* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download rpoB gene sequence-based characterization of emerging non
Gene desert wikipedia , lookup
History of genetic engineering wikipedia , lookup
Gene therapy wikipedia , lookup
Point mutation wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Gene nomenclature wikipedia , lookup
Genome evolution wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Genome editing wikipedia , lookup
Pathogenomics wikipedia , lookup
Koinophilia wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
DNA barcoding wikipedia , lookup
Designer baby wikipedia , lookup
Metagenomics wikipedia , lookup
Helitron (biology) wikipedia , lookup
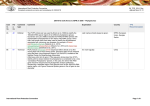
International Journal of Systematic and Evolutionary Microbiology (2006), 56, 133–143 DOI 10.1099/ijs.0.63969-0 rpoB gene sequence-based characterization of emerging non-tuberculous mycobacteria with descriptions of Mycobacterium bolletii sp. nov., Mycobacterium phocaicum sp. nov. and Mycobacterium aubagnense sp. nov. Toı̈di Adékambi, Pierre Berger, Didier Raoult and Michel Drancourt Correspondence Michel Drancourt Michel.Drancourt@medecine. Unité des Rickettsies, CNRS UMR 6020 IFR 48, Faculté de Médecine, 27, Boulevard Jean Moulin, Université de la Méditerranée and Assistance Publique-Hôpitaux de Marseille Timone, Fédération de Microbiologie Clinique, Marseille, France univ-mrs.fr Over the past 10 years, 16S rRNA gene sequencing has contributed to the establishment of more than 45 novel species of non-tuberculous mycobacteria and to the description of emerging mycobacterial infections. Cumulative experience has indicated that this molecular tool underestimates the diversity of this group and does not distinguish between all recognized mycobacterial taxa. In order to improve the recognition of emerging rapidly growing mycobacteria (RGM), rpoB gene sequencing has been developed. Our previous studies have shown that an RGM isolate is a member of a novel species if it exhibits >3 % sequence divergence in the rpoB gene from the type strains of established species. When applied to a collection of 59 clinical RGM isolates, rpoB gene sequencing revealed nine novel isolates (15?3 %) whereas only two isolates (3?4 %) were deemed to be novel by conventional 16S rRNA gene sequence analysis. A polyphasic approach, including biochemical tests, antimicrobial susceptibility analyses, hsp65, sodA and recA gene sequence analysis, DNA G+C content determination and cell-wall fatty acid composition analysis, supported the evidence that these nine isolates represent three novel species. Whereas Mycobacterium phocaicum sp. nov. (type strain N4T=CIP 108542T=CCUG 50185T) and Mycobacterium aubagnense sp. nov. (type strain U8T=CIP 108543T=CCUG 50186T; Mycobacterium mucogenicum group) were susceptible to most antibiotics, Mycobacterium bolletii sp. nov. (type strain BDT=CIP 108541T=CCUG 50184T; Mycobacterium chelonae–abscessus group) was resistant to the quinolones, tetracycline, macrolides and imipenem. Only M. bolletii was resistant to clarithromycin. These data illustrate that rpoB gene sequence-based identification is a powerful tool to characterize emerging RGM and mycobacterial infections and provides valuable help in differentiating RGM at both the intra- and interspecies level, thus contributing to a faster and more efficient diagnosis and epidemiological follow-up. INTRODUCTION Over the last 10 years, 16S rRNA gene sequence analysis of non-tuberculous mycobacteria (NTM) has led to the description of 45 novel species and has contributed to the Abbreviations: MIC, minimum inhibitory concentrations; NTM, nontuberculous mycobacteria; RGM, rapidly growing mycobacteria. The GenBank/EMBL/DDBJ accession numbers for the 16S rRNA, recA, hsp65 and sodA genes of Mycobacterium bolletii BDT, Mycobacterium phocaicum N4T and Mycobacterium aubagnense U8T are AY859681–AY859683, AY859687–AY859689, AY859675– AY859677 and AY862403 and AY859706–AY859707, respectively. A table detailing whole-cell fatty acid content and a figure showing the hypervariable region of the rpoB gene are available as supplementary material in IJSEM Online. 63969 G 2006 IUMS description of novel clinical isolates. Infections caused by rapidly growing mycobacteria (RGM) have received greater clinical attention in recent years because of their increasing incidence in AIDS patients (Smith et al., 2001; Wallace et al., 1993, 1997) as well as in non-immunocompromised patients (Brown-Elliott & Wallace, 2002). Many RGM are ubiquitous in the environment and water has been shown to be an important source of these opportunistic mycobacteria (Covert et al., 1999; Dailloux et al., 1999; Wallace et al., 1998). This fact is illustrated by reports of cases such as Mycobacterium fortuitum furunculosis following footbaths (Winthrop et al., 2002), a disseminated infection in a leukaemia patient (Kauppinen et al., 1999) and hypersensitivity pneumonitis in automobile workers exposed to metalworking fluids (Wallace et al., 2002; Wilson et al., 2001). Likewise, Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 Printed in Great Britain 133 T. Adékambi and others contamination of hospital equipment and medication, traced to the ubiquitous presence of these organisms in tap water and their resistance to commonly used disinfectants (Tiwari et al., 2003; Wallace et al., 1998), was responsible for pseudo-outbreaks of infections associated with surgical implants, health care-associated septicaemia and lung disease following bronchoscopy (Anaissie et al., 2002; Ashford et al., 1997; Ferguson et al., 2004; Lai et al., 1998; Wallace et al., 1998). The most common types of infection are skin and soft tissue infections, infections characterized by slowly progressive granulomatous inflammation, lymphadenitis and skeletal, catheter-related, disseminated and pulmonary infections (Brown-Elliott & Wallace, 2002; Schinsky et al., 2004). Increasing recovery of RGM from environmental and clinical sources has prompted the development of laboratory methods to determine their taxonomic affiliation and identify them precisely. Accurate identification of RGM species is a key step towards the description of the emerging opportunistic infections that they cause. Conventional laboratory methods alone are unable to discriminate between RGM because of their overlapping phenotypic patterns (Conville & Witebsky, 1998; Springer et al., 1996). Cell-wall fatty acid and mycolic acid composition analysis contributed to the identification of novel mycobacterial species (Butler & Kilburn, 1990; Munoz et al., 1997), but the discriminatory power of the analyses was limited by profile similarity among emerging RGM (Wilson et al., 2001). 16S rRNA gene sequencing has been used as the first-line method for the identification of unusual mycobacterial isolates (Pauls et al., 2003; Tortoli et al., 2001) and for further discrimination of emerging NTM (Böddinghaus et al., 1990; Rogall et al., 1990). It has contributed greatly to the delineation of novel species of the genus Mycobacterium and to the description of new clinical forms due to known NTM. However, 16S rRNA gene sequence-based description of novel mycobacterial taxa is still a matter of debate. Ambiguous results can be obtained due to the possible presence of two copies of the 16S rRNA gene with different sequences in the same organism (Adékambi & Drancourt, 2004; Ninet et al., 1996; Reischl et al., 1998; Turenne et al., 2001). Closely related RGM species, such as Mycobacterium houstonense and Mycobacterium senegalense, cannot be discriminated by this molecular tool (Adékambi et al., 2003; Adékambi & Drancourt, 2004). Partial sequencing of PCR-amplified rpoB, the gene encoding the b-subunit of bacterial RNA polymerase, has been developed as a suitable tool for the accurate identification of RGM (Adékambi et al., 2003) and its usefulness for determining the taxonomy of this group of micro-organisms has been demonstrated (Adékambi & Drancourt, 2004). In this study, this new tool was applied to a collection of clinical RGM isolates and 9/59 isolates from 52 patients were found to exhibit three original rpoB sequences, indicative of novel RGM species. A polyphasic investigation, including biochemical tests, antimicrobial susceptibility analyses, DNA G+C content determination, cell-wall fatty acid composition analyses and sequence-based analyses, confirmed that these isolates were indeed prototype strains for emerging RGM of clinical interest. The names Mycobacterium bolletii sp. nov., Mycobacterium phocaicum sp. nov. and Mycobacterium aubagnense sp. nov. are proposed for these three novel RGM. METHODS Mycobacterial strains, genetic and phylogenetic analyses. The nine isolates under study and their clinical sources are listed in Table 1. In addition, we determined sequences for two RGM species: ‘Mycobacterium massiliense’ CIP 108297 and Mycobacterium alvei CIP 103464T. These newly determined sequences were added to those of 20 species studied previously (Adékambi et al., 2003). DNA was extracted from colonies grown on 5 % sheep blood agar using the Fast-prep device and the FastDNA kit according to the manufacturer’s recommendations (BIO 101). Five molecular targets including the 16S rRNA (Weisburg et al., 1991), hsp65 (Telenti et al., 1993), Table 1. Laboratory and clinical information for the three novel RGM Strain M. bolletii BDT (=CIP 108541T=CCUG 50184T) E2 U2 U6 M. phocaicum N4T (=CIP 108542T=CCUG 50185T) N9 N30 M. aubagnense U8T (=CIP 108543T=CCUG 50186T) D5 134 Clinical source GenBank accession number DNA G+C content (mol%) 16S rRNA recA hsp65 sodA Sputum Stomach aspirate Sputum Sputum AY859681 AY859687 AY859675 AY862403 63±2 Bronchial aspirate Sputum Bronchial aspirate AY859682 AY859688 AY859676 AY859706 65±1 Bronchial aspirate Joint fluid AY859683 AY859689 AY859677 AY859707 65±1 Downloaded from www.microbiologyresearch.org by International Journal of Systematic and Evolutionary Microbiology 56 IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 Three novel rpoB-defined Mycobacterium species sodA (Adékambi & Drancourt, 2004), recA (Blackwood et al., 2000) and rpoB (Adékambi et al., 2003) genes were amplified and sequenced. A partial rpoB sequence of 764 bp was amplified using the primer pair Myco-F (59-GGCAAGGTCACCCCGAAGGG-39) and Myco-R (59-AGCGGCTGCTGGGTGATCATC-39) (see Supplementary Fig. S1 in IJSEM Online) and a 723 bp sequence (apart from 41 nt at both ends of the amplicon, corresponding to primer binding sites) was derived from the amplicon by using the same primer pair in both directions (Adékambi et al., 2003). Products of sequencing reactions were recorded with an ABI Prism 3100 DNA sequencer following the manufacturer’s standard protocol (Perkin Elmer Applied Biosystems). The percentage similarity between the sequences was determined using the CLUSTAL W program supported by the PBIL website (http://npsa-pbil.ibcp.fr/cgi-bin/npsa). For phylogenetic analyses, sequences were trimmed so that they started and finished at the same nucleotide position for all isolates. Multisequence alignment was performed by using the CLUSTAL_X program, version 1.81 from the PHYLIP software package (Thompson et al., 1997). A phylogenetic tree was obtained from DNA sequences by using the neighbour-joining method with Kimura’s two-parameter (K2P) distance correction model with 1000 bootstrap replications in the MEGA version 2.1 software package (Kumar et al., 2001). The tree was rooted using Mycobacterium tuberculosis and Mycobacterium leprae. The sequences determined in this study have been deposited in GenBank/EMBL/DDBJ (Table 1 and Fig. 1). DNA G+C content determination and cellular fatty acid analysis. After culture on 5 % sheep blood agar for 3 days, DNA extrac- tion, purification, degradation and determination of the DNA G+C content by HPLC were performed as described by Mesbah et al. (1989) except that a Waters 625 LC system with a Waters 486 Tenable Absorbance Detector and a Waters 746 Data Module (Millipore) were used. Three determinations were performed. Total fatty acid methyl esters were extracted and prepared by following the instructions for the Microbial Identification System (Microbial ID) and were analysed by GLC using a gas chromatograph (HP 6890A; Hewlett Packard). Identification of fatty acids for isolates BDT, N4T and U8T was performed using the Microbial Identification System with a library created using Sherlock Library Generation System version 4.0 software (Sasser, 1990). Phenotypic characterization of the isolates. Sputum and bronchioalveolar specimens were decontaminated as previously described (Kent & Kubica, 1985; Kubica et al., 1963). Half of the sediment was frozen whilst the other half was inoculated into BACTEC 9000MB broth according to the manufacturer’s instructions (BD Biosciences) after Ziehl–Neelsen staining. The joint fluid specimen was inoculated directly into BACTEC 9000MB broth. Mycobacteria were subcultured on Middlebrook 7H10 agar, eggbased Lowenstein–Jensen (LJ) slants (bioMérieux) and 5 % sheep blood agar (bioMérieux) and cultures were inspected twice weekly Fig. 1. Phylogenetic tree of the partial rpoB gene sequences of the three novel mycobacterial species and 21 RGM prepared by using the neighbour-joining method and Kimura’s two-parameter distance correction model. The support of each branch, as determined from 1000 bootstrap samples, is indicated by the value at each node (as a percentage). M. tuberculosis and M. leprae were used as the outgroups. Bar, 2 % difference in nucleotide sequences. http://ijs.sgmjournals.org Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 135 T. Adékambi and others for the presence of colonies. We observed colony morphology, pigmentation and the ability of the isolate to grow at various temperatures (24, 30, 37 and 42 uC) on 5 % sheep blood agar, LJ slants, Middlebrook 7H10 agar and LJ slants in the presence of 5 % NaCl. We tested the activities of arylsulfatase and catalase, iron uptake and degradation of p-aminosalicylic acid (Kent & Kubica, 1985; Vincent et al., 2003). Additional biochemical tests were performed by inoculation of API Coryne and API 20E strips (bioMérieux) (Adékambi et al., 2004) according to the manufacturer’s instructions with an incubation time of 3 days at 30 uC under a highly humidified atmosphere. Antibiotic susceptibility testing. Mycobacterial suspensions of the isolates were prepared by emulsifying colonies grown on 5 % sheep blood agar slants into 5 ml sterile water to achieve a density equal to a 1?0 McFarland turbidity standard by visual examination. Suspensions were mixed vigorously on a vortex mixer for 20 s and then inoculated on the entire surface of a 5 % sheep blood agar plate. The minimum inhibitory concentrations (MIC) of rifampicin, ciprofloxacin, ofloxacin, sparfloxacin, doxycycline, minocycline, erythromycin, clarithromycin, azithromycin, amikacin, penicillin, amoxycillin, imipenem, cefotaxime, ceftriaxone, metronidazole, teicoplanin and vancomycin were determined by incubation with the respective E-test (AB Biodisk) at 30 uC for 3 days. An additional disk-diffusion method on 5 % sheep blood agar for 3 days at 30 uC was used to determine the susceptibility to trimethoprim/sulfamethoxazole (1?25/23?75 mg), tobramycin (10 mg), amoxycillin/clavulanate (30 mg), pipemidic acid (30 mg), cefalotin (30 mg) and cefoxitin (30 mg). The MIC of the antimicrobial agents tested was determined according to the breakpoints recommended by the NCCLS (NCCLS 2002, 2003) and those proposed by Brown-Elliott & Wallace (2002). Every test was done three times on three separate days in order to ensure the reproducibility of results. RESULTS Mycobacterial strains Of the nine isolates studied, three isolates (N4T, N30 and U8T) were recovered from bronchial aspirate specimens, four isolates (BDT, U2, U6 and N9) from sputum specimens, one isolate (E2) from a stomach aspirate and one isolate (D5) from joint fluid. Genetic and phylogenetic analyses We showed previously that RGM isolates belong to the same species if they have <2 % partial rpoB gene sequence divergence from an established species. Isolates can be considered to belong to a novel species if they exhibit >3 % rpoB sequence divergence from established species using the partial 723 bp rpoB sequence (Adékambi et al., 2003, 2004). When applying rpoB gene sequencing and the above criteria to the first-line identification of 59 RGM clinical isolates collected from 52 patients over a 7 year period, we found that nine isolates (15?3 %) were not well established at the species level. Four isolates, BDT, E2, U2 and U6, shared only 95?0 % sequence similarity with Mycobacterium abscessus ATCC 19977T, three isolates, N4T, N9 and N30, shared 95?5 % sequence similarity with Mycobacterium mucogenicum ATCC 49650T, and two isolates, U8Tand D5, shared 90?1 % sequence similarity with M. mucogenicum ATCC 49650T due to 15 bp insertions corresponding to the amino 136 acids ANGAY inserted at position 141 (M. mucogenicum ATCC 49650T partial rpoB gene amino-acid sequence numbering). rpoB gene sequence variation was not observed among isolates belonging to the same species. An rpoB phylogenetic tree was created that included a representative sequence for each of the nine isolates and 21 sequences from established RGM species tested in our laboratory (Fig. 1). These analyses suggested that strain BDT was recently derived from M. abscessus and belongs to the Mycobacterium chelonae–M. abscessus group. Strain N4T and U8T were closely related to M. mucogenicum and belonged to the M. mucogenicum group. A bootstrap value ¢75 % in the neighbour-joining tree supported the fork separating strain BDT, strain N4T and strain U8T from the closely related species. Their lineages were clearly different from that of closely related species and quite distant from other recognized RGM. Further sequence analyses of the 16S rRNA gene sequences over 1483 bp showed that isolates BDT, E2, U2 and U6 shared 100 % sequence similarity with M. abscessus ATCC 19977T, isolates N4T, N9 and N30 shared 100 % sequence similarity with M. mucogenicum ATCC 49650T and isolates U8T and D5 shared 99?1 % sequence similarity with M. mucogenicum ATCC 49650T (14 bp difference). Further molecular characterization of the seven isolates for which the 16S rRNA sequence exhibited 100 % similarity with the corresponding type strain, but showed large differences in the rpoB gene sequence, was done by analysis of the hsp65, sodA and recA gene sequences. For the hsp65, sodA and recA genes, strain BDT shared 98?2, 97?7 and 97?9 % similarity, respectively, with M. abscessus. Strain N4T showed 98?8 % similarity with M. mucogenicum ATCC 49650T in the hsp65 gene sequence, 98?3 % for the sodA gene and 98?4 % for the recA gene. Thus, the isolates initially identified as M. abscessus or as M. mucogenicum ATCC 49650T on the basis of their phenotypic pattern and 16S rRNA gene sequencing were unambiguously distinguished from closely related species by rpoB, recA, sodA and hsp65 gene sequencing. The one remaining novel strain, U8T, shared 96?0 % similarity with M. mucogenicum ATCC 49650T in the hsp65 gene sequence, 96?6 % in the sodA gene and 94?8 % in the recA gene. Complete rpoB gene sequence analyses of the three novel species revealed similar relationships to the partial rpoB sequence analysis described previously (Adékambi et al., 2003). Molecular analysis, including sequence analyses of the 16S rRNA, hsp65, sodA, recA and rpoB genes, identified the nine isolates as representatives of three novel mycobacterial species. No gene sequence variation was observed among isolates belonging to the same species. DNA G+C content and fatty acid analysis The DNA G+C content was 63–65 mol% and the results are summarized in Table 1. GLC analyses of the fatty acids of isolates revealed the expected pattern diagnostic for members of the genus Mycobacterium. The profiles of strains BDT, N4T and U8T contained straight-chain saturated and unsaturated fatty acids including 16 : 0 (35?2, 15?7 and Downloaded from www.microbiologyresearch.org by International Journal of Systematic and Evolutionary Microbiology 56 IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 Three novel rpoB-defined Mycobacterium species 19?7 %, respectively), 18 : 1v9c (32?1, 23?9 and 20?4 %), 16 : 1v7c/15 : 0 iso (9?7, 10?7 and 9?8 %), 16 : 1v7c (3?8, 6?1 and 10?6 %), 14 : 0 (6?1, 4?9 and 6?5 %), 17 : 1v7c (0, 20?3 and 13?9 %), 18 : 2v6,9c/18 : 0 ante (6?9, 4?3 and 3?3 %). Minor amounts of other fatty acids were also detected. Tuberculostearic acid (TBSA; 10-methyl 18 : 0) was only detected in isolate BDT (2?3 %). Details of the fatty acid content are presented in Supplementary Table S1 in IJSEM Online. Based on the pattern of fatty acids disclosed by GLC analysis and using the MIDI fatty acid database, the similarity of strain BDT and M. abscessus CIP 104536T was 93?3 %, strain N4T and M. mucogenicum ATCC 49650T showed 90?9 % similarity and strain U8T and M. mucogenicum ATCC 49650T showed 93?7 % similarity. These results suggest that the three strains were different from closely related species. Phenotypic characteristics and susceptibility testing Biochemical and susceptibility characteristics that differentiated the clinical isolates from closely related species are summarized in Tables 2 and 3. Colonies of strains BDT, N4T and U8T are non-pigmented and appear on 5 % sheep blood agar, Middlebrook 7H10 agar and egg-based LJ slants in 2–5 days at temperatures between 24 and 37 uC. No growth occurs at 42 uC. In the M. mucogenicum group, strain N4T utilizes citrate as the sole carbon source, unlike strain U8T and M. mucogenicum ATCC 49650T. All three strains tested Table 2. Differentiating biochemical characteristics of the three novel RGM and closely related Mycobacterium species Strains: 1, M. bolletii BDT; 2, M. abscessus CIP 104536T; 3, M. phocaicum N4T; 4, M. mucogenicum ATCC 49649; 5, M. mucogenicum ATCC 49650T; 6, M. aubagnense U8T. All species were able to grow at 24, 30 and 37 uC, but not at 42 uC. All strains are nonpigmented and test negative for the following enzyme activities: b-galactosidase, N-acetyl-b-glucosaminidase, urease, gelatinase, arginine dihydrolase, lysine decarboxylase, ornithine decarboxylase and tryptophan desaminase. All species are positive for catalase and arylsulfatase (3 days) activity, are able to hydrolyse aesculin and can degrade p-aminosalicylate. Production of H2S and indole and iron uptake are negative. All strains are able to produce acetoin. +, Positive; 2, negative; ±, intermediate. Characteristic 1 2 3 4 5 6 Enzyme activity: Alkaline phosphatase a-Glucosidase b-Glucuronidase Nitrate reductase Pyrazinamidase Pyrrolidonyl arylamidase Citrate utilization Tolerance of 5 % NaCl + 2 2 2 + + 2 + + + + 2 + + 2 + + 2 2 + + 2 + 2 2 2 2 + + 2 + 2 2 2 2 + + 2 2 2 + 2 2 2 2 ± 2 2 http://ijs.sgmjournals.org positive for acetoin and aesculin activity and were negative for urease activity. Strain N4T and M. mucogenicum ATCC 49650T exhibited positive activities for nitrate reductase and pyrazinamidase, unlike strain U8T. Strains N4T and U8T showed positive alkaline phosphatase activity, in contrast with M. mucogenicum ATCC 49650T. Using the API Coryne strip, none of the strains tested produced acid from Dglucose, D-ribose, D-xylose, D-mannitol, D-maltose, Dlactose, D-sucrose or glycogen in 3 days. Using the API 20E strip, none of the strains utilized D-glucose, D-mannitol, inositol, D-sorbitol, L-rhamnose, D-sucrose, D-melibiose, amygdalin or L-arabinose as sole carbon sources in 3 days. Strain N4T, U8T and M. mucogenicum ATCC 49650T were susceptible to imipenem, minocycline, doxycycline, clarithromycin, erythromycin, azithromycin, amikacin, ciprofloxacin, ofloxacin and sparfloxacin. Strain N4T was resistant to amoxycillin, amoxycillin/clavulanate and trimethoprim/sulfamethoxazole, in contrast to M. mucogenicum ATCC 49650T. Strain U8T was susceptible to tobramycin, unlike M. mucogenicum ATCC 49650T. Strain BDT and M. abscessus have intermediate resistance to amikacin, but strain BDT was resistant to clarithromycin, whereas M. abscessus was susceptible. The antimicrobial susceptibility profiles and the biochemical test patterns obtained for strains BDT, N4T and U8T and the corresponding isolates were identical. DISCUSSION 16S rRNA gene sequencing has been used as the reference method for identifying unusual mycobacterial isolates (Pauls et al., 2003; Tortoli et al., 2001; Turenne et al., 2001). This approach has contributed to the description of 45 novel NTM species over the last 10 years. However, the investigation of large NTM collections by 16S rRNA gene sequencing has not resolved the classification of all isolates. The use of 16S rRNA gene sequencing for the identification of clinical NTM has indicated that 37 % of such isolates remain unclassified and suggests the need for complementary molecular tools for proper phylogenetic assignment and accurate NTM identification (Pauls et al., 2003). The common assumption that bacterial isolates are members of the same species if they have fewer than 5–15 bp differences in the 16S rRNA gene sequence (Fox et al., 1992) or if they have 16S rRNA gene sequence similarity >97 % (Drancourt et al., 2000) may not be applicable to mycobacteria, whose members are much more closely related to each other (Adékambi & Drancourt, 2004; Tortoli, 2003; Turenne et al., 2001). Furthermore, 16S rRNA gene sequence-based descriptions of novel mycobacterial taxa are still a matter of debate because ambiguous results have been found due to the presence of two copies of the 16S rRNA gene with different sequences in the same organism (Adékambi & Drancourt, 2004; Ninet et al., 1996; Reischl et al., 1998; Turenne et al., 2001). Molecular tools including sodA (Zolg & Philippi-Schulz, 1994), dnaJ (Takewaki et al., 1994), 32kDa protein-encoding gene (Soini & Viljanen, 1997), hsp65 (Ringuet et al., 1999) recA (Blackwood et al., 2000), 16S-23S Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 137 T. Adékambi and others Table 3. Antimicrobial Mycobacterium species susceptibility of the three novel RGM and closely related Strains: 1, M. bolletii BDT; 2. M. abscessus CIP 104536T; 3, M. phocaicum N4T; 4, M. mucogenicum ATCC 49649; 5, M. mucogenicum ATCC 49650T; 6, M. aubagnense U8T. Values are MIC (mg ml21). AMC, Amoxycillin/clavulanate; TMP/SMZ, trimethoprim/sulfamethoxazole. +, Positive. AMC (disc 20/10 mg) Amikacin Amoxycillin Azithromycin Cefalotin (disc 30 mg) Cefinase test Cefotaxime Cefoxitin (disc 30 mg) Ceftriaxone Ciprofloxacin Clarithromycin Colistin (disc 50 mg) Doxycycline Erythromycin Imipenem Metronidazole Minocycline Ofloxacin Penicillin Pipemidic acid (disc 20 mg) Rifampicin Sparfloxacin Teicoplanin TMP/SMZ (disc 1?25/23?75 mg) Tobramycin (disc 10 mg) Vancomycin 1 2 3 4 5 6 >4 24 >256 >256 >32 + >256 >32 >256 >32 >256 >2 >32 >256 >32 >256 >256 >32 >32 >16 >32 >32 >256 >8 >8 >256 >4 32 >256 >256 >32 + >256 >32 >256 >32 1?5 >2 >32 >256 >32 >256 >256 >32 >32 >16 >32 >32 >256 >8 >8 >256 >4 1?5 64 1?5 >32 + 32 <2 >256 0?50 0?064 >2 1?5 3 0?50 >256 0?75 0?75 >32 >16 >32 0?25 >256 >8 >8 >256 <4 4 3 1?5 >32 + 48 <8 >256 0?25 0?125 >2 0?125 1?5 0?75 >256 0?50 3 >32 >16 >32 0?50 128 <2 >8 >256 <4 1 1?5 0?125 >32 + 12 <8 >256 0?125 0?032 >2 1?5 1 0?75 >256 1?5 0?75 >32 >16 >32 0?25 >256 <2 >8 >256 <4 3 0?125 2 >32 + 64 <8 >256 0?125 0?125 >2 1 1 0?75 >256 1?5 0?25 >32 >16 >32 0?125 64 <2 <4 >256 rRNA internal transcribed spacer (ITS) (Park et al., 2000), DNA gyrase genes (Dauendorffer et al., 2003) and secA1 (Zelazny et al., 2005) sequence analyses have been proposed as alternative tools for the molecular identification of NTM isolates, including RGM. However, no criteria have been validated for the delineation of species using these molecular tools. The rpoB gene is a single-copy gene encoding the b-subunit of bacterial RNA polymerase and has been previously used for the molecular identification of numerous bacterial genera, including Mycobacterium (Adékambi et al., 2003; Kim et al., 1999; Lee et al., 2003). In this study, when rpoB gene sequencing was applied to improve the genetic identification of clinical RGM isolates, we obtained 9/59 clinical isolates (15?3 %) that exhibited >3 % rpoB gene sequence divergence from the closest related species. However, 7/9 isolates (77?8 %) shared 100 % similarity with the corresponding 16S rRNA gene sequence. Similarly, Blackwood et al. (2000) found that Mycobacterium peregrinum ATCC 14467T and M. peregrinum ATCC 23015, which have complete 16S rRNA gene sequence identity, diverged by 3?9 % in the 915 bp recA gene sequence; the intraspecies variation of mycobacteria was <1?3 %. 138 Sequencing of the rpoB gene alone revealed that 15?3 % of isolates were deemed to be novel, corresponding to three novel species, whereas conventional 16S rRNA gene sequencing identified only 3?4 % of the isolates as novel, corresponding to one novel species. The intraspecies similarity of the 915 bp recA gene ranges from 98?7 to 100 % (Blackwood et al., 2000). This additional finding allowed us to consider the sequences which were deemed to be novel as representing genuine novel species. Further molecular analysis, including hsp65 and sodA gene sequence analyses, confirmed that the nine isolates represented Mycobacterium species that were distinct from known Mycobacterium species. These data illustrate that rpoB gene sequencing is a powerful tool for the characterization of novel RGM species, as previously illustrated by the use of the rpoB gene sequence for the delineation of ‘M. massiliense’ (Adékambi et al., 2004) and Mycobacterium cosmeticum (Cooksey et al., 2004). Previous studies have shown that the antibiotic susceptibility of RGM varies widely (Brown et al., 1992; Swenson et al., 1985; Wallace et al., 1990, 1991; Woods et al., 2000). Downloaded from www.microbiologyresearch.org by International Journal of Systematic and Evolutionary Microbiology 56 IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 Three novel rpoB-defined Mycobacterium species Large variations in antibiotic susceptibility to the currently available anti-RGM antimicrobials among isolates that apparently belong to the same RGM species has confirmed the need for accurate identification at the species level (Yang et al., 2003; Yakrus et al., 2001). Our results clearly demonstrate that species of the M. mucogenicum group were often more susceptible to antibiotics than species of the M. chelonae–abscessus group. Notable differences were found for antibiotics such as the tetracyclines (minocycline and doxycycline), the macrolides (erythromycin and azithromycin), the quinolones (ciprofloxacin, ofloxacin and sparfloxacin) and imipenem. Amikacin was effective against almost all species. Our data showed that first- and thirdgeneration cephalosporins demonstrated poor activities against members of each group whereas cefoxitin had variable activity. Although the predictive value of in vitro antibiotic susceptibility testing of RGM is uncertain, some anti-RGM antimicrobials could be useful markers for differentiating the three novel species from closely related species. Unlike M. mucogenicum ATCC 49650T, strain U8T was susceptible to tobramycin (MIC<4 mg ml21) and strain N4T was resistant to amoxycillin (MIC >64 mg ml21), amoxycillin/clavulanate (MIC>4 mg ml21) and trimethoprim/ sulfamethoxazole (MIC>8 mg ml21). Strain BDT was resistant to clarithromycin (MIC >256 mg ml21) but M. abscessus was susceptible, even though they shared 100 % similarity in 16S rRNA gene sequences. Recent antibiotic susceptibility testing disturbingly showed that 21–36 % of M. abscessus isolates were resistant to clarithromycin (Yang et al., 2003; Yakrus et al., 2001), making the differentiation of strain BDT and M. abscessus important. In another case, Mycobacterium boenickei and Mycobacterium neworleansense, which share 99?9 % similarity in 16S rRNA gene sequences, differed in their susceptibility to doxycycline and minocycline (Schinsky et al., 2004). These data illustrate that accurate identification of emerging RGM species can reveal the presence of large variations in susceptibility to the currently available antiRGM antimicrobials. The polyphasic approach we adopted showed clear-cut differences between closely related species with identical 16S rRNA gene sequences. Indeed, 16S rRNA gene sequence identity alone is not a useful criterion for the identification of mycobacteria. A review of the 13 novel mycobacterial species described in the 2004 issues of International Journal of Systematic and Evolutionary Microbiology indicated that only 6/13 descriptions of novel species incorporated DNA– DNA hybridization results, including only 4/9 novel species which exhibited greater than 99 % 16S rRNA gene sequence similarity with the most closely related species. Furthermore, DNA–DNA hybridization was performed by only one of the nine research groups that proposed novel species in 2004. These data indicate that the majority of novel mycobacterial species are not described on the basis of DNA–DNA hybridization, even when 16S rRNA gene sequences are almost identical. In these cases, species were described on the basis of one to three other gene sequences. We performed sequence analysis for five different genes in http://ijs.sgmjournals.org the present study. These findings are in agreement with the proposition of the ad hoc committee for re-evaluation of the species definition to sequence five housekeeping genes instead of DNA–DNA hybridization in order to describe novel species (Stackebrandt et al., 2002). Due to the highly conserved nature of the 16S rRNA gene, there is no linear correlation between the DNA–DNA relatedness value and 16S rRNA gene sequence similarity for closely related organisms (Grimont, 1988; Stackebrandt & Goebel, 1994). For example, M. houstonense shared 100 % 16S rRNA gene sequence similarity to M. senegalense but in DNA–DNA hybridization studies, labelled genomic DNA from M. houstonense was <65 % related to that of M. senegalense (Schinsky et al., 2004). Using the rpoB gene as an alternative tool, M. houstonense shared 97?0 % sequence similarity to M. senegalense (Adékambi et al., 2003). This similarity value fulfils the definition of a novel mycobacterial species (Adékambi et al., 2003). Without DNA–DNA hybridization, the rpoB gene has been used for the description of novel mycobacterial species such as ‘M. massiliense’ and M. cosmeticum (Adékambi et al., 2004, Cooksey et al., 2004). Furthermore, recent studies with species of Bartonella, Bosea and Afipia have shown a correlation between DNA– DNA relatedness and rpoB gene sequence similarity for closely related organisms and rpoB gene sequencing has been proposed for the classification of isolates misidentified by 16S rRNA gene sequencing (Khamis et al., 2003; La Scola et al., 2003). A species diagnosis is essential for the management of patients with RGM infections. For example, it is well known that infections with M. abscessus in patients with cystic fibrosis or with chronic meningitis are very difficult to treat (Sanguinetti et al., 2001; Maniu et al., 2001). In some cases, M. abscessus is essentially ineradicable with the possible exception of a resection of the affected lobe of the lung (Griffith et al., 1993; Wallace et al., 1997). Knowledge of the characteristics of mycobacterial species is important for the treatment and prognosis of patients with RGM. Thus, all clinical isolates of RGM should be identified to the species level. Phenotypic characterization, including pigmentation, growth rate, biochemical test algorithms and 16S rRNA gene sequencing, have been used in the identification of Mycobacterium species since the earliest isolation of RGM in clinical specimens. However, rpoB gene sequencing has revealed advantages over both conventional testing and 16S rRNA gene sequence analysis for identifying mycobacterial species and detecting novel species. In keeping with previous findings, it can generally be assumed that a novel species has been detected if base pair discrepancies are found in the variable regions of the rpoB gene and the organism has distinct phenotypic properties (Adékambi et al., 2004). Molecular identification of mycobacteria is a key step towards the description of emerging RGM species and the opportunistic infections they cause. The characteristics of one of the novel species described in this paper, Mycobacterium bolletii sp. nov., also illustrate that accurate Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 139 T. Adékambi and others identification of RGM can be predictive of antibiotic susceptibility patterns of prime clinical value. The present data indicate that selected partial rpoB gene sequencing could be used as a first-line molecular tool for the accurate identification of emerging RGM in man. Description of Mycobacterium bolletii sp. nov. Mycobacterium bolletii (bol9let.i.i. N.L. gen. n. bolletii of Bollet, to honour our deceased colleague Claude Bollet, a famous clinical microbiologist and taxonomist). The organisms are acid-fast and Gram-positive bacilli. Colonies are non-pigmented and appear on 5 % sheep blood agar, Middlebrook 7H10 agar and egg-based LJ slants in 2–5 days at temperatures between 24 and 37 uC, optimally at 30 uC. No growth occurs at 42 uC. This species is a multidrug-resistant mycobacteria, notably to clarithromycin but with intermediate resistance to amikacin. It is associated with chronic pneumonia. It is positive for 3-day arylsulfatase activity, negative for iron uptake and urease activity, does not grow on LJ containing 5 % NaCl at 35 uC and does not utilize citrate, sorbitol or mannitol as sole sources of carbon. It shares 100 % 16S rRNA and 95?6 % rpoB gene sequence similarity with M. abscessus, the closest species. The type strain, BDT (=CIP 108541T=CCUG 50184T), was recovered from sputum. Description of Mycobacterium phocaicum sp. nov. Mycobacterium phocaicum [pho.cai9cum. L. neut. adj. phocaicum pertaining to Phocaea, a maritime town of lonia, a colony of the Athenians, whose inhabitants fled to escape from Persian domination and founded Massilia (Marseille), which was the source of the type strain]. The organisms are acid-fast and Gram-positive bacilli. Colonies are non-pigmented and appear on 5 % sheep blood agar, Middlebrook 7H10 agar and egg-based LJ slants in 2–5 days at temperatures between 24 and 37 uC, optimally at 30 uC. No growth occurs at 42 uC. This species is associated with chronic pneumonia. It is susceptible in vitro to cefoxitin, imipenem, minocycline, doxycycline, clarithromycin, erythromycin, azithromycin, amikacin, ciprofloxacin, ofloxacin and sparfloxacin and is resistant to amoxycillin, amoxycillin/clavulanate and tobramycin. It is positive for 3-day arylsulfatase, nitrate reductase and pyrazinamidase activities and for the production of aesculin and acetoin and negative for iron uptake and urease activity. M. phocaicum differs from M. mucogenicum ATCC 49650T by exhibiting positive activity for penicillinase and alkaline phosphatase and by utilizing citrate as a sole source of carbon. It shares 100 % 16S rRNA and 95?0 % rpoB gene sequence similarity with M. mucogenicum ATCC 49650T, the closest phylogenetic species. 140 The type strain, N4T (=CIP 108542T=CCUG 50185T), was recovered from bronchial aspirate. Description of Mycobacterium aubagnense sp. nov. Mycobacterium aubagnense (au.bag.nen9se. N.L. neut. adj. aubagnense pertaining to Aubagne, the city from where the first patient originated). The organisms are acid-fast and Gram-positive bacilli. Colonies are non-pigmented and appear on 5 % sheep blood agar, Middlebrook 7H10 agar and egg-based LJ slants in 2–5 days at temperatures between 24 and 37 uC, optimally at 30 uC. No growth occurs at 42 uC. This species is associated with chronic pneumonia and sepsis. It is susceptible in vitro to amoxycillin, amoxycillin/clavulanate, cefoxitin, imipenem, minocycline, doxycycline, clarithromycin, erythromycin, azithromycin, amikacin, tobramycin, ciprofloxacin, ofloxacin, sparfloxacin and trimethoprim/sulfamethoxazole. It is positive for 3-day arylsulfatase activity and for the production of aesculin and acetoin, but negative for iron uptake and urease activity. Does not utilize citrate as a sole source of carbon. M. aubagnense differs from M. mucogenicum ATCC 49650T by exhibiting positive alkaline phosphatase activity and no nitrate reductase or pyrazinamidase activity. It shares 99?1 % 16S rRNA and 92?7 % rpoB gene sequence similarity with M. mucogenicum ATCC 49650T, the closest phylogenetic species. The type strain, U8T (=CIP 108543T=CCUG 50186T), was recovered from bronchial aspirate. ACKNOWLEDGEMENTS This work is dedicated to Dr Claude Bollet. We thank Christian de Fontaine for technical assistance, Pierre Yves-Levy for providing mycobacterial isolates and Esther Platt for expert reviewing of the manuscript. REFERENCES Adékambi, T. & Drancourt, M. (2004). Dissection of phylogenetic relationships among 19 rapidly growing Mycobacterium species by 16S rRNA, hsp65, sodA, recA, and rpoB gene sequencing. Int J Syst Evol Microbiol 54, 2095–2105. Adékambi, T., Colson, P. & Drancourt, M. (2003). rpoB-based identification of nonpigmented and late-pigmenting rapidly growing mycobacteria. J Clin Microbiol 41, 5699–5708. Adékambi, T., Reynaud-Gaubert, M., Greub, G., Gevaudan, M.-J., La Scola, B., Raoult, D. & Drancourt, M. (2004). Amoebal co-culture of ‘Mycobacterium massiliense’ sp. nov. from the sputum of a patient with hemoptoic pneumonia. J Clin Microbiol 42, 5493–5501. Anaissie, E. J., Penzak, S. R. & Dignani, M. C. (2002). The hospital water supply as a source of nosocomial infections: a plea for action. Arch Intern Med 162, 1483–1492. Ashford, D. A., Kellerman, S., Yakrus, M., Brim, S., Good, R. C., Finelli, L., Jarvis, W. R. & McNeil, M. M. (1997). Pseudo-outbreak of septicaemia due to rapidly growing mycobacteria associated with Downloaded from www.microbiologyresearch.org by International Journal of Systematic and Evolutionary Microbiology 56 IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 Three novel rpoB-defined Mycobacterium species extrinsic contamination of culture supplement. J Clin Microbiol 35, 2040–2042. Khamis, A., Colson, P., Raoult, D. & La Scola, B. (2003). Usefulness Blackwood, K. S., He, C., Gunton, J., Turenne, C. Y., Wolfe, J. & Kabani, A. M. (2000). Evaluation of recA sequences for identification of rpoB gene sequencing for identification of Afipia and Bosea species, including a strategy for choosing discriminative partial sequences. Appl Environ Microbiol 69, 6740–6749. of Mycobacterium species. J Clin Microbiol 38, 2846–2852. Kim, B. J., Lee, S. H., Lyu, M. A. & 7 other authors (1999). Böddinghaus, B., Rogall, T., Flohr, T., Blöcker, H. & Böttger, E. C. (1990). Detection and identification of mycobacteria by amplifica- Identification of mycobacterial species by comparative sequence analysis of the RNA polymerase gene (rpoB). J Clin Microbiol 37, 1714–1720. tion of rRNA. J Clin Microbiol 28, 1751–1759. Brown, B. A., Wallace, R. J., Jr, Onyi, G. O., De Rosas, V. & Wallace, R. J., III (1992). Activities of four macrolides, including clarithromycin, Kubica, G. P., Dye, W. E., Cohn, M. L. & Middlebrook, G. (1963). against Mycobacterium fortuitum, Mycobacterium chelonae, and M. chelonae-like organisms. Antimicrob Agents Chemother 36, 180–184. Sputum digestion and decontamination with N-acetyl-L-cysteinesodium hydroxide for culture of mycobacteria. Am Rev Respir Dis 87, 775–779. Brown-Elliott, B. A. & Wallace, R. J., Jr (2002). Clinical and Kumar, S., Tamura, K., Jakobsen, I. B. & Nei, M. (2001). MEGA2: taxonomic status of pathogenic nonpigmented or late-pigmenting rapidly growing mycobacteria. Clin Microbiol Rev 15, 716–746. molecular evolutionary genetics analysis software. Bioinformatics 17, 1244–1245. Butler, W. R. & Kilburn, J. O. (1990). High-performance liquid Lai, K. K., Brown, B. A., Westerling, J. A., Fontecchio, S. A., Zhang, Y. & Wallace, R. J., Jr (1998). Long-term laboratory contamination by chromatography patterns of mycolic acids as criteria for identification of Mycobacterium chelonae, Mycobacterium fortuitum, and Mycobacterium smegmatis. J Clin Microbiol 28, 2094–2098. Conville, P. S. & Witebsky, F. G. (1998). Variables affecting results of sodium chloride tolerance test for identification of rapidly growing mycobacteria. J Clin Microbiol 36, 1555–1559. Mycobacterium abscessus resulting in two pseudo-outbreaks: recognition with the use of random amplified polymorphic DNA (RAPD) polymerase chain reaction. Clin Infect Dis 27, 169–175. La Scola, B., Zeaiter, Z., Khamis, A. & Raoult, D. (2003). Gene- sequence-based criteria for species definition in bacteriology: the Bartonella paradigm. Trends Microbiol 11, 318–321. Cooksey, R. C., de Waard, J. H., Yakrus, M. A., Rivera, I., Chopite, M., Toney, S. R., Morlock, G. P. & Butler, W. R. (2004). Mycobacterium Lee, H., Bang, H. E., Bai, G. H. & Cho, S. N. (2003). Novel cosmeticum sp. nov., a novel rapidly growing species isolated from a cosmetic infection and from a nail salon. Int J Syst Evol Microbiol 54, 2385–2391. polymorphic region of the rpoB gene containing Mycobacterium species-specific sequences and its use in identification of mycobacteria. J Clin Microbiol 41, 2213–2218. Covert, T. C., Rodgers, M. R., Reyes, A. L. & Stelma, G. N., Jr (1999). Maniu, C. V., Hellinger, W. C., Chu, S. Y., Palmer, R. & AlvarezElcoro, S. (2001). Failure of treatment for chronic Mycobacterium Occurrence of nontuberculous mycobacteria in environmental samples. Appl Environ Microbiol 65, 2492–2496. Dailloux, M., Laurain, C., Weber, M. & Hartemann, P. H. (1999). abscessus meningitis despite adequate clarithromycin levels in cerebrospinal fluid. Clin Infect Dis 33, 745–748. Water and nontuberculous mycobacteria. Water Res 33, 2219–2228. Mesbah, M., Premachandran, U. & Whitman, W. B. (1989). Precise Dauendorffer, J. N., Guillemin, I., Aubry, A., Truffot-Pernot, C., Sougakoff, W., Jarlier, V. & Cambau, E. (2003). Identification of mycobacterial species by PCR sequencing of quinolone resistancedetermining regions of DNA gyrase genes. J Clin Microbiol 41, 1311–1315. Drancourt, M., Bollet, C., Carlioz, A., Martelin, R., Gayral, J. P. & Raoult, D. (2000). 16S ribosomal DNA sequence analysis of a large collection of environmental and clinical unidentifiable bacterial isolates. J Clin Microbiol 38, 3623–3630. measurement of the G+C content of deoxyribonucleic acid by highperformance liquid chromatography. Int J Syst Bacteriol 39, 159–167. Munoz, M., Julian, E., Garcia-Barcelo, M., Ausina, V. & Luquin, M. (1997). Easy differentiation of Mycobacterium mucogenicum from other species of the Mycobacterium fortuitum complex by thin-layer and gas chromatography of fatty esters and alcohols. J Chromatogr B Biomed Sci Appl 689, 341–347. NCCLS (2002). Performance standards for antimicrobial suscept- ibility testing. Twelfth Informational Supplement, M100-S12. Wayne, PA: NCCLS. Ferguson, D. D., Gershman, K., Jensen, B., Arduino, M. J., Yakrus, M. A., Cooksey, R. C. & Srinivasan, A. (2004). Mycobacterium goodii NCCLS (2003). Susceptibility testing of Mycobacteria, Nocardia, and infections associated with surgical implants at Colorado hospital. Emerg Infect Dis 10, 1868–1871. other aerobic actinomycetes. Approved standard M24-A. Wayne, PA: NCCLS. Fox, G. E., Wisotzkey, J. D. & Jurtshuk, P., Jr (1992). How close is Ninet, B., Monod, M., Emler, S., Pawlowski, J., Metral, C., Rohner, P., Auckenthaler, R. & Hirschel, B. (1996). Two different 16S rRNA close: 16S rRNA sequence identity may not be sufficient to guarantee species identification. Int J Syst Bacteriol 42, 166–170. Griffith, D. E., Girard, W. M. & Wallace, R. J., Jr (1993). Clinical features of pulmonary disease caused by rapidly growing mycobacteria. An analysis of 154 patients. Am Rev Respir Dis 147, 1271–1278. Grimont, P. A. (1988). Use of DNA reassociation in bacterial classification. Can J Microbiol 34, 541–546. genes in a mycobacterial strain. J Clin Microbiol 34, 2531–2536. Park, H., Jang, H., Kim, C., Chung, B., Chang, C. L., Park, S. K. & Song, S. (2000). Detection and identification of mycobacteria by amplification of the internal transcribed spacer regions with genusand species-specific PCR primers. J Clin Microbiol 38, 4080–4085. Pauls, R. J., Turenne, C. Y., Wolfe, J. N. & Kabani, A. (2003). A high Kauppinen, J., Nousiainen, T., Jantunen, E., Mattila, R. & Katila, M. L. (1999). Hospital water supply as a source of disseminated proportion of novel mycobacteria species identified by 16S rDNA analysis among slowly growing AccuProbe-negative strains in a clinical setting. Am J Clin Pathol 120, 560–566. Mycobacterium fortuitum infection in a leukemia patient. Infect Control Hosp Epidemiol 20, 343–345. Reischl, U., Feldmann, K., Naumann, L., Gaugler, B. J., Ninet, B., Hirschel, B. & Emler, S. (1998). 16S rRNA sequence diversity in Kent, P. T. & Kubica, G. P. (1985). Public Health Mycobacteriology: a Mycobacterium celatum strains caused by presence of two different copies of 16S rRNA gene. J Clin Microbiol 36, 1761–1764. guide for the level III laboratory. US Department of Health and Human Services, publication no. (CDC) 86-8230. Atlanta, GA: Centers for Disease Control. http://ijs.sgmjournals.org Ringuet, H., Akoua-Koffi, C., Honore, S., Varnerot, A., Vincent, V., Berche, P., Gaillard, J. L. & Pierre-Audigier, C. (1999). hsp65 Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 141 T. Adékambi and others sequencing for identification of rapidly growing mycobacteria. J Clin Microbiol 37, 852–857. Rogall, T., Flohr, T. & Böttger, E. C. (1990). Differentiation of Mycobacterium species by direct sequencing of amplified DNA. J Gen Microbiol 136, 1915–1920. Sanguinetti, M., Ardito, F., Fiscarelli, E., La Sorda, M., D’Argenio, P., Ricciotti, G. & Fadda, G. (2001). Fatal pulmonary infection due to Tortoli, E. (2003). Impact of genotypic studies on mycobacterial taxonomy: the new mycobacteria of the 1990s. Clin Microbiol Rev 16, 319–354. Tortoli, E., Bartoloni, A., Böttger, E. C. & 8 other authors (2001). Burden of unidentifiable mycobacteria in a reference laboratory. J Clin Microbiol 39, 4058–4065. Turenne, C. Y., Tschetter, L., Wolfe, J. & Kabani, A. (2001). Necessity of multidrug-resistant Mycobacterium abscessus in a patient with cystic fibrosis. J Clin Microbiol 39, 816–819. quality-controlled 16S rRNA gene sequence databases: identifying nontuberculous Mycobacterium species. J Clin Microbiol 39, 3637–3648. Sasser, M. (1990). Identification of bacteria by gas chromatography Vincent, V., Brown-Elliot, B. A., Jost, K. C., Jr & Wallace, R. J., Jr (2003). Mycobacterium: phenotypic and genotypic identification. In of cellular fatty acids. MIDI technical note no. 101. Newark, DE: MIDI. Schinsky, M. F., Morey, R. E., Steigerwalt, A. G. & 10 other authors (2004). Taxonomic variation in the Mycobacterium fortuitum third Manual of Clinical Microbiology, 8th edn, pp. 560–584. Edited by P. M. Murray, E. J. Baron, J. H. Jorgensen, M. A. Pfaller & R. H. Yolken. Washington, DC: American Society for Microbiology. Wallace, R. J., Jr, Bedsole, G., Sumter, G., Sanders, C. V., Steele, L. C., Brown, B. A., Smith, J. & Graham, D. R. (1990). Activities of biovariant complex: description of Mycobacterium boenickei sp. nov., Mycobacterium houstonense sp. nov., Mycobacterium neworleansense sp. nov. and Mycobacterium brisbanense sp. nov. and recognition of Mycobacterium porcinum from human clinical isolates. Int J Syst Evol Microbiol 54, 1653–1667. ciprofloxacin and ofloxacin against rapidly growing mycobacteria with demonstration of acquired resistance following single-drug therapy. Antimicrob Agents Chemother 34, 65–70. Smith, M. B., Schnadig, V. J., Boyars, M. C. & Woods, G. L. (2001). Wallace, R. J., Jr, Brown, B. A. & Onyi, G. O. (1991). Susceptibilities of Clinical and pathologic features of Mycobacterium fortuitum infections. An emerging pathogen in patients with AIDS. Am J Clin Pathol 116, 225–232. Mycobacterium fortuitum biovar. fortuitum and the two subgroups of Mycobacterium chelonae to imipenem, cefmetazole, cefoxitin, and amoxicillin-clavulanic acid. Antimicrob Agents Chemother 35, 773–775. Soini, H. & Viljanen, M. K. (1997). Diversity of the 32-kilodalton protein gene may form a basis for species determination of potentially pathogenic mycobacterial species. J Clin Microbiol 35, 769–773. Wallace, R. J., Jr, Silcox, V. A., Tsukamura, M., Brown, B. A., Kilburn, J. O., Butler, W. R. & Onyi, G. (1993). Clinical significance, biochem- ical features, and susceptibility patterns of sporadic isolates of the Mycobacterium chelonae-like organism. J Clin Microbiol 31, 3231–3239. Springer, B., Stockman, L., Teschner, K., Roberts, G. D. & Böttger, E. C. (1996). Two-laboratory collaborative study on identification of Wallace, R. J., Jr, Glassroth, J., Griffith, D. E., Olivier, K. N., Cook, J. L. & Gordin, F. (1997). Diagnosis and treatment of disease caused by mycobacteria: molecular versus phenotypic methods. J Clin Microbiol 34, 296–303. Wallace, R. J., Jr, Brown, B. A. & Griffith, D. E. (1998). Nosocomial Stackebrandt, E. & Goebel, B. M. (1994). Taxonomic note: a place for DNA-DNA reassociation and 16S rRNA sequence analysis in the present species definition in bacteriology. Int J Syst Bacteriol 44, 846–849. Stackebrandt, E., Frederiksen, W., Garrity, G. M. & 10 other authors (2002). Report of the ad hoc committee for the re-evaluation of the species definition in bacteriology. Int J Syst Evol Microbiol 52, 1043–1047. nontuberculous mycobacteria. Am J Resp Crit Care Med 156, S1–S15. outbreaks/pseudo-outbreaks caused by nontuberculous mycobacteria. Annu Rev Microbiol 52, 453–490. Wallace, R. J., Jr, Zhang, Y., Wilson, R. W., Mann, L. & Rossmore, H. (2002). Presence of a single genotype of the newly described species Mycobacterium immunogenum in industrial metalworking fluids associated with hypersensitivity pneumonitis. Appl Environ Microbiol 68, 5580–5584. Weisburg, W. G., Barns, S. M., Pelletier, D. A. & Lane, D. J. (1991). Swenson, J. M., Wallace, R. J., Jr, Silcox, V. A. & Thornsberry, C. (1985). Antimicrobial susceptibility of five subgroups of Myco- 16S ribosomal DNA amplification for phylogenetic study. J Bacteriol 173, 697–703. bacterium fortuitum and Mycobacterium chelonae. Antimicrob Agents Chemother 28, 807–811. Wilson, R. W., Steingrube, V. A., Böttger, E. C. & 11 other authors (2001). Mycobacterium immunogenum sp. nov., a novel species Takewaki, S. I., Okuzumi, K., Manabe, I., Tanimura, M., Miyamura, K., Nakahara, K. I., Yazaki, Y., Ohkubo, A. & Nagai, R. (1994). related to Mycobacterium abscessus and associated with clinical disease, pseudo-outbreaks and contaminated metalworking fluids: an international cooperative study on mycobacterial taxonomy. Int J Syst Evol Microbiol 51, 1751–1764. Nucleotide sequence comparison of the mycobacterial dnaJ gene and PCR-restriction fragment length polymorphism analysis for identification of mycobacterial species. Int J Syst Bacteriol 44, 159–166. Telenti, A., Marchesi, F., Balz, M., Bally, F., Böttger, E. & Bodmer, T. (1993). Rapid identification of mycobacteria to the species level by Winthrop, K. L., Abrams, M., Yakrus, M., Schwartz, I., Ely, J., Gillies, D. & Vugia, D. J. (2002). An outbreak of mycobacterial furunculosis associated with footbaths at a nail salon. N Engl J Med 346, 1366–1371. polymerase chain reaction and restriction enzyme analysis. J Clin Microbiol 31, 175–178. Woods, G. L., Bergmann, J. S., Witebsky, F. G., Fahle, G. A., Boulet, B., Plaunt, M., Brown, B. A., Wallace, R. J., Jr & Wanger, A. (2000). Multisite reproducibility of Etest for susceptibility testing Thompson, J. D., Gibson, T. J., Plewniak, F., Jeanmougin, F. & Higgins, D. G. (1997). The CLUSTAL_ X windows interface: flexible of Mycobacterium abscessus, Mycobacterium chelonae, and Mycobacterium fortuitum. J Clin Microbiol 38, 656–661. strategies for multiple sequence alignment aided by quality analysis tools. Nucleic Acids Res 25, 4876–4882. Yakrus, M. A., Hernandez, S. M., Floyd, M. M., Sikes, D., Butler, W. R. & Metchock, B. (2001). Comparison of methods for identification of Tiwari, T. S., Ray, B., Jost, K. C. Jr, Rathod, M. K., Zhang, Y., Brown-Elliott, B. A., Hendricks, K. & Wallace, R. J., Jr (2003). Forty Mycobacterium abscessus and M. chelonae isolates. J Clin Microbiol 39, 4103–4110. years of disinfectant failure: outbreak of postinjection Mycobacterium abscessus infection caused by contamination of benzalkonium chloride. Clin Infect Dis 36, 954–962. Yang, S. C., Hsueh, P. R., Lai, H. C. & 7 other authors (2003). High 142 prevalence of antimicrobial resistance in rapidly growing mycobacteria in Taiwan. Antimicrob Agents Chemother 47, 1958–1962. Downloaded from www.microbiologyresearch.org by International Journal of Systematic and Evolutionary Microbiology 56 IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 Three novel rpoB-defined Mycobacterium species Zelazny, A. M., Calhoun, L. B., Li, L., Shea, Y. R. & Fischer, S. H. (2005). Identification of Mycobacterium species by secA1 sequences. J Clin Microbiol 43, 1051–1058. http://ijs.sgmjournals.org Zolg, J. W. & Philippi-Schulz, S. (1994). The superoxide dismutase gene, a target for detection and identification of mycobacteria by PCR. J Clin Microbiol 32, 2801–2812. Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 04 Aug 2017 01:43:39 143