* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download SHORT COMMUNICATION One-step multiplex RT-PCR
Site-specific recombinase technology wikipedia , lookup
Gene expression programming wikipedia , lookup
Gene desert wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Genome (book) wikipedia , lookup
Epigenetics of diabetes Type 2 wikipedia , lookup
Gene nomenclature wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
X-inactivation wikipedia , lookup
Microevolution wikipedia , lookup
Primary transcript wikipedia , lookup
Gene therapy wikipedia , lookup
Designer baby wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
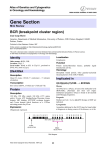
Asia AsPacPacific J. Mol. Journal Biol. Biotechnol., of MolecularVol. Biology 16 (2), and2008 Biotechnology, 2008 Vol. 16 (2) : 41-44 BCR/ABL gene in chronic myeloid leukaemia 41 SHORT COMMUNICATION One-step multiplex RT-PCR for detection of BCR/ABL gene in Malay patients with chronic myeloid leukaemia Rosline Hassan1*, Majdan Ramli1, Wan Zaidah Abdullah1, Rapiaah Mustaffa1, Selamah Ghazali1, Ravindran Ankathil3, Zilfalil Alwi3, Abu Dzar Abdullah2, Abdul Aziz Baba2 Department of Haematology, 2Department of Medicine, 3Human Genome Center, School of Medical Sciences, Health Campus, University Sains Malaysia, Kelantan, Malaysia 1 Received 19 June 2007 / Accepted 22 May 2008 Abstract. BCR/ABL fusion gene is a product derived from translocation of chromosome 22 to chromosome 9. Its presence confers a diagnostic value for chronic myeloid leukaemia (CML). The aim of this study was to detect the presence of BCR/ABL fusion gene using a One-Step Multiplex Reverse Transcriptase –Polymerase Chain Reaction (RT-PCR) and identify the types of breakpoints in Malay patients diagnosed as CML. Their clinical characteristics and cytogenetic findings were also included. Thirty-six Malay patients diagnosed as CML by the usual haematological investigations were enrolled into the study. RNA was extracted from the blood and bone marrow samples and was subjected to One-Step Multiplex RT-PCR for BCR/ABL gene. Thirty-five (97.2%) had BCR/ABL fusion gene. Breakpoints at b3a2 and b2a2 were detected in 68.6% and 31.4% respectively. Majority of them were in chronic phase of CML at diagnosis and the median age was 45.5 years old. In conclusion, One-Step Multiplex RT-PCR has been successfully used to detect and subtype BCR/ABL fusion gene. It is a fast and effective technique. It should be done upfront at diagnosis in patients with CML, as its molecular subtype is crucial in the treatment follow-ups. Keywords. BCR/ABL gene, One–step multiplex, RT-PCR, CML INTRODUCTION The Philadelphia chromosome (Ph) is a shortened of chromosome 22 which is due to a balanced translocation of chromosome 9 and 22. It is the most frequent cytogenetic aberration in human leukaemia. It is detected in more than 95% of patients with Chronic Myeloid Leukaemia (CML), 20% to 40% in patients with Acute Lymphoblastic Leukaemia (ALL) and only 2% to 5% in paediatric ALL (Savage et al., 1997). From clinical and haematological investigations, CML can be divided into chronic, accelerated and blastic phases. In t(9;22)(q34;q11), the BCR gene on chromosome 9 is juxtaposed next to ABL gene located on chromosome 22 giving rise to the BCR/ABL fusion gene. There are two common regions involved in the breakpoints of BCR gene in leukaemia patients. The breakpoints in CML are between exons 12 and 16 (also known as exons b1’-b5) in a region called as major breakpoint cluster region (M-bcr). Most breakpoints fall within the major breakpoint cluster region (M-bcr). Resultant BCR/ABL mRNA molecules with transcript of either b3a2 (55%) or b2a2 (40%) or both b3a2 and b2a2 (5%) encode a 210-kDa fusion proteins. The second breakpoint involves a minor cluster region (m-bcr), which located upstream at e1a2 junction. It is then translated into a 190kDa fusion protein (Okamoto et al., 1997). However a 210-kd protein is the hallmark for CML. Figure 1 illustrates the schematic representation of the ABL and the BCR genes disrupted in the t(9,22)(q34;q11). For many years, RT-PCR has been used routinely to detect the presence of BCR/ABL transcripts. BCR/ABL mRNAs allow for the detection of leukaemic clones. However many routine RT-PCR techniques require multiple steps and many paired primers for the detection of the different breakpoints. This is expensive and time-consuming. To simplify this procedure a One-step multiplex RT-PCR was established in which the cDNA synthesis and PCR were performed in a single tube. This method reduced the number of manipulations and the risk of contamination. It was utilized in Malay patients with CML and enabled the identification of different breakpoints regions/transcripts. *Author for Correspondence. Mailing address: Department of Hematology, School of Medical Sciences, University Sains Malaysia, Kubang Kerian, Kelantan, Malaysia. Fax :+6097652709 ; Email : [email protected] 42 AsPac J. Mol. Biol. Biotechnol., Vol. 16 (2), 2008 BCR/ABL gene in chronic myeloid leukaemia Table 1. Primer sequences used in one step muliplex RT-PCR Primer name Sequences Figure 1. Schematic representation of the ABL and the BCR genes in the t(9;22). Exons are represented by boxes and introns by connecting horizontal lines. Breakpoints in ABL, illustrated as vertical arrows, almost invariably occur either upstream of exon Ib, between Ib and Ia, or between Ia and a2.The BCR gene contains 25 exons, including two putative alternative first (e1’) and second (e2’) exons. The breakpoints in BCR usually occur within one of three breakpoint cluster regions (bcr), the location and probable extents of which are shown by the three double-headed horizontal arrows. In exceptional cases, the BCR breakpoints fall between m-bcr and M-bcr, within the region indicated by the double headed dashed-line arrow. The lower half of the figure shows the structure of the various BCR-ABL mRNA transcripts which are formed in accordance with the position of the breakpoint in BCR. Breaks in m-bcr give origin to BCR/ABL mRNA molecules with an e1a2 junction. The breaks in M-bcr occur either between exons b2 (e13) and b3 (e14) or between b3 and b4 (e15), generating fusion transcripts with a b2a2 or b3a2 junction, respectively. Breakpoints in µ-bcr, the most 3’ cluster region, result in BCR-ABL transcripts with an e19a2 junction. (Adapted from Melo, 1996) BCR-C B2B C5e- CA3- 5’ ACC GCATGTTCCGGGACA AAAG 3’ 5’ ACAGaATTCGCTGACCATCAATAAG 3’ 5’ ATAGGATCCTTTGCAACCGGGTCTGAA 3’ 5‘ TGTTGACTGGCGTGATGTAGTTGCTTGG3’ RNA was added to the master mix with the total volume of 10µl. The BCR/ABL primer mix consisted of primers for mRNAs transcripts for b2a2, b3a2 and e1a2. It was made up of a mixture of four primers. The primer sequences were as listed in Table 1. Then RT-PCR was performed using RT-PCR kit (TitanTM One Tube RT-PCR kit). Each PCR experiment was repeated at least once and included a negative and three positive controls. DNA derived from K562 cell line was used as one of the positive controls. Two other positive controls used were from known ALL and CML patients with breakpoints at e1a2 and b2a2 respectively. PCR parameters were 35 cycles at 96 ºC for 1min, 55 ºC for 50s, and 72 ºC for 1min, followed by 10 min extension at 72 ºC. Amplified products were electrophoresed on a 1.8% agarose gel in 1X TBE buffer. The gel was stained with ethidium bromide placed on a transilluminator and photographed. The two molecular variants yielded products of 310 bp (b2a2) and 385 bp (b3a2) respectively. The e1a2 product was 481 bp while BCR gene was used as internal control with PCR product of 808 bp. MATERIAL AND METHODS RESULTS A total of 36 Malay patients diagnosed as CML in Hospital Universiti Sains Malaysia were enrolled in this study from 2003 to 2006. Written consent was taken from them and hospital ethical committee had approved the study. Blood and bone marrow samples were obtained from patients for cytogenetic and molecular studies. Chromosomal studies were done on bone marrow cells using direct technique or after 24 hour culture in-vitro without stimulation. The chromosomes were identified using a GTG-banding technique and 15-20 metaphases per slide were analysed. RNA was extracted from peripheral blood or bone marrow specimen using standard method as in the manufacturer’s protocol (QIAamp®RNA Blood Mini Kits). The presence of RNA was confirmed by agarose gel electrophoresis. A reaction mix was prepared comprising the following components: 5 x RT buffer, 2 mM dNTP, BCR/ABL primer mix (10um each primers), 25 mM MgCl2, 100 mM DTT, 40 U/ul RNASIN, Rnase-free H2O and Enzyme mix. 100ng of Thirty-six Malay patients diagnosed as CML were identified during the four year study. Thirty patients were in chronic phase, four in accelerated phase while two in blastic phase of CML stages. The median age of the study group was 45.5 years old and comprised of 13 and 23 males and females respectively. Cytogenetic studies were performed on 30 bone marrow samples of which 27 exhibited the Philadelphia chromosome. Three samples had additional chromosome abnormalities such as deletions of chromosome 1, 5 and 13 and all of them were in chronic phase of CML. Cytogenetic results for patients in accelerated and blastic phase were not available in the other 6 CML patients. Our results showed thirty-five (97.2%) were positive for BCR/ABL fusion gene. Of these positive ones, 24 (68.6%) had a breakpoint at b3a2 junction and 11 (31.4%) at b2a2 junction (Figure 2). None of them had fusion transcripts at both junctions. The only one patient who was negative for BCR/ABL has also a normal female karyotype though clinically and morphologically she was diagnosed as CML. AsPac J. Mol. Biol. Biotechnol., Vol. 16 (2), 2008 1 2 3 4 5 6 7 8 9 10 Figure 2. One-step multiplex RT-PCR results for BCR/ABL fusion transcript. Lane 1, 10 : 100bp DNA marker Lane 2,3,4 : 385bp PCR product of b3a2 BCR/ABL transcript Lane 5 : 481bp PCR product of e1a2 BCR/ABL transcript Lane 6 : Negative control Lane 7,8,9 : Positive control for b2a2, b3a2, e1a2 BCR/ABL transcript respectively This patient was persistently in chronic phase for the past 5 years. There was a good correlation between cytogenetic and One-step RT-PCR. DISCUSSION In the year 2002, there were 1447 cases of leukaemias reported to the National Cancer Registry, Malaysia comprising 5.7% of total number of cancers. Male to female ratio was 1.4:1 and leukaemias were the fourth commonest cancer in males and fifth in females. CML constituted 14.6% of total cases of leukaemia (Lim et al., 2002). In this study, 36 Malay patients were diagnosed as CML over a period of four years. These patients were treated either with hydroxyurea or imatinib. The median age was 45.5 years and it tends to occur in younger patients with female to male ratio, 1.7:1. These findings are in contrast to the Scandinavian data, whereby their median age was 67 years and predominantly male with the ratio of 1.4:1 (Chronic Myeloid Leukemia Trialists’ Collaborative Group, 1997). Cytogenetic abnormalities were detected in bone marrow samples of 27 out of 30 patients. Two samples did not yield good metaphase spreads. Philadelphia chromosomes were detected in twenty-five patients and three displayed apparently normal karyotypes. Repeat cytogenetic studies revealed the presence of the Philadelphia chromosome in 2 of those with normal karyotype. The cytogenetic studies were used as the gold standard with which to evaluate the one-step multiplex RT-PCR technique (Harrison et al., 2000). In our study, One-step multiplex RT-PCR technique was performed in all patients diagnosed as CML and BCR/ABL fusion gene was found in all patients except one. One patient BCR/ABL gene in chronic myeloid leukaemia 43 was negative for BCR/ABL fusion gene. One study reported that more than 95% of patients with the diagnosis of CML were positive for BCR/ABL fusion gene (Shepherd et al., 1995). The patient who was negative for BCR/ABL had clinical features and peripheral blood film suggestive of chronic myeloproliferative disease. Her condition was complicated by carcinoma of the breast that developed later. The use of conventional cytogenetic analysis has complemented PCR at initial diagnosis and at follow-up as additional cytogenetic abnormalities, numerical aberrations and abnormalities other than balanced translocations cannot be detected by the later technique. One-step multiplex RT-PCR has its own advantages because it can identify both p190BCR/ABL and p210BCR/ABL in one single procedure. In addition the technique can also discriminate the different breakpoints which can be used as a marker to guide imatinib mesylate treatment. Determination of the type of fusion transcript is crucial for quantitatively monitoring the course of the disease during treatment. Nested RT-PCR is another method routinely performed for the detection of BCR/ABL gene (Gleissner et al., 2001). The benefit of the multiplex approach is to simplify and shorten the procedure of RT-PCR for the detection of p210 and p190 in a single reaction. Secondly the amount of RNA used is minimised. Multiplex PCR assay is clinically useful, efficient and a fast procedure for the detection of fusion gene products, saving time and cost. This technique is useful for initial diagnosis to guide CML in clinical management. ACKNOWLEDGEMENT We would like to thank Mr David Mc Donald from Molecular Diagnostic Lab, Institute of Clinical Pathology and Medical Research, Westmead Hospital, Australia for providing us with the K562 cDNA. The work is supported by the USM short term-grant ((304/PPSP/6131215). This study was approved by ethical committee, School of Medical Sciences, University Sains Malaysia, Malaysia. REFERENCES Chronic Myeloid Leukemia Trialists' Collaborative Group.1997. Interferon alfa versus chemotherapy for chronic myeloid leukemia: a meta-analysis of seven randomized trials. Journal of the National Cancer Institute, 89, 1616–1620. Gleissner, B., Rieder, H., Thiel, E., Fonatsch, C., Janssen, L.A., Heinze, B., Janssen, J.W., Schoch, C., Goekbuget, N., Maurer, J., Hoelzer, D. and Bartram, C.R. 2001. 44 AsPac J. Mol. Biol. Biotechnol., Vol. 16 (2), 2008 Prospective BCR-ABL analysis by polymerase chain reaction (RT-PCR) in adult acute B-lineage lymphoblastic leukemia: reliability of RT-nested-PCR and comparison to cytogenetic data. Leukemia 15:1834-40. Harrison, C.J. 2000. The management of patients with leukaemia: The role of cytogenetics in this molecular era. British Journal of Haematology 108(1):19-30. Lim, G.C., Halimah, Y. and Lim, T.O. 2002. In Cancer incidence in Malaysia, The First Report of The National Cancer Registry: Ministry of Health. Melo, J.V. 1996. The diversity of BCR-ABL fusion proteins and their relationship to leukaemia phenotype. Blood 88: 2375-2384 (editorial). Okamoto, K., Krawasa, M., Sakai, H., Ogura, H., Morita, K. aand Naruse, T., 1997. �������������������������������� A novel acute lymphoid leukemia type BCR/ABL transcript in chronic myelogenous leukemia. British Journal of Haematology 96: 611-613. Savage, D.G., Szydlo, RM. and Goldman, J.M. 1996. Clinical features at diagnosis in 430 patients with chronic myeloid leukaemia seen at a referral centre over a 16-year period. British Journal of Haematology 96:111-116. Shepherd, P., Suffolk, R., Halsey, J. and Allan, N. 1995. Analysis of molecular breakpoint and m-RNA transcripts in a prospective randomized trial of interferon in chronic myeloid leukaemia: no correlation with clinical features, cytogenetic response, duration of chronic phase or survival. British Journal of Haematology 89: 546-554. BCR/ABL gene in chronic myeloid leukaemia