* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download B-catenin
Long non-coding RNA wikipedia , lookup
Epigenetics in stem-cell differentiation wikipedia , lookup
History of genetic engineering wikipedia , lookup
Gene expression programming wikipedia , lookup
Gene expression profiling wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Mir-92 microRNA precursor family wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Wnt signaling pathway wikipedia , lookup
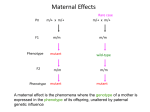
Diabetes Mellitus Type II Beta Cell Failure in DM T2 signaling pathways implicated in β-cell failure Controls organismal growth and differentiation Wnt Signaling Pathway Wnt signalling Pathway and DM T2 1. Homozygous mutation of LRP5 in mice leads to defective glucose-stimulated insulin secretion from isolated islets in vitro. 2. Components of the Wnt pathway are present in the adult pancreas, and in particular multiple members of the frizzled family of Wnt receptors have been identified in the islet. 3. TCF7/L2 gene polymorphism affects B-cell function While most studies have found little evidence that Wnt signaling is involved in endocrine differentiation or in the adult islet, there is some evidence for an effect of Wnt signaling on β-cell replication. Main Objective To study the role of Wnt signaling in human diabetes Systematically examined components of the pathway in the pancreas of normal & DMT2 Mouse Studies METHODS TISSUE PREPARATION 1. Paraffin-embedded from human pancreases: 5 non-diabetic & 9 DM T2 2. Freshly isolated & cultured pancreases: 3 non-diabetic (Isolated human islets) 3. Human Fetal Pancreases in 18-24 gestational weeks 4. Murine Pancreaes (Balb/c or C57/bl mice) 5. NEPCs IMMUNO-HISTOCHEMISTRY 1. Paraffin samples 2. Frozen samples WESTERN BLOT 1. Whole-cell extracts I. Objective: To determine if TCF7L2 is upregulated in islets of type II diabetic patients •TCF7L2 is a protein acting as a transcription factor. •Several SNPs of the gene are associated with Type 2 DM TCF/L2 TCF3 TCF7L2 is upregulated in islets of type II diabetic patients II. Objective: To determine if Wnt2b is upregulated in type II diabetes To test the hypothesis that the induction of TCF factors, being a both effector as well as a downstream target of Wnt Signaling, is a result of a more global activation of Wnt signaling B Catenin Wnt2b Wnt 2b is upregulated in Type 2 Diabetes In islets III. Objective: To determine if B-catenin is upregulated in type II diabetes B-catenin B-catenin insulin Human B-cellsB-Catenin lack In islets Detectable B-catenin expression but it is highly upregulated in DM T2 islet Normal Normal Beta-catenin in human islets of all 5 nondiabetics was markedly lower Than in the surrounding exocrine Tissue where it was strongly Expressed (figs. 2f-2h) insulin insulin DM T2 B-catenin B-catenin DM T2 Beta-catenin is strongly expres in the islets of all DM T2 to a Level approximately half that of the Surrounding exocrine tissue (figs 2h-2j) IV. Objective: To determine if the terminal effectors (c-myc & cyclin D) are upregulated in DM T2 TCF/LEF factors activate a number of terminal effectors Of Wnt signaling (c-myc and cyclinD1) c NORMAL Terminal effectors of CyclinD1 C-myc Wnt signaling In islets DM T2 In(c-myc islets & cyclinD1) are upregulated in human type 2 Diabetes MOUSE MODEL V. Objective: To determine whether Wnt activation was an early or late event in diabetes pathogenesis normal chow high-fat diet 12 weeks OBESE BUT WITH NORMAL FBS Harvested pancreases examined for c-myc expression High-fat Expression of the Wnt target gene c-myc is an early response to high-fat diet Normal B -catenin Normal C-myc Normal Normal Islets High-Fat Figure 6: Wnt signaling in high-fat fed mice. •In normal mouse pancreas, β-catenin (green in (a) and (b)) is expressed in islets as identified by somatostatin (red in (a)) and colocalizes with insulin (red in (c)). •C-myc (red in (d) and (e)) was not expressed in islets of normal mice (marked by dotted lines and glucagon in green in (d)) • but was induced in islets and some ducts of high-fat fed mice (islets marked by glucagon in green). •C-myc expression is quantitated in (f). Summary 1. B-catenin in human islets of all 5 nondiabetics was markedly lower than in the surrounding exocrine tissue, where it was strongly expressed. 2. Expression of the Wnt2b, B-catenin, TCF7/L2, & terminal effectors (c-myc & cyclinD1) are all upregulated in the islets in type II diabetes 3. The mouse model suggested that obesity alone may be sufficient to induce Wnt activation, which would mark it as an early event in the pathogenesis of type II diabetes. Conclusion Type II Diabetes activates the Wnt signaling pathway specifically in the Beta cells of the islets of Langerhans Thank You!!! • Immunohistochemical analysis of insulin (green) and anti-sFRP (red in (f) and (g)) detects sFRP on islet cells only when sFRP has been added to the culture media. • sFRP exposure led to inhibition of β-catenin ((h) versus (i), quantitated in (j)) and c-myc ((k) versus (l), quantitated in (m)). • Error bars = mean +/−s.e.m. ∗P < .05. Scale bars in (f)–(m): 25 μm. • To pursue the role of Wnt activation in the islet, it would be desirable to have an in vitro model. Thus, we examined Wnt activation in isolated islets. • Surprisingly, when cultured human islets were examined by Western blotting, βcatenin, which is low or absent in the islet compared with surrounding tissue in situ, was expressed at a higher level than in the nonendocrine pancreatic cells (NEPCs) [23] (Figure 4(a)). • To pursue the finding that β-cells with lowinsulin expression had a pattern of catenin expression resembling that in the exocrine pancreas, pancreas sections were immunostained for the acinar marker amylase as well as insulin, revealing that low-insulin βcells coexpressed amylase (Figures 5(f), 5(g), 5(h)). • The insulin/amylase doublepositive cells expressed PDX-1 (Figure 5(i)), which in the adult pancreas is restricted to β-cells and is never expressed in mature acinar cells, indicating that the weak insulin expression was not artifactual. • To further explore whether the areas containing the insulin/amylase double-positive cells arose by alteration of preexisting β-cells or by induction of insulin expression in preexisting exocrine cells, as has been described in some β- cell regeneration models [37–39], we examined those areas for glucagon expression. • Consistently, high levels of glucagon and a lack of amylase were observed in all α-cells, whether the islets exhibited high or low insulin expression (Figure 5(l)). • Figure 1. Schematic representation of WNT/TCF signalling. Secreted WNTs bind to FZD and LRP receptors, which in turn inactivate the degradation complex comprising AXIN, DVL and GSK3B. • This results in non-phosphorylated b-catenin entering into the nucleus and binding to TCF7L2, thus activating a wide variety of genes. • TCF7L2 could regulate several genes – tissue specifically influencing both insulin secretion and insulin sensitivity. For example, TCF7L2 regulates b-cell growth and differentiation. TCF7L2 also activates the expression of proglucagon gene, which encodes the GLP-1 (glucagons like peptide-1) and thus promotes insulin secretion. Alterations in this pathway (in TCF7L2 risk variants) could lead to reduced secretion of GLP-1 and hence defective insulin secretion. • In addition, altered WNT signalling (in TCF7L2 risk variants) could be expected to influence adipose tissue growth and development and thus BMI. Increased pro-inflammatory signals (IL-6, TNF-a) and altered adiponectin from the adipocytes (through their endocrine function) might result in skeletal muscle insulin resistance. With regard to microvascular complications of diabetes, TCF7L2 may also influence mesangial cell expansion and retinal neovascularization.