* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The molecular mechanisms of general anaesthesia: dissecting the
Survey
Document related concepts
Mechanosensitive channels wikipedia , lookup
Bottromycin wikipedia , lookup
Cell-penetrating peptide wikipedia , lookup
Genetic code wikipedia , lookup
Index of biochemistry articles wikipedia , lookup
Expanded genetic code wikipedia , lookup
Biochemistry wikipedia , lookup
Neurotransmitter wikipedia , lookup
G protein–coupled receptor wikipedia , lookup
NMDA receptor wikipedia , lookup
Signal transduction wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Transcript
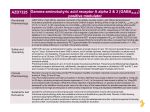
The molecular mechanisms of general anaesthesia: dissecting the GABAA receptor Cameron J Weir BSc(Hons) FRCA PhD The mechanisms underlying the dramatic clinical effects of general anaesthetics remain elusive. This review summarizes the remarkable developments which have occurred in general anaesthetic research over the past decade demonstrating that, rather than acting nonspecifically to disrupt lipid membranes, general anaesthetics target certain CNS proteins in a highly selective manner. Lipid theory of narcosis Paul Ehrlich (1854–1915) first proposed the concept of highly specific interactions between drugs and receptors—corpora non agunt nisi fixata (drugs do not act unless they are bound). However, this concept cannot be easily applied to general anaesthetics because they are chemically and structurally diverse and they lack obvious structure–activity relationships. Such diversity led early researchers to focus on nonspecific perturbation of central nervous system neurones as the basis for the clinical effects of general anaesthetic drugs. For example, at the beginning of the 20th century HH Meyer and CE Overton independently reported a striking correlation between the oil/water partition coefficients of a range of anaesthetic compounds and their ability to immobilize tadpoles, that is, the greater the lipid solubility of the compound the greater its anaesthetic potency. Meyer’s son (KH Meyer) refined these observations in his 1937 publication ‘Contributions to the theory of narcosis’.1 Anomalies with unitary theories The development of sophisticated scientific techniques during the 20th century provided the impetus for numerous theories of anaesthetic action including alterations to the volume or fluidity of lipid bilayers (critical volume hypothesis or lateral phase separation theory) or the disruption of neuronal activity by the formation of anaesthetic microcrystals with water molecules (clathrate theory). These ‘physicochemical’ theories accommodated the diverse chemical nature of general anaesthetic drugs, but closer scrutiny reveals several anomalies: (i) Some compounds do not obey the Meyer and Overton rule. For example, some halogenated alkanes predicted to be potent anaesthetics based on their lipid solubility fail to suppress movement in response to noxious stimulation at appropriate concentrations. These compounds are therefore termed nonimmobilizers. (ii) The ability of general anaesthetics to perturb lipid membranes in vitro can be reproduced by a temperature increase of less than 1 C, a change well within the physiological range and clearly not sufficient to induce loss of consciousness per se. (iii) Stereoisomers existing as mirror images of each other are termed enantiomers (e.g. the isomers of R-(þ)- and S-()etomidate). Enantiomers have identical physicochemical effects in an achiral environment (e.g. the lipid bilayer). However, in vitro and in vivo studies demonstrate that enantiomers of many general anaesthetics do not produce identical clinical effects. For example, the Rþ isomer of etomidate is 10 times more potent than its S isomer at potentiating GABAA receptor activity. These differential effects suggest that the primary site of action of such anaesthetics is not the lipid bilayer and provide compelling evidence for specific interactions with stereoselective binding sites (i.e. within proteins). (iv) According to Meyer and Overton, the addition of methylene groups to a homologous series of long chain alcohols, or alkanes, should increase their lipid solubility and thereby produce a corresponding increase in anaesthetic potency. However, at a certain chain length (n ¼ 10) addition of further methylene groups does not produce the expected doi 10.1093/bjaceaccp/mki068 Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 2 2006 ª The Board of Management and Trustees of the British Journal of Anaesthesia [2006]. All rights reserved. For Permissions, please email: [email protected] Key points Early theories of general anaesthetic action focused on nonspecific disruption of neuronal cell membranes. Compelling evidence now demonstrates that certain general anaesthetics act in a highly specific manner upon central nervous system proteins. Key amino acids within the a subunit of GABAA receptors may contribute to an anaesthetic binding pocket for volatile anaesthetic agents. Genetically engineered mice harbouring single amino acid mutations at critical sites within GABAA receptor subunits lack certain components of i.v. anaesthetic activity in vivo. GABAA receptors containing specific subunits appear to mediate the sedative (b2 subtype) and anaesthetic (b3 subtype) activity of i.v. anaesthetics. Cameron J Weir BSc(Hons) FRCA PhD Consultant Anaesthetist/Senior Lecturer Department of Anaesthesia Ninewells Hospital and Medical School Dundee DD1 9SY Scotland UK E-mail: [email protected] 49 The molecular mechanisms of general anaesthesia increase in anaesthetic potency, i.e. there appears to be a ‘cut off’ effect above a certain molecular volume which is indicative of anaesthetic agents interacting with binding site(s) of finite dimensions. In a landmark series of experiments in the early 1980s, Franks and Lieb2 demonstrated that the relationship reported by Meyer and Overton could be reproduced using a soluble protein. They demonstrated that a range of general anaesthetics acted as competitive antagonists of the protein firefly luciferase. Remarkably, inhibition of luciferase was directly correlated with anaesthetic potency providing persuasive evidence that general anaesthetic drugs could selectively interact with proteins. Of course, the next major hurdle involved identifying which proteins within the mammalian CNS were responsible for mediating the dramatic behavioural effects of general anaesthetic drugs. Transmitter-gated ion channels Chemical synaptic transmission is the process whereby an electrical signal in the presynaptic neurone modulates the release of transmitter into the synaptic cleft to produce a receptor-mediated, electrical, or biochemical event in the postsynaptic neurone. This remarkable feat is achieved by the integrated activity of a range of different proteins including ion channels, enzymes, second messengers, and transporters located in pre- and postsynaptic neurones and within the synaptic cleft. In vitro experiments demonstrate that general anaesthetics alter the activity of many of these proteins, but when clinically relevant concentrations are considered the list of possible targets is greatly diminished. However, one group of proteins has emerged as a likely target for some general anaesthetic agents. This group is known as the transmitter-gated ion channel (TGIC) superfamily and includes g-aminobutyric acid type A (GABAA), strychnine-sensitive glycine, neuronal nicotinic acetylcholine (nAch) and 5-hydroxytryptamine (5-HT3) receptors (Fig. 1). TGICs are usually located within the postsynaptic membrane of excitable neurones and they mediate the majority of fast excitatory and inhibitory neurotransmission within the CNS. Opening of intrinsic ion channels by specific agonists (neurotransmitters) allows selective transfer of ions across the nerve cell membrane. For example, under normal conditions, activation of GABAA receptors induces inward movement of mainly chloride ions down their electrochemical gradient resulting in a hyperpolarization of the cell membrane, whereas activation of nicotinic receptors produces a net inward movement of sodium ions and depolarization of the cell membrane. Therefore, augmenting an inhibitory signal, or inhibiting an excitatory signal, provides a logical mechanism for general anaesthetic action. However, when analysis is restricted to clinically relevant concentrations it appears that inhibitory GABAA receptors are sensitive to modulation by the majority of inhalation and i.v. general anaesthetics agents with ketamine and xenon as the most noticeable exception. GABA-gated receptors The small amino acid GABA is synthesized from glutamate by the action of glutamic acid dehydrogenase (GAD). On release from the presynaptic terminal GABA diffuses across the synaptic cleft to activate GABAA and GABAB receptors. GABAA receptors are classed as ionotropic receptors (linked to an intrinsic ion channel) General Anaesthetics Fig. 1 General anaesthetics modulate the activity of transmitter-gated ion channels to either enhance inhibitory, or inhibit excitatory neurotransmission. At clinically relevant concentrations the majority of general anaesthetics augment the activity of the GABAA receptor. 50 Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 2 2006 The molecular mechanisms of general anaesthesia and are the principal mediators of fast inhibitory neurotransmission in higher centres of the CNS accounting for approximately 30% of all inhibitory synapses. GABAB receptors are classed as metabotropic receptors (coupled to a G-protein), but they are essentially insensitive to therapeutic anaesthetic concentrations and will not be discussed further in this review. Subunit composition and topology GABAA receptors are composed of pentameric arrangements of subunits around a central ion channel pore. Eighteen possible subunits including a1–6, b1–3, g 1–3, d, e, p, r1–3 subtypes have been identified in the mammalian genome. If there were no limitations to receptor assembly, then many thousands of different GABAA receptors could exist within the central nervous system. However, certain molecular rules do regulate the co-assembly of subunits within a receptor and the actual number of GABAA receptor isoforms is probably 30. Furthermore, the differential expression pattern of each subunit can limit certain GABAA receptor combinations to specific brain regions or even neurones. For example, a6-containing GABAA receptors are exclusively found within cerebellar granule cells whereas a5-containing receptors are limited to the hippocampus and sub-thalamic areas. Each subunit is composed of a polypeptide sequence of approximately 450–630 amino acids (40–60 kDa) with large Nterminal and smaller C-terminal extracellular domains (Fig. 2). Hydropathy plots (analysis of primary amino acid sequences predicting regions with high hydrophobic, or hydrophilic nature) suggest that individual subunits contain four distinct transmembrane (TM) domains, with the second transmembrane domain (TM2) lining the channel lumen. A large intracellular loop connects the TM3 and TM4 regions providing sites for phosphorylation by a range of serine, threonine, and tyrosine kinases. Pharmacology of GABAA receptors GABAA receptors are sensitive to a number of clinically useful drugs, including general anaesthetics, benzodiazepines, and other neuro-depressant agents including ethanol.3 Many bind at distinct sites within the receptor to ‘allosterically’ modulate the action of GABA. For example, in the presence of general anaesthetics, the ability of GABA to open, or ‘gate’ the ion channel is increased and, as a result, the overall inhibitory activity of the receptor is enhanced. At supra-clinical concentrations some anaesthetic agents open GABAA receptor ion channels directly without the need for GABA indicating that two or more distinct binding sites (modulatory and direct) might exist for these agents on each receptor. In vitro studies Single amino acids determine i.v. anaesthetic activity If GABAA receptors are important targets for general anaesthetics, are all receptors equally sensitive to their effects, or are certain subunit combinations more sensitive than others? This question can be addressed by examining the activity of the i.v. anaesthetic, etomidate which demonstrates selective effects for receptors containing certain subtypes of the b subunit. For example, receptors containing b2 or b3, but not b1 subunits are particularly sensitive to the modulatory effects of this anaesthetic.4 Studies using a combination of electrophysiological and molecular biological techniques demonstrated that the selectivity of etomidate maps NH2 β γ α α GABA β COOH TM2 Fig. 2 GABAA receptors are composed of pentameric arrangements of subunits arrange around an ion channel pore. The predominant subunit ratio within the cerebral cortex is 2a:2b:g. Each subunit contains approximately 450 amino acid residues putatively forming four transmembrane domains. The second transmembrane domain (TM2) of each subunit faces into the ion channel. The binding of GABA to residues at the interface of a and b subunits induces a conformational change within the TM2 region to open the ion channel pore. Key amino acid residues (represented as closed circle) at the extracellular end of the transmembrane domains of a and b subunits are crucial for volatile and i.v. anaesthetic activity, respectively. Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 2 2006 51 The molecular mechanisms of general anaesthesia to a single amino acid located within the second transmembrane domain (TM2) of the b subunit (asparagine for b2 and b3, and serine for b1 subunits). Exchanging the asparagine for serine within etomidate sensitive b3-containing GABAA receptors reduced the activity of etomidate, whereas the reciprocal change in the b1 subunit, (serine ! asparagine) enhanced the activity of the anaesthetic. Other residues within the neighbouring TM1 and TM3 domains have additionally been shown to influence the actions of propofol, alphaxalone, and pentobarbital. Such dramatic effects produced by altering single amino acids within a large receptor complex provides a persuasive argument for i.v. general anaesthetics interacting in a highly specific manner with GABAA receptors. A binding site for volatile anaesthetics? The effects of volatile agents on GABAA receptor activity are also influenced by a single amino acid. Remarkably, the amino acid responsible (serine) is located within the TM2 region, not in the b subunit, but at the equivalent position in the a subunit. Subsequent studies demonstrated that the volume of this amino acid correlated with the activity of volatile anaesthetics on GABAA receptors. Specifically, substitution with small volume amino acids enhanced the potentiating activity of isoflurane, halothane, and chloroform, whereas the presence of bulkier amino acids reduced anaesthetic activity. Moreover, the volume of neighbouring amino acids within the TM1, TM3, and TM4 regions also influenced inhalation anaesthetic actions.5 The combined approach of altering amino acid volume, together with the use of volatile agents of differing size (isoflurane, 144 Å3; halothane, 110 Å3, and chloroform, 90 Å3) led to the proposal that the four amino acid residues from the extracellular end of TM1, TM2, TM3, and TM4 domains of the a subunit contribute towards an anaesthetic binding pocket for volatile agents of approximately 250–370 Å3. In vivo studies Although in vitro models are invaluable for investigating detailed drug–receptor interactions, interpretation of such experiments is limited because they do not represent a fully integrated nervous system. In order to address this problem, several research groups have created genetically engineered mice harbouring precise mutations within their genotype. Using these mice allows comparison of the pharmacological responses of ‘mutant’ animals with their ‘wild type’ (genetically normal) counterparts and provides a powerful tool for the identification of neuroactive drug targets.6 For example, loss of drug activity after alteration of a specific protein indicates that the altered protein might be involved with mediating the pharmacological effects of the drug. This remarkable technology allows comparison of genetically diverse populations of mice differentiated by only single amino acids within their genome. Such ‘knock-in’ mice have been used successfully to dissect out some receptor isoforms 52 Table 1 Assigning various behavioural features of benzodiazepines to individual GABAA receptor subtypes GABAA receptor subunit Pharmacological effect a1 Sedation Anticonvulsant activity Anterograde amnesia a2 Anxiolysis a3 Myorelaxation a5 Memory and learning Tolerance to benzodiazepines that mediate specific behavioural effects of benzodiazepines and general anaesthetics.6 For example, mice harbouring a single amino acid substitution within the GABAA receptor a1 subunit are resistant to the sedative and anterograde amnesic effects of diazepam, but they retain the anxiolytic response to the benzodiazepine. In contrast, mice harbouring the equivalent mutation within the a2 subunit display reduced anxiolytic behaviour, but retain sensitivity to the sedative and amnesic effects of diazepam. These landmark observations provide compelling evidence for the a1 subunit mediating the sedative and amnesic effects of benzodiazepines, whereas the a2 subunit might mediate anxiolytic activity. Furthermore, it appears that the a5 subunit plays an important role in learning and memory and may also be involved with development of tolerance to benzodiazepines. The various behavioural features of benzodiazepines to individual GABAA receptor subtypes are summarized in Table 1. The role of the b subunit in anaesthesia Similar investigations using ‘knock-in’ mice have been instrumental in assigning the various behavioural facets of general anaesthetic drugs to certain receptor subtypes. The unique subunit selectivity of etomidate guided the development of a strain of genetically engineered mice harbouring a single amino acid mutation within the TM2 region of the b3 subunit.7 These mice were found to be insensitive to some of the effects of etomidate and propofol, that is, the hind limb withdrawal reflex (immobilization) was completely absent and the duration of the loss of righting reflex (hypnosis) was greatly reduced. In contrast, actions of the volatile anaesthetics enflurane and isoflurane were relatively unaffected in the mutant mice. These exciting experiments using whole animals concur with in vitro work showing the actions of certain i.v. anaesthetics to be mediated, in part, by the b3 subunit of the GABAA receptor. Further analysis of etomidate-induced anaesthesia has been carried out using genetically engineered mice harbouring a single amino acid mutation of the GABAA b2 subunit.8 In these knockin mice, the native b2 subunit TM2 asparagine was replaced with a serine residue found within the etomidate insensitive b1 subunit. Intra-peritoneal injection of etomidate, propofol, or pentobarbital produced an anaesthetic effect (loss of righting reflex, loss of pedal withdrawal) indistinguishable from that seen in Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 2 2006 The molecular mechanisms of general anaesthesia genetically normal mice.8 However, the mutant mice were resistant to the sedative and ataxic effects produced by sub-anaesthetic concentrations of etomidate and significantly improved locomotor activity was also observed. In other words, the mutant mice were sensitive to the anaesthetic effects of etomidate presumably because the b3 subunit was still functional, but their recovery profile was consistent with the b2 subunit mediating the ‘hangover’ effects of this i.v. anaesthetic (i.e. drowsiness and ataxia). Anaesthetic targets The chemical diversity of general anaesthetics has resulted in the perception that they are ‘dirty’ drugs. In particular, the volatile agents modulate the activity of many proteins including ion channels and second messenger systems. However, before a protein can be considered a target for general anaesthetic drugs certain criteria must be met; the protein must be sensitive at clinically relevant concentrations; it must be expressed at appropriate anatomical sites within the CNS and, if the anaesthetic displays stereoselective activity, this should be seen both in vitro and in vivo.9 Experimentally, general anaesthetics alter the function of many of these potential targets, but most do not meet the strict conditions set out above. However, certain GABAA receptor subtypes satisfy most of the criteria. It is possible, therefore, that the range of GABAA receptor subunit combinations displaying individual anaesthetic sensitivities together with their distinct expression patterns within the CNS, provides a rationale for the diverse clinical effects of these drugs. Of course, it is unlikely that enhancement of GABAA receptor activity is the only mechanism to account for the wide range of behavioural effects of general anaesthetics. Increasing evidence suggests that modulation of two-pore domain potassium channels, or voltage-gated sodium channels may account for some of the actions of volatile anaesthetic agents. Alternatively, inhibition of glutamate-gated NMDA (N-methyl-D-aspartate) receptors by ketamine, xenon, and nitrous oxide provides a mechanism of action in keeping with a predominant analgesic profile. specific point mutations permits the assignment of certain general anaesthetic and benzodiazepine-induced behaviours to particular GABAA receptor isoforms. Using this information, it may be possible to synthesize novel anaesthetic agents with improved therapeutic profiles, that is, subunit selective compounds producing anaesthesia with a reduced propensity for side-effects (e.g. cardio-respiratory depression, postoperative sedation, ataxia, and nausea and vomiting). Furthermore, relating GABAA receptor isoforms to their expression patterns in the CNS may help with identifying the anatomical locus and the neural networks responsible for general anaesthesia. Acknowledgements The author was supported by a Research Fellowship from the British Journal of Anaesthesia and a research grant from the Royal College of Anaesthetists. Thanks also to Professor J. A. Peters and Dr S. Humble for their help in preparing the manuscript. References 1. Meyer KH. Contributions to the theory of narcosis. Trans Faraday Soc 1937; 33: 1062–8 2. Franks NP, Lieb WR. Do general anaesthetics act by competitive binding to specific receptors? Nature 1984; 310: 599–601 3. Whiting PJ. GABA-A receptor subtypes in the brain: a paradigm for CNS drug discovery? Drug Discov Today 2003; 8: 445–50 4. Belelli D, Pistis M, Peters JA, Lambert JJ. General anaesthetic action at transmitter-gated inhibitory amino acid receptors. Trends Pharmacol Sci 1999; 20: 496–502 5. Jenkins A, Greenblatt EP, Faulkner HJ, et al. Evidence for a common binding cavity for three general anesthetics within the GABAA receptor. J Neurosci 2001; 21: RC136 6. Rudolph U, Mohler H. Analysis of GABAA receptor function and dissection of the pharmacology of benzodiazepines and general anesthetics through mouse genetics. Annu Rev Pharmacol Toxicol 2004; 44: 475–98 7. Jurd R, Arras M, Lambert S, et al. General anesthetic actions in vivo strongly attenuated by a point mutation in the GABAA receptor beta3 subunit. FASEB J 2003; 17: 250–52 8. Reynolds DS, Rosahl TW, Cirone J, et al. Sedation and anesthesia mediated by distinct GABAA receptor isoforms. J Neurosci 2003; 23: 8608–17 Conclusions Dramatic progress has been made since Meyer and Overton first used olive oil and tadpoles to investigate the mechanisms of general anaesthesia. Today, the creation of mice harbouring 9. Krasowski MD, Harrison NL. General anaesthetic actions on ligand-gated ion channels. Cell Mol Life Sci 1999; 55: 1278–1303 Please see multiple choice questions 1–5. Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 2 2006 53