constitutive enzymes eNOS and nNOS. At low concentrations, NO stimulates guanylate cyclase activity and triggers the formation of cyclic GMP (cGMP), an important messenger mediating physiological functions of NO such as vascular homeostasis. Higher concentrations of NO produced by iNOS interact with thiol groups or transition-metalcontaining proteins and can alter protein function or initiate gene expression to protect cells. There is a continuous shift at even higher concentrations of NO towards cell damage or apoptosis, with other factors in the microenvironment of a cell critically influencing the final outcome (Brüne et al., 1998). Regulation of iNOS expression Two important observations were reported by different groups when working on iNOS expression. First, lipopolysaccharide (LPS) and interferon-γ (IFN-γ) are strong inducers of iNOS in monocytes, whereas the cytokines TNFα and IL-1β have, if any, only marginal effects. In contrast, most tissue-derived cells including hepatocytes, mesangial cells, vascular smooth muscle cells, myocytes and pancreatic β-cells, to name just a few, are more sensitive to the induction of iNOS when challenged with TNF-α or, in particular, with IL-1β. In nearly all cell types, LPS, IFN-γ, IL-1β and TNF-α enhance iNOS expression synergistically. Second, rodent cells can more easily be triggered to express iNOS than human cells. For example, IL-1β is a strong stimulus for iNOS transcription in rat mesangial cells (Pfeilschifter and Schwarzenbach, 1990), whereas in human mesangial cells considerable iNOS expression occurs only when combinations of cytokines were administered as a cocktail (Nicolson et al., 1993). Conflicting results were obtained concerning the role of cyclic AMP (cAMP) in iNOS expression. Whereas in rat vascular smooth muscle cells and rat mesangial cells, cAMP is a strong inducer of iNOS mRNA (Koide et al., 1993; Mühl et al., 1994; Kunz et al., 1994), cAMP reduces iNOS expression in other rodent cells. Recently, other stimulators of iNOS expression such as IL-2, IL-12, IL-18 and IFN-α have been described (Kröncke et al., 1995). Three main signalling pathways are thought to be 646 K.-F. BECK AND OTHERS responsible for iNOS expression. Induction of iNOS in murine macrophages is mediated by γ-activated sites and IFN-γresponsive elements in the iNOS promoter (Xie et al., 1993; Martin et al., 1994). In rat mesangial cells, binding of the nuclear factor κB (NF-κB) at the appropriate site on the iNOS promoter is essential for the induction of iNOS by IL-1β (Eberhardt et al., 1994, 1998). In contrast, endothelin-1 inhibits cytokine-induced iNOS expression without affecting NF-κB binding, suggesting additional mechanisms that are essential for cytokine-induced iNOS expression (Beck and Sterzel, 1996). For the induction of iNOS by cAMP, enhanced binding of the transcription factors CAAT/enhancer-binding protein (C/EBP) and cAMP-responsive element-binding protein (CREB) on the iNOS promoter has been reported (Eberhardt et al., 1998). Many inflammatory diseases are accompanied by an increase in NO production and, in appropriate animal models, a beneficial action of iNOS inhibitors has been demonstrated. Therefore, many groups are currently studying physiological or synthetic agents that inhibit cytokine-induced iNOS expression at the transcriptional level (Pfeilschifter et al., 1996). As a common theme, cytokine-induced iNOS expression is inhibited by agents that diminish activation or binding of NF-κB. This has been shown for a variety of pharmacological substances, including dithiocarbamates (Eberhardt et al., 1994), dexamethasone (Pfeilschifter and Schwarzenbach, 1990; Kunz et al., 1996) and cyclosporin A (Mühl et al., 1993; Kunz et al., 1995). These novel therapeutic approaches may provide new methods for treating inflammatory diseases associated with pathological NO overproduction. Soluble guanylate cyclase as a target of NO action The physiologically most relevant action of NO is the activation of soluble guanylate cyclase by nitrosation of its haem moiety (Ignarro, 1990). The subsequent increase in cGMP level alters the activity of three main target proteins: (i) cGMP-regulated ion channels, (ii) cGMP-regulated phosphodiesterases, and (iii) cGMP-dependent protein kinases (for a review, see Schmidt et al., 1993). The molecular basis of the sensory systems of visualization and olfaction is related to the action of cation channels which are regulated by cellular cGMP levels. These proteins have one binding site for cGMP. Binding of cGMP critically determines the function of these sensors. Activation of the vertebrate rod photoreceptor cells by light results in hydrolysis of cGMP. The drop in cellular cGMP concentration leads to closure of a cGMP-regulated cation channel with subsequent hyperpolarization of the cell; this is the primary neuronal response in visualization (Dhallan et al., 1992). Activation of odorant receptors in olfactory cilia is likely to be connected to an inositol-trisphosphate-mediated rise in intracellular Ca2+ concentration and activation of a constitutive NOS. NO increases cGMP levels in adjacent neurones, which in turn mediates further activation of the odorant signalling pathway by opening Ca2+ channels (Breer and Shephard, 1993). Phosphodiesterases play a key role in controlling the actions of the second messengers cAMP and cGMP. Of the six family members of phosphodiesterases, the enzyme activity of type II and type III proteins is directly regulated by binding of cGMP to conserved non-catalytic cGMP binding domains. Type II phosphodiesterases are stimulated by cGMP binding, whereas the type III enzymes are inhibited by cGMP. Therefore, cGMP can increase cAMP levels via activation of type III phosphodiesterase. In contrast, activation of type II enzymes increases cAMP hydrolysis and accordingly decreases cAMP concentrations (Schmidt et al., 1993). Two major classes of cGMP-dependent protein kinases have been identified, the soluble type I (GKI) and the membrane-bound type II (GKII) enzymes. GKI is further subdivided in α and β isoforms. GKI exists as a dimer, whereas GKII is a monomer. Protein analysis of GKI revealed a dimerization domain which includes an autophosphorylation and an autoinhibitory site, two cGMP binding domains and a catalytic domain. GKII is predominantly expressed in the intestinal epithelial brush border and is involved in intestinal Cl− absorption and secretion. GKI is expressed in various tissues, and its role in physiology is much better characterized. In myocytes, activation of GKI modulates contractility by inhibiting an inward Ca2+ current. In the kidney, GKI is expressed in different cell types such as mesangial cells, smooth muscle cells, microvascular pericytes and myofibroblasts. Functionally, it has been demonstrated that GKI regulates an amiloride-sensitive Na+ channel in the inner medullary collecting duct. In the cerebellum, GKI is highly expressed in Purkinje cells. However, its role in these cells is not yet clear. Furthermore, in smooth muscle cells and platelets, GKI inhibits agonist-induced elevations in Ca2+ concentration and thus modulates smooth muscle contraction and platelet activation (Schmidt et al., 1993). Protein kinases and phosphatases as targets of NO action The first evidence for an effect of NO on protein kinase cascades was reported by Lander et al. (1993a), who found that, in human peripheral blood mononuclear cells, NOgenerating compounds stimulated a membrane-associated protein tyrosine phosphatase activity which led to a dephosphorylation and activation of the src family protein tyrosine kinase p56lck, which is critically involved in T cell activation. These authors later showed that NO activates all three parallel mitogen-activated protein kinase (MAPK) cascades (Fig. 1) in Jurkat T cells, i.e. the stress-activated protein kinase/c-Jun N-terminal kinase (SAPK/JNK) cascade, the stress-activated p38 MAPK cascade and the classical ERK/MAPK cascade (Lander et al., 1996). A similar stimulatory effect of NO on the different MAPK cascades was observed in glomerular mesangial cells and endothelial cells Role of inducible NO synthase in cell signalling Fig. 1. NO modulation of signal flow in the three main mitogen-activated protein kinase (MAPK) pathways and the Janus kinase (JAK)/signal transducer and activator of transcription (STAT) cascade. Cdc42, a member of the Ras superfamily of small GTPbinding proteins; ERK, extracellular signalregulated kinase; IL-1, interleukin 1; JAK, Janus kinase; JNK, c-Jun N-terminal kinase; LPS, lipopolysaccharide; MAPK, mitogenactivated protein kinase; MAPKK, MAPK kinase; MAPKKK, MAPKK kinase; MEK, MAPK or ERK kinase; MEKK, MEK kinase; MKK, mitogen-activated protein kinase kinase; PAK, p21-activated protein kinase; p53, a tumour suppressing protein; R, receptor; RK, reactivating protein kinase; Rac, a member of the Ras superfamily of small GTP-binding proteins; Raf, a serine/threonine protein kinase; Ras, small GTP-binding protein; SAPK, stress-activated protein kinase; SEK, SAPK kinase; SMase, sphingomyelinase; STAT, signal transducer and activator of transcription; TAK, transforming growth factor β-activated protein kinase; TAO, thousand and one amino acid protein kinase; TNF, tumour necrosis factor. 647 Growth factors, NO Cytokines (TNF-α, IL-1) NO SMase Heat shock, IL-1, LPS NO R R Ras Rac/Cdc42 PAKs JAKs Raf MEKK1–3 MEK1/2 SEK1/MKK4 TAK1/TAO MKK3/6 MAPKKK MAPKK STATs ERK1/2 (Pfeilschifter and Huwiler, 1996; Callsen et al., 1998; A. Huwiler and J. Pfeilschifter, in preparation). Mechanistically, activation of the different MAPK cascades by NO may occur either by direct alterations to the kinases themselves or by modulation of an upstream factor such as the small GTP-binding protein p21ras (Lander et al., 1995; Yun et al., 1998). The activation of p21ras by NO was reported to be direct, reversible and initiated by S-nitrosylation of a critical cysteine residue of p21ras that stimulates guanine nucleotide exchange by interacting with a region of p21ras which normally interacts with guanine nucleotide exchange factors (GEFs) (Lander et al., 1995). Other potential direct targets for NO and upstream factors in the MAPK cascades are the heterotrimeric G-proteins. NO greatly enhanced GTPase activity of Gsα and Giα both in T cells and in vitro when pure recombinant proteins were used (Lander et al., 1993b). Alternatively, NO may directly modulate members of the different MAPK cascades and cause either activation or inhibition of the enzymes. The NO-releasing compound Snitrosoglutathione (GSNO) was found to cause S-nitrosylation and inactivation of the JNK2/SAPK cascade in vitro and may thereby exert its antiapoptotic effect in B-lymphocytes (So et al., 1998). Similarly, the NO-generating compound diethylenetriamine nitric oxide inhibits JNK activation in pheochromocytoma (PC12) cells (Park et al., 1996). Another family of protein kinases that plays a key role in several signal-transducing pathways is the family of protein kinase C (PKC) isoenzymes. Reactive oxygen species as well as NO have been reported to increase PKC activity (Klann et al., 1998). In contrast, NO was found to suppress PKC activity JNKs/SAPKs p38/RK MAPK Cell responses in mesangial cells (Gopalakrishna et al., 1993; Studer et al., 1996). However, neither of these studies gave any evidence for a direct effect of NO on the activation state of PKC. Recently, an additional class of protein kinases was shown to be directly modulated by NO in vitro and in vivo, the Janus kinases (JAKs). Both JAK2 and JAK3 autokinase activity were found to be inhibited by NO, presumably by oxidation of crucial dithiols to disulphides (Duhe et al., 1998). Such an inhibition of JAK activity in vivo may contribute to the immunosuppressive effects of NO because JAKs transmit signals from almost all types of cytokine receptors. Other possible targets for NO represent the family of protein phosphatases. By direct interaction with this class of enzyme, either an activation or inhibition of phosphatase activity may be achieved, and this will lead to increased or decreased phosphorylation of their target proteins which include, importantly, members of the different MAPK pathways. Activation of a membrane-bound phosphatase was reported in T cells (Lander et al., 1993a). Furthermore, protein tyrosine phosphatase activation was also observed in rat aortic smooth muscle cells (Kaur et al., 1998). In contrast, NO was reported to inactivate a low-molecular-mass protein tyrosine phosphatase in vitro by S-nitrosylation of two adjacent cysteine residues in the active site of the enzyme (Caselli et al., 1994). Comparable data were described recently for mesangial cells: NO was found directly to inhibit a tyrosine phosphatase activity, leading to increased phosphorylation and activation of the classical MAPKs (Callsen et al., 1998). However, the identity of this tyrosine phosphatase was not analysed further. Moreover, it has been 648 K.-F. BECK AND OTHERS reported that NO leads to an induction of MAPK phosphatase-1 (MKP-1) mRNA in human embryonic lung fibroblasts, which would suggest an increased MKP activity and conversely a decreased MAPK activity in these cells (Marquis and Demple, 1998). In conclusion, these studies suggest that NO can, in principle, deliver signals into all the major MAPK cascades including the classical ERK, SAPK/JNK and p38 kinase cascades as well as the JAK/signal transducer and activator of transcription (STAT) pathway. An integration of signals will lead to cell-type-specific responses that critically depend on interactions between the individual constituents of a cell and the components of the different signalling cascades. These cascade events then trigger the phosphorylation of key nuclear proteins, including transcription factors such as c-Jun, ternary complex factors or STATs and, finally, perhaps lead to alterations in gene expression. Modulation of transcription factors and gene expression by NO The molecular mechanisms by which NO affects gene expression are still poorly understood, and an ultimate ‘NOresponsive promoter element’ has yet to be identified. However, increasing evidence is accumulating that NO preferentially alters transcription factors that are sensitive to changes in the cellular oxidation–reduction (redox) status. At least two well-defined transcription factors, NF-κB and activator protein 1 (AP-1) were shown to be regulated by the intracellular redox state (Sen and Packer, 1996). NO is a molecule with both anti-oxidant and pro-oxidant properties depending on the availability and concentration of potential reaction partners such as superoxide and hydrogen peroxide or other reactive oxygen species (ROS). This may explain the disparate observations that in some cells, including human blood mononuclear cells and rat glomerular mesangial cells, treatment with NO donors such as sodium nitroprusside (SNP), S-nitroso-N-acetylpenicillamine (SNAP) and GSNO resulted in enhanced binding activity of NF-κB family members (Lander et al., 1993a; W. Eberhardt, unpublished results), whereas in other cell types activation of NF-κB binding following cytokine treatment could be inhibited by treatment with NO donors (Peng et al., 1995). Endogenous NO may function to scavenge reactive oxygen intermediates, thereby inhibiting activation of NF-κB, as has been shown for the expression of genes coding for monocyte chemoattractant protein 1 (MCP-1) and macrophage colony stimulating factor 1 (CSF-1) (Zeiher et al., 1994; Peng et al., 1995). However, a universal hypothesis for activation of NF-κB by ROS seems uncertain and may be restricted to specific cell types (Brennan and O’Neill, 1995). Alternative mechanisms for NF-κB inhibition by NO include increased expression and nuclear translocation of inhibitor protein IκBα, as demonstrated for VCAM-1 gene expression in human endothelial cells (Spiecker et al., 1997). A direct inhibition of the DNA-binding activity of NF-κB family proteins by NO has been demonstrated in vitro using recombinant p50/p65 proteins (Matthews et al., 1996). It was observed that NO modifies a conserved cysteine residue within the N-terminal region of the transcription factor thought to be responsible for DNA binding, dimerization and nuclear translocation. A direct in vitro modification of transcriptional activators has also been demonstrated for AP-1 (Tabuchi et al., 1994). Single conserved cysteine residues within the DNA-binding domains of c-Fos and c-Jun, the major components of AP-1, seem to be responsible for redox regulation of AP-1 activity. Nitrosylation of critical cysteines by NO may account for the increase in junB and c-fos gene expression observed in some mammalian cell types. Generally, protein modifications may reflect a common mechanism for the activation of the phorbol ester 12-O-tetradecanoylphorbol-13-acetate (TPA) responsive element (TRE)-containing gene promoters by NO-releasing agents and by cGMP analogues (Pilz et al., 1995). Other molecular mechanisms by which NO may directly influence transcription factors involve the destruction of zinc–sulphur clusters and the release of zinc from metallothioneins, thereby inhibiting zinc-finger-type transcription factors. NO-mediated nitrosylation of the zincfinger domains results in the formation of disulphide bonds and the loss of in vitro DNA binding capacity, as demonstrated for the yeast transcription factor LAC9 (Kröncke et al., 1994). It seems quite plausible that NO may affect mammalian zincfinger transcription factors in a similar way. During the last few years, an increasing number of genes have been shown to be under regulatory control by nitric oxide, including those for extracellular matrix proteins (Chatziantoniou et al., 1998) and the corresponding proteases (Sasaki et al., 1998), growth factors (Sasaki et al., 1998; Tsurumi et al., 1997; Chin et al., 1997), cytokines (VanDervort et al., 1994), chemokines (Villarete and Remick, 1995; Mühl and Dinarello, 1997), receptors (Ichiki et al., 1998), enzymes (Hartsfield et al., 1997; Mühl and Pfeilschifter, 1995) or even hormones (Wang et al., 1998). The gene for interleukin-8 (IL-8) has been revealed to be under transcriptional control by NO. In human endothelial cells, TNF-α-stimulated IL-8 production was inhibited by the NOS inhibitor (L)-NG-nitroarginine methylester (L-NAME) in a dose-dependent manner. Moreover, exogenously added NO donors induced IL-8 expression in these cells (Villarete and Remick, 1995). Besides IL-8, TNF-α is likely to be induced in a paracrine manner by endothelial and smooth-muscle-derived NO in human neutrophils (VanDervort et al., 1994). Furthermore, expression of macrophage inflammatory protein 1α (MIP-1α), another member of the chemokine family, was directly dependent on lipopolysaccharide-induced NO synthesis in peripheral blood mononuclear cells (Mühl and Dinarello, 1997). Another group of target genes for NO action has been detected recently: the extracellular matrix proteins and their degrading enzymes, the matrix metalloproteinases (MMPs). In the kidney, accumulation of extracellular matrix is often a hallmark of chronic diseases eventually leading to the Role of inducible NO synthase in cell signalling development of glomerulosclerosis. Within this pathological process, NO triggers the inhibition of collagen type I gene expression in afferent arterioles and glomeruli. Hypertensive transgenic mice harbouring a luciferase reporter gene under the control of the collagen I-α2 chain promoter revealed a pronounced four- to tenfold increase in promoter activity and subsequent deposition of collagen I in the afferent arterioles and glomeruli, respectively, in the presence of systemically applied L-NAME (Chatziantoniou et al., 1998). Furthermore, IL-1β-stimulated MMP-9 expression is triggered via an autocrine NO loop in articular chondrocytes (Sasaki et al., 1998). Regulation of vascular endothelial growth factor (VEGF), a growth factor mediating angiogenesis and vascular permeability, was found to be modulated by NO. VEGF is upregulated in smooth muscle cells of arterial walls in response to endothelial injury. This up-regulation is inhibited by NO donors known to interfere with the binding of AP-1 to the VEGF promoter. This mechanism constitutes a negative feedback loop in which NO released from the restored endothelium shuts off VEGF expression (Tsurumi et al., 1997). The development of a new blood vessel network connected to the circulation is a crucial stage in tumour growth. VEGF expression is induced by NO-donating agents in glioblastoma and hepatocarcinoma cells. For both cell lines, however, NOinduced gene expression is mediated through the activation of guanylate cyclase (Chin et al., 1997). Finally, NO is even able to trigger transcription of its own biosynthetic machinery: it was found to increase IL-1βinduced iNOS gene expression at the transcriptional level in mesangial cells. Inhibition of NO synthesis clearly reduced IL1β-stimulated iNOS expression, suggesting that NO functions in a positive feedback loop that speeds up and strengthens its own biosynthesis (Mühl and Pfeilschifter, 1995). This potent amplification mechanism may form the basis for the excessive formation of NO in acute and chronic inflammatory diseases. Powerful negatively acting regulatory pathways are required to terminate amplification loops such as the one described above. The most direct way to suppress NO-triggered amplification of iNOS expression is by substrate depletion. Moreover, NO can initiate apoptotic cell death in glomerular mesangial cells and various other cell types (Mühl et al., 1996; Pfeilschifter and Huwiler, 1996; Sandau et al., 1997; Brüne et al., 1998). This may provide a delayed shut-off mechanism for the production of NO by mesangial cells. Apopotosis: cell signalling by redox regulation Although ‘nitric oxide’ was treated as equivalent to NO• under physiological conditions and with regard to therapeutic aspects using various NO donors, NO can be interconverted among different redox forms such as the nitrosonium cation (NO+), the nitric oxide free radical (NO•) and the nitroxyl anion (NO−), each with distinctive chemistry (Stamler, 1994). Moreover, from a biological standpoint, the various and rapid reactions of NO with oxygen, e.g. the reaction of NO with O2− 649 in aqueous solution yielding peroxynitrite (ONOO−), and with metal ions determine its ability to modulate signal transduction. With respect to the complex NO redox chemistry, innumerable studies have been undertaken to elucidate the molecular switching mechanisms that transduce the chemical (radical) signal into a functional cell response. NO-responsive signalling proteins (transcription factors, enzymes, receptors, ion channels) are usually characterized by the existence of thiol and tyrosine residues strategically located at either allosteric or active sites. Modification of thiol residues by NO resulting in the formation of S-nitrosothiols has been described for many different enzymes, such as the glycolytic enzyme glyceraldehyde-3-phosphate dehydrogenase (GAPDH), and signal transduction components, such as the ras oncogene product p21 (p21ras), and PKC predominantly inhibits its enzymatic activities (see above). Regulation of GAPDH by NO and ONOO− received attention because endogenously released NO as well as NO supplied by NO donors stimulated Snitrosylation of GAPDH (Mohr et al., 1994). This modification subsequently resulted in the transfer and covalent binding of NADH to the cysteine residue accompanied by the inhibition of enzymatic activity in vitro and in vivo (Dimmeler et al., 1994; Meßmer and Brüne, 1996a) and an alteration in intracellular distribution (Meßmer and Brüne, 1996a; Galli et al., 1998). Comparably, signalling components were differentially regulated by NO and its oxidation products through S-nitrosylation. The biological activity of PKC and the transcription factor AP-1 were blocked by a high-output NO synthase, whereas NO induced activation of the pertussistoxin-sensitive G protein and p21ras (see above). In addition to S-nitrosylation, nitration of tyrosine residues is another class of reaction through which NO and ONOO− influence signal transduction. Although many proteins contain tyrosine residues, factors such as the nature of the nitrating agents (NO, ONOO−, NO2•, etc.), protein folding and the presence of glutamate in the local environment may serve as markers for tyrosine nitration rather than simply the number of tyrosine residues (Ischiropoulos, 1998). One important in vivo target reported recently is the mitochondrial manganese superoxide dismutase (Mn-SOD). In contrast to Cu/Zn-SOD, which lacks tyrosine residues and therefore is not a target for nitration, Mn-SOD enzymatic activity is blocked by the exclusive nitration of Tyr 34 (Yamakura et al., 1998). Similarly, prostacyclin synthase (Zou et al., 1997), neurofilament L, actin and several other substrates have been identified as in vivo protein targets. In addition to protein nitration, N-nitrosation of DNA occurs when NO is released in large amounts, and this reaction is considered to be a potential toxic mechanism of NO• and other NO redox forms (Stamler, 1994). The role in cell signalling of NO•- and NO•/O2−-derived congenitors has been intensively studied for apoptotic cell death. Since 1993, many different groups have described the induction of apoptotic cell death following iNOS induction or exogenous application of NO donors in different cell types such as macrophages, mesangial cells and neurones (Brüne et 650 K.-F. BECK AND OTHERS al., 1998). Cell death by apoptosis is highly organized and follows a universal pattern characterized by chromatin condensation, DNA cleavage by an active endonuclease, cell shrinkage, membrane blebbing and redistribution of phosphatidylserine from the inner to the outer leaflet of the cell membrane, an important mechanism for the recognition of apoptotic cells by surrounding phagocytes. Following the initial observations that endogenously derived NO• and the application of various NO donors (e.g. SNP, GSNO) caused apoptotic manifestations in different in vitro models, important signalling pathways that provide mechanistic insights were characterized in the mouse RAW 264.7 macrophage cell line. One of the first signals to be established in NO-mediated cell death was an accumulation of the tumour suppressor p53 (Meßmer et al., 1994). p53 accumulation occurred as an early response following iNOS activation or NO donor treatment and resulted from a decreased rate of protein degradation (Meßmer and Brüne, 1996b). Initially described in RAW 264.7 macrophages, the requirement for p53 has been confirmed in several other cellular systems (Brüne et al., 1998). The accumulation of p53, an established guardian of the genome, reflects DNA damage as an ultimate result of high levels of NO production and places oxidative and nitrosative DNA damage into the early apoptotic pathways. Following p53 accumulation, activation of caspases was described in NOmediated apoptosis (Meßmer et al., 1998). Caspases are a family of cysteine proteases that assist in apoptotic cell death by cleaving distinct cellular proteins such as the poly(ADPribose) polymerase (PARP), lamin, PKC-δ and MAPK kinase (MEK) kinase 1 (MEKK1), which are subsequently selectively inactivated or activated. PARP cleavage and caspase-3 activation, but not p53 upregulation, were prevented by Bcl-2 gene transfer (Meßmer et al., 1996). It is important to note that different cells vary greatly in their sensitivity to NO, and in this context the response of a cell can be modulated by the simultaneous release of oxygen radicals. For example, glomerular mesangial cells (Fig. 2) respond to NO donor treatment with an induction of apoptosis, as do RAW 264.7 macrophages, but in contrast to macrophages, mesangial cells remain highly resistant to iNOS induction by IL-1β (Nitsch et al., 1997). Whether endogenously produced NO can fulfill the function of an apoptosis inducer may critically depend on a balance between the reactive nitrogen and oxygen species produced by mesangial cells. Appropriate generation of O2− simultaneously with NO will therefore block NO-donor-induced apoptosis in mesangial cells (Sandau et al., 1997). Disturbing the NO/O2− balance by superinduction of IL1β-mediated NO release by basic fibroblast growth factor may therefore be associated with increased mesangial cell apoptosis (Kunz et al., 1997). Assuming that the simultaneous generation of NO/O2− would result in ONOO− formation, we suggest that the production of ONOO− represents a protective mechanism. Supporting evidence comes from detailed experiments using RAW 264.7 macrophages (Brüne et al., 1997), although contradictory reports describe ONOO− as an inducer of apoptotic cell death (Beckman and Koppenol, 1996). Although NO is established as a potent inducer of apoptosis in certain cell types, contradictory effects have been reported, with NO displaying anti-apoptotic effects in lymphocytes, Bcells, eosinophils, hepatocytes and endothelial cells (for a review, see Dimmeler and Zeiher, 1997). One major difference from the apoptosis-inducing system is the amount of NO required for these anti-apoptotic effects. Anti-apoptotic activities of NO were observed at concentrations that are only 2–10 % of those needed for the induction of apoptosis (Haendeler et al., 1997). Most interesting, but yet unresolved, are the precise mechanisms responsible for the anti-apoptotic effects of NO. Several groups reported and favoured a direct inhibition of caspases by reversible S-nitrosylation and therefore an interaction between NO•- and NO•/O2−-derived congenitors and the executioners of apoptotic signal transduction (Li et al., 1997; Haendeler et al., 1997; Dimmeler TGF- β PDGF Steroids, CsA Epithelial cells Fig. 2. Schematic representation of the inflammatory process in glomerulonephritis, focusing on the role of NO generated by glomerular mesangial cells and macrophages. bFGF, basic fibroblast growth factor; C/EBP, CCAAT/enhancer binding protein family of transcription factors; CsA, cyclosporin A; IFN-γ, interferon-γ; IL-1, interleukin 1; iNOS, inducible nitric oxide synthase; LPS, lipopolysaccharide; NF-κB, nuclear factor κB; PDGF, platelet-derived growth factor; TGF, transforming growth factor; TNF, tumour necrosis factor. IL-1 + TNF-α + bFGF + Forskolin LPS +IFN-γ NF-κ B C/EBP DNA mRNA iNOS NO Mesangial cells DNA Endothelial cells iNOS Macrophages TNF-α LPS Role of inducible NO synthase in cell signalling and Zeiher, 1997). Although a tempting hypothesis, questions remain as to the in vivo relevance of S-nitrosylation of caspases by NO. Uncertainties arise from differences between purified enzymes or cytosolic cell extracts under strong reducing conditions and the microenvironment of the enzymes in an intact cell. Furthermore, there are striking differences in NO donor concentrations required for in vitro S-nitrosylation of crude caspases, which are 100- to 1000-fold higher than those needed for cell culture experiments (Haendeler et al., 1997). In general, one should consider that inhibition of an apoptotic signalling cascade upstream of caspases will also prevent caspase activation. Therefore, stress responses, induction of heat-shock proteins and defence enzymes, such as Mn-SOD or Cu/Zn-SOD, and activation of anti-apoptotic signalling components provide alternative mechanisms for cell protection. This debate highlights the fact that NO is a double-edged sword which, when produced in small amounts, by the constitutively expressed NOS isoenzymes, exerts a protective effect. However, a high output of NO by the inducible iNOS may exert deleterious effects. Moreover, it is worth mentioning that the cellular responses of cells that produce NO constitutively, e.g. endothelial cells, can differ markedly from those of cells that do not (Harrison, 1997). Perspectives Since the initital report of NO activity (Furchgott and Zawaski, 1980), enormous progress has been made over the last two decades in the field of NO research. Whereas most physiological responses triggered by moderate concentrations of NO are mediated by activation of soluble guanylate cyclase and the subsequent production of cGMP as the principal signalling messenger, recent studies have provided a wealth of evidence for alternative signalling pathways in which concentrations of NO are high. These signals operate in part through redox-sensitive regulation of transcription factors and gene expression and alter, on a more long-term basis, the capacity of a cell to deal with stress conditions. Crosscommunication with other pro-oxidant or anti-oxidant mediators will critically influence the fate of a cell under pathological conditions when iNOS is expressed. It will be an exciting challenge to unravel this delicate network of interactions to yield the desired mechanistic insights needed for the development of efficacious novel therapies. The work of the authors was supported by the Deutsche Forschungsgemeinschaft (SFB 553) and the Commission of the European Union (Biomed 2, PL950979). References Beck, K. F. and Sterzel, R. B. (1996). Cloning and sequencing of the proximal promoter of the rat iNOS gene: activation of NFκB is not sufficient for transcription of the iNOS gene in rat mesangial cells. FEBS Lett. 394, 263–267. 651 Beckman, J. S. and Koppenol, W. H. (1996). Nitric oxide, superoxide and peroxynitrite: the good, the bad and the ugly. Am. J. Physiol. 271, C1424–C1437. Breer, H. and Shepherd, G. M. (1993). Implications of the NO/cGMP system for olfaction. Trends Neurosci. 1, 5–9. Brennan, P. and O’Neill, L. A. J. (1995). Effects of oxidants and antioxidants on nuclear factor κB activation in three different cell lines: evidence against a universal hypothesis involving oxygen radicals. Biochim. Biophys. Acta 1260, 167–175. Brüne, B., Götz, C., Meßmer, U. K., Sandau, K., Hirvonen, M. R. and Lapetina, E. G. (1997). Superoxide formation and macrophage resistance to nitric oxide mediated apoptosis. J. Biol. Chem. 272, 7253–7258. Brüne, B., von Knethen, A. and Sandau, K. B. (1998). Nitric oxide and its role in apoptosis. Eur. J. Pharmac. 351, 261–272. Callsen, D., Pfeilschifter, J. and Brüne, B. (1998). Rapid and delayed p42/p44 MAPK activation by nitric oxide: the role of cGMP and tyrosine phosphatase inhibition. J. Immunol. 161, 4852–4858. Caselli, A., Camici, G., Manao, G., Moneti, G., Pazzagali, L., Cappugi, G. and Ramponi, G. (1994). Nitric oxide causes inactivation of the low molecular weight phosphotyrosine protein phosphatase. J. Biol. Chem. 269, 24878–24882. Chatziantoniou, C., Boffa, J. J., Ardaillou, R. and Dussaule, J. C. (1998). Nitric oxide inhibition induces early activation of type I collagen gene in renal resitance vessels and glomeruli in transgenic mice. J. Clin. Invest. 101, 2780–2789. Chin, K., Kurashima, Y., Ogura, T., Tajiri, H., Yoshida, S. and Esumi, H. (1997). Induction of vascular endothelial growth factor by nitric oxide in human glioblastoma and hepatocellular carcinoma cells. Oncogene 15, 437–442. Dhallan, R. S., Macke, J. P., Eddy, R. L., Shows, T. B., Reed, R. R., Yau, K.-W. and Nathans, J. (1992). Human rod photoreceptor cGMP-gated channel: amino acid sequence, gene structure and functional expression. J. Neurosci. 12, 3248–3256. Dimmeler, S., Meßmer, U. K., Tiegs, G. and Brüne, B. (1994). Modulation of glyceraldehyde-3-phosphate dehydrogenase in Salmonella abortus equi lipopolysaccharide-treated mice. Eur. J. Pharmac. Mol. Pharmac. 267, 105–112. Dimmeler, S. and Zeiher, A. M. (1997). Nitric oxide and apoptosis: another paradigm for the double-edged role of nitric oxide. Nitric Oxide: Biol. Chem. 1, 275–281. Duhe, R. J., Evan, G. A., Erwin, R. A., Kirken, R. A., Cox, G. W. and Farrar, W. L. (1998). Nitric oxide and the redox regulation of Janus kinase activity. Proc. Natl. Acad. Sci. USA 95, 126–131. Eberhardt, W., Kunz, D. and Pfeilschifter, J. (1994). Pyrrolidine dithiocarbamate differentially affects interleukin 1 beta- and cAMP-induced nitric oxide synthase expression in rat renal mesangial cells. Biochem. Biophys. Res. Commun. 200, 163–170. Eberhardt, W., Plüss, C., Hummel, R. and Pfeilschifter, J. (1998). Molecular mechanisms of inducible nitric oxide synthase gene expression by IL-1β and cAMP in rat mesangial cells. J. Immunol. 160, 4961–4969. Furchgott, R. F. and Zawadski, J. V. (1980). The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 288, 373–376. Galli, F., Rovidati, S., Ghibelli, L. and Canestrari, F. (1998). SNitrosylation of glyceraldehyde-3-phosphate dehydrogenase decreases the enzyme affinity to the erythrocyte membrane. Nitric Oxide: Biol. Chem. 2, 17–27. Gopalakrishna, R., Chen, Z. H. and Gundimeda, U. (1993). Nitric 652 K.-F. BECK AND OTHERS oxide and nitric oxide-generating agents induce a reversible inactivation of protein kinase C activity and phorbol ester binding. J. Biol. Chem. 268, 27180–27185. Haendeler, J., Weiland, U., Zeiher, A. M. and Dimmeler, S. (1997). Effects of redox-related congeners of NO on apoptosis and caspase-3 activity. Nitric Oxide: Biol. Chem. 1, 282–293. Harrison, D. G. (1997). Cellular and molecular mechanisms of endothelial dysfunction. J. Clin. Invest. 100, 2153–2157. Hartsfield, C. L., Alam, J., Cook, J. L. and Choi, A. M. (1997). Regulation of heme oxygenase-1 gene expression in vascular smooth muscle cells by nitric oxide. Am. J. Physiol. 273, L980–L988. Ichiki, T., Usui, M., Kato, M., Funakoshi, Y., Ito, K., Egashira, K. and Takeshita, A. (1998). Downregulation of angiotensin II type 1 receptor gene transcription by nitric oxide. Hypertension 31, 342–348. Ignarro, J. J. (1990). Biosynthesis and metabolism of endotheliumderived nitric oxide. Annu. Rev. Pharmac. Toxicol. 30, 535–560. Ischiropoulos, H. (1998). Biological tyrosine nitration: a pathophysiological function of nitric oxide and reactive oxygen species. Arch. Biochem. Biophys. 356, 1–11. Kaur, K., Yao, J., Pan, X., Matthews, C. and Hassid, A. (1998). NO decreases phosphorylation of focal adhesion proteins via reduction of Ca in rat aortic smooth muscle cells. Am. J. Physiol. 274, H1613–H1619. Klann, E., Roberson, E. D., Knapp, L. T. and Sweatt, J. D. (1998). A role for superoxide in protein kinase C activation and induction of long-term potentiation. J. Biol. Chem. 273, 4516–4522. Koide, M., Kawahara, Y., Nakayama, I., Tsuda, T. and Yokoyama, M. J. (1993). CAMP-elevating agents induce an inducible type of nitric oxide synthase in cultured vascular smooth muscle cells. J. Biol. Chem. 268, 24959–24966. Kröncke, K. D., Fehsel, K. and Kolb-Bachofen, V. (1995). Inducible nitric oxide synthase and its product nitric oxide, a small molecule with complex biological activities. Biol. Chem. HoppeSeyler 376, 327–343. Kröncke, K. D., Fehsel, K., Schmidt, T., Zenke, F. T., Dasting, I., Wesener, J. R., Bettermann, H., Breunig, K. D. and KolbBachofen, V. (1994). Nitric-oxide destroys zinc–sulfur clusters inducing zinc release from metallothionein and inhibition of the zinc finger-type yeast transcription activator LAC9. Biochem. Biophys. Res. Commun. 200, 1105–1110. Kunz, D., Mühl, H., Walker, G. and Pfeilschifter, J. (1994). Two distinct pathways trigger the expression of inducible nitric oxide synthase in rat renal mesangial cells. Proc. Natl. Acad. Sci. USA 91, 5387–5391. Kunz, D., Walker, G., Eberhardt, W., Messmer, U. K., Huwiler, A. and Pfeilschifter, J. (1997). Platelet-derived growth factor and fibroblast growth factor differentially regulate interleukin 1β- and cAMP-induced nitric oxide synthase expression in rat renal mesangial cells. J. Clin. Invest. 100, 2800–2809. Kunz, D., Walker, G., Eberhardt, W., Nitsch, D. and Pfeilschifter, J. (1995). Interleukin 1β-induced expression of nitric oxide synthase in rat renal mesangial cells is suppressed by cyclosporin A. Biochem. Biophys. Res. Commun. 216, 438–446. Kunz, D., Walker, G., Eberhardt, W. and Pfeilschifter, J. (1996). Molecular mechanisms of dexamethasone inhibition of nitric oxide synthase expression in interleukin 1β-stimulated mesangial cells: evidence for the involvement of transcriptional and posttranscriptional regulation. Proc. Natl. Acad. Sci. USA 93, 255–259. Lander, H. M., Jacovina, A. T., Davis, R. J. and Tauras, J. M. (1996). Differential activation of mitogen-activated protein kinases by nitric-oxide-related species. J. Biol. Chem. 271, 19705–19709. Lander, H. M., Ogiste, J. S., Paerce, S. F. A., Levi, R. and Novogrodsky, A. (1995). Nitric oxide-stimulated guanine nucleotide exchange on p21ras. J. Biol. Chem. 270, 7017–7020. Lander, H. M., Sehajpal, P., Levine, D. M. and Novogrodsky, A. (1993a). Activation of human peripheral blood mononuclear cells by nitric oxide-generating compounds. J. Immunol. 150, 1509–1516. Lander, H. M., Sehajpal, P. K. and Novogrodsky, A. (1993b). Nitric oxide signaling: a possible role for G proteins. J. Immunol. 151, 7182–7187. Li, J., Billiar, T. R., Talanian, R. V. and Kim, Y. M. (1997). Nitric oxide reversibly inhibits seven members of the caspase family via S-nitrosylation. Biochem. Biophys. Res. Commun. 240, 419–424. Marquis, J. C. and Demple, B. (1998). Complex genetic response of human cells to sublethal levels of pure nitric oxide. Cancer Res. 58, 3435–3440. Martin, E., Nathan, C. and Xie, Q. W. (1994). Role of interferon regulatory factor 1 in induction of nitric oxide synthase. J. Exp. Med. 180, 977–984. Matthews, J. R., Botting, C. H., Panico, M., Morris, H. R. and Hay, R. T. (1996). Inhibition of NF-κB DNA binding by nitric oxide. Nucleic Acids Res. 24, 2236–2242. Meßmer, U. K., Ankarcrona, M., Nicotera, P. and Brüne, B. (1994). p53 expression in nitric oxide-induced apoptosis. FEBS Lett. 355, 23–26. Meßmer, U. K. and Brüne, B. (1996a). Modification of macrophage glyceraldehyde-3-phosphate dehydrogenase in response to nitric oxide. Eur. J. Pharmac. 302, 171–182. Meßmer, U. K. and Brüne, B. (1996b). Nitric oxide-induced apoptosis: p53-dependent and p53-independent signalling pathways. Biochem. J. 319, 299–305. Meßmer, U. K., Reed, J. C. and Brüne, B. (1996). Bcl-2 protects macrophages from nitric oxide-induced apoptosis. J. Biol. Chem. 271, 20192–20197. Meßmer, U. K., Reimer, D. M. and Brüne, B. (1998). Protease activation during nitric oxide-induced apoptosis: Dissection between PARP and U1-70kDa cleavage. Eur. J. Pharmac. 349, 333–343. Mohr, S., Stamler, J. S. and Brüne, B. (1994). Mechanisms of covalent modification of glyceraldehyde-3-phosphate dehydrogenase at its active site thiol by nitric oxide, peroxynitrite and related nitrosating agents. FEBS Lett. 348, 223–227. Moncada, S., Palmer, R. M. J. and Higgs, E. A. (1991). Nitric oxide: physiology, pathophysiology and pharmacology. Pharmac. Rev. 43, 109–142. Mühl, H. and Dinarello, C. A. (1997). Macrophage inflammatory protein-1 alpha production in lipopolysaccharide-stimulated human adherent blood mononuclear cells is inhibited by the nitric oxide synthase inhibitor NG-monomethyl-L-arginine. J. Immunol. 159, 5063–5069. Mühl, H., Kunz, D. and Pfeilschifter, J. (1994). Expression of nitric oxide synthase in rat glomerular mesangial cells mediated by cyclic AMP. Br. J. Pharmac. 112, 1–8. Mühl, H., Kunz, D., Rob, P. and Pfeilschifter, J. (1993). Cyclosporin derivatives inhibit interleukin 1 induction of nitric oxide synthase in renal mesangial cells. Eur. J. Pharmac. 249, 95–100. Mühl, H. and Pfeilschifter, J. (1995). Amplification of nitric oxide Role of inducible NO synthase in cell signalling synthase expression by nitric oxide in interleukin-1β-stimulated rat mesangial cells. J. Clin. Invest. 95, 1941–1946. Mühl, H., Sandau, K., Brüne, B., Briner, V. A. and Pfeilschifter, J. (1996). Nitric oxide donors induce apoptosis in glomerular mesangial cells, epithelial cells and endothelial cells. Eur. J. Pharmac. 317, 137–149. Nathan, C. and Xie, Q. (1994). Regulation of biosynthesis of nitric oxide. J. Biol. Chem. 269, 13725–13728. Nicolson, A. G., Haites, N. E., McKay, N. G., Wilson, H. M., MacLeod, A. M. and Benjamin, N. (1993). Induction of nitric oxide synthase in human mesangial cells. Biochem. Biophys. Res. Commun. 193, 1269–1274. Nitsch, D. D., Ghilardi, N., Mühl, H., Nitsch, C., Brüne, B. and Pfeilschifter, J. (1997). Apoptosis and expression of iNOS are mutually exclusive in renal mesangial cells. Am. J. Path. 150, 889–900. Park, D. S., Stefanis, L., Yan, C. Y. I., Farinelli, S. E. and Greene, L. A. (1996). Ordering the cell death pathway. Differential effects of Bcl-2, an interleukin-1-converting enzyme family protease inhibitor and other survival agents on JNK activation in serum/nerve growth factor-deprived PC12 cells. J. Biol. Chem. 271, 21898–21905. Peng, H. B., Rajavashisth, T. B., Libby, P. and Liao, J. K. (1995). Nitric oxide inhibits macrophage-colony stimulating factor gene transcription in vascular endothelial cells. J. Biol. Chem. 270, 17050–17055. Pfeilschifter, J., Eberhardt, W., Hummel, R., Kunz, D., Mühl, H., Nitsch, D., Plüss, C. and Walker, G. (1996). Therapeutic strategies for the inhibition of inducible nitric oxide synthase – potential for a novel class of antiinflammatory agents. Cell Biol. Int. 20, 51–58. Pfeilschifter, J. and Huwiler, A. (1996). Nitric oxide stimulates stress-activated protein kinases in glomerular endothelial and mesangial cells. FEBS Lett. 396, 67–70. Pfeilschifter, J. and Schwarzenbach, H. (1990). Interleukin 1 and tumor necrosis factor stimulate cGMP formation in rat renal mesangial cells. FEBS Lett. 273, 185–187. Pilz, R. B., Suhasini, M., Idriss, S., Meinkoth, J. L. and Boss, G. R. (1995). Nitric oxide and cGMP analogs activate transcription from AP-1-responsive promoters in mammalian cells. FASEB J. 9, 552–558. Sandau, K., Pfeilschifter, J. and Brüne, B. (1997). The balance between nitric oxide and superoxide determines apoptotic and necrotic death of rat mesangial cells. J. Immunol. 158, 4938–4946. Sasaki, K., Hattori, T., Fujisawa, T., Takahashi, K., Inoue, H. and Takigawa, M. (1998). Nitric oxide mediates interleukin-1-induced gene expression of matrix metalloproteinases and basic fibroblast growth factor in cultured rabbit articular chondrocytes. J. Biochem. 123, 431–439. Schmidt, H. H. H. W., Lohmann, S. M. and Walter, U. (1993). The nitric oxide and cGMP signal transduction system: regulation and mechanism of action. Biochim. Biophys. Acta 1178, 153–175. 653 Sen, C. K. and Packer, L. (1996). Antioxidant and redox regulation of gene transcription. FASEB J. 10, 709–720. So, H. S., Park, R. K., Kim, M. S., Lee, S. R., Jung, B. H., Chung, S. Y., Jun, C. D. and Chung, H. T. (1998). Nitric oxide inhibits c-Jun N-terminal kinase 2 (JNK2) via S-nitrosylation. Biochem. Biophys. Res. Commun. 247, 809–813. Spiecker, M., Peng, H. B. and Lia, J. K. (1997). Inhibition of endothelial vascular cell adhesion molecule-1 expression by nitric oxide involves the induction and nuclear translocation of IκBα. J. Biol. Chem. 272, 30969–30974. Stamler, J. S. (1994). Redox signaling: nitrosylation and related target interactions of nitric oxide. Cell 78, 931–936. Studer, R. K., DeRupertis, F. R. and Craven, P. A. (1996). Nitric oxide suppresses increases in mesangial cell protein kinase C, transforming growth factor β and fibronectin synthesis induced by thromboxane. J. Am. Soc. Nephrol. 7, 999–1005. Tabuchi, A., Sano, K., Oh, E., Tsuchiya, T. and Tsuda, M. (1994). Modulation of AP-1 activity by nitric oxide (NO) in vitro: NOmediated modulation of AP-1. FEBS Lett. 351, 123–127. Tsurumi, Y., Murohara, T., Krasinski, K., Chen, D., Witzenbichler, B., Kearny, M., Couffinhal, T. and Isner, J. M. (1997). Reciprocal relation between VEGF and NO in the regulation of endothelial integrity. Nature Med. 3, 879–886. VanDervort, A. L., Yan, L., Madara, P. J., Cobb, J. P., Wesley, R. A., Corriveau, C. C., Tropea, M. M. and Danner, R. L. (1994). Nitric oxide regulates endotoxin-induced TNF-α production by human neutrophils. J. Immunol. 152, 4102–4109. Villarete, L. H. and Remick, D. G. (1995). Nitric oxide regulation of IL-8 expression in human endothelial cells. Biochem. Biophys. Res. Commun. 211, 671–676. Wang, H., Li, S. and Pelletier, G. (1998). Role of nitric oxide in the regulation of gonadotropin-releasing hormone and tyrosine hydroxylase gene expression in the male rat brain. Brain Res. 792, 66–71. Xie, Q. W., Whisnant, R. and Nathan, C. (1993). Promoter of the mouse gene encoding calcium-independent nitric oxide synthase confers inducibility by interferon γ and bacterial lipopolysaccharide. J. Exp. Med. 177, 1779–1784. Yamakura, F., Taka, H., Fujimura, T. and Murayama, K. (1998). Inactivation of human manganese-superoxide dismutase by peroxynitrite is caused by exclusive nitration of tyrosine 34 to 3nitrotyrosine. J. Biol. Chem. 273, 14085–14089. Yun, H.-Y., Gonzalez-Zulueta, M., Dawson, V. L. and Dawson, T. M. (1998). Nitric oxide mediates N-methyl-D-aspartate receptorinduced activation of p21ras. Neurobiol. 95, 5773–5778. Zeiher, A. M., Fisslthaler, B., Schray-Utz, B. and Busse, R. (1994). Nitric oxide modulates the expression of monocyte chemoattractant protein 1 in cultured human endothelial cells. Circulation Res. 76, 980–986. Zou, M., Martin, C. and Ullrich, V. (1997). Tyrosine nitration as a mechanism of selective inactivation of prostacyclin synthase by peroxynitrite. Biol. Chem. Hoppe-Seyler 378, 707–713.