* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cells
Molecular mimicry wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
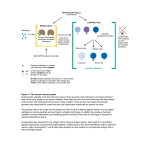
Innate immunity Cells of nespecific immunity, phagocytosis Module IB, Cell Blood cells lineage Structure of the immune system • • • • Lymphoid stem cells Myeloid stem cells They will develop in mature immune cells Human immune system is formed by – 1012 cells – 1014 various molecules, usually proteins • Dispersity - cells will localize whole body • Movement during development and effector function Proportion of types of white cells in periphery, adult healthy man Cell type Neu granulo Proportion (%) 60-70 Eo granulo 1-3 Baso granulo 0-2 Mono 5-10 Lympho 20-40 First level of defense • To establish an infection, the pathogen must to overcome barriers – the skin, which is impermeable to most agents a secretes anti-bacterial fatty acids – Mucus secretion blocks adherence to epithelial cells. • Many secreted fluids are bactericidal – lysozyme, spermine, gastric acid • Gut commensals may block growth of pathogenic bacteria Second level of defense • Immune reaction Primary lymphatic organs • Thymus - maturation of immune cells • environment for T lymphocytes development – epithelial cells, thymus hormones. Lymphoid cells (similar to blasts) • Bone marrow – source and maturation of immune cells, dominantly B cells (equivalent to Bursa Fabricii in birds) Secondary lymphatic tissues • Lymph nodes • Spleen • Mucosa associated lymphoid structure (MALT) – Diffuse • BALT - following principal bronchi, M cells are near trachea bifurcation, most cells are B cells • GALT - Peyer plaques, isolated lymphatic follicles, covered by lymphoepitelial cells – M cells • NALT – Nasal lymphoid tissue – Organised aggregates of folicules: tonsils, Peyer plaques, appendix Primary and secondary lymphoid organs – body localization Lymphoid elements of the intestinal immune system – inductive and effector site Inductive site – contact with the Ag. Germinal centers - differentiation of B cells Effector site – mast cells MC mucosal – tryptase MC conective tissue – typtase + chymase CD4+8+ T cells, IEL are T cells Traffic of immune cells General Types of Immunity • Innate (natural) – First line of defense – No previous exposure to agent required – Nonspecific • Physical and chemical mechanical barriers • Adaptive (acquired) – Specific response to infectious agent – Immunological memory for invader Innate Immunity • Physical and chemical barriers – Intact skin – effective physical barrier • Low pH – bactericidal for many organisms • Normal skin flora – helps prevent colonization by pathogens – Loss of normal flora allows resistant organisms or fungi to proliferate Innate Immunity, Cont. • Mucous membranes of respiratory, gastrointestinal, and urogenital tracts – Ciliated epithelial cells – trap and sweep away airborne particles and organisms – Goblet cells – produce mucus to make epithelial surface sticky – Enzymes in secretions inhibit invasion by organisms Innate Immunity, Cont. Innate immune defenses located at different body sites. Innate Immunity, Cont. • Plasma proteins – antimicrobial and antiviral effects – Acute phase reactants – Complement system: cascades and components – Cytokines – ex. Tumor necrosis factor alpha (TNF) – Interferons (IFN) – Opsonins – fibronectin Cells of the Immune System, Cont. • Leukocyte (WBC), phago cells – Phagocytic cells primary to host defense • Granulocytes – Neutrophil • Monocyte/Macrophage – Natural Killers – Auxiliary cells • Eosinophils • Basophils • Mast cells Cells of innate immunity • • • • • Macrophages are phagocytes that are constitutively present in tissues and respond rapidly to microbes that enter these tissues. Neutrophils, an abundant type of phagocyte, and monocytes, the precursors of tissue macrophages, are always present in the blood and can be quickly delivered anywhere in the body. Almost all tissues contain dendritic cells, which are APCs that are specialized to capture microbial antigens, to transport them to lymphoid tissues, and to present them for recognition by lymphocytes. Naive lymphocytes (lymphocytes that have not previously encountered antigens) migrate through these peripheral lymphoid organs, where they recognize antigens and initiate adaptive immune responses. The anatomy of lymphoid organs promotes cell-cell interactions that are required for antigen recognition by lymphocytes and for the activation of naive lymphocytes, resulting in the generation of effector and memory lymphocytes. Effector and memory lymphocytes circulate in the blood, home to peripheral sites of antigen entry, and are efficiently retained at these sites. This ensures that immunity is systemic (i.e., that protective mechanisms can act anywhere in the body). Characteristics of innate immunity fylogenetically conserved identification of „danger“ patterns determines „context“ for specific immunity INNATE IMMUNITY ontogenically conserved relationship to other systems immediate reactivity Adaptive immune response • Antigen specific B cells – immunoglobulin secretion, Ag specific antibodies are responsible for eliminating invading microorganism • T cells help B cells to produce antibodies, eradicate IC pathogens - activating Mo, direct killing • Antigen presenting cells - they display the antigen to lymphocytes and collaborate with them in the response Innate and Adaptive Immune response - summary Feature Phyllogenic age Main target Physical barriers Soluble factors Nonspecific Specific Phylogenetically old, conserved struct. Young „Common“ infectious agents Persistent infect. skin and mucosal membranes none enzymes (lysozyme, complement) antibodies Acute phase reaction proteins (CRP) Cytokines (IF) Cells Macrophages, PMN, NK cells T and B cells Foreign recognition “identification“ of dangerous patterns specific – „foreign“ Target structures PAMPs, conservative structural details – epitopes Recognition struct. Membrane PRR (TLR), solubile PRR membrane BCR, TCR, antibodies Receptor distrib. Non-clonal, all cells of one type clonal Specificity no yes Memoryno yes Innate and acquired immune response work together to recognize antigens (and eliminate pathogens) PHAGOCYTOSIS cell factor of innate immunity macrophages presentation of antigens dendritic cells granulocytes source of cytokines ingestion of microbes PHAGOCYTOSIS is the ability of specialised cells: to engulf to kill to destroy microbes and foreign particules Multistep leukocyte-endothelial interactions mediating leukocyte recruitment into tissues Adhesion molecules Adhesion mol. Ligand Relevance Defective expression Selectin family CD15 Transient adhesion and rolling Defective on Neu, Eo, Mono CD15 expression of Leu on endothelium - severe ID, similar to CD18 def L-selectin CD34, GlyCAM on high Transient adhesion for (CD62L) rolling endothelial venules No human disease homing molecule - lymph nodes Immunoglobulin super-gene family strengthen the interaction btw APC and T cells ICAM 1, 2, 3, CD28 – CD80, 86, TCR, BCR, MHC I and II Adhesion molecules and leukocyte-endothelial interaction β2 integrin family – leukocyte integrins Adhesion mol. Ligand Clin rel. of interaction CD18/CD11 all Neu ICAM-1 on endothelium Tight adhesion btw leuko and endothelium Defective expression Severe ID – leucocytosis, bacterial, fungal infection ACTIVATION OF PHAGOCYTES ENDOGENOUS: proinflammatory cytokines chemokines CSF C3a C5a PAF LT EXOGENOUS: bacterial components LPS, CpG, „danger patterns“ (PAMP) Characteristics of innate immunity ACTIVATION • receptors directed against high number of structures on microorganisms • germline coded receptors (in opposition to: BCR, TCR – individual, not inherited) • only few genes for those receptors • receptors for limited number of conserved molecular patterns (common for microorganisms, distinguishable from self patterns) – Pathogen Associated Molecular Patterns - PAMPs Pattern recognition receptors (PRR) PAMP LPS Lipoproteins Peptidoglycan Lipoarabinom annan Flagellin CpG (bacterial DNA) Heat shock proteins Microbes Most G - bacteria Most bacteria Most bacteria mycobacteria PRR LBP, CD14, TLR4 TLR2 CD14, TLR2 TLR2, MBP G- bacteria Most bacteria TLR5 TLR9 Most bacteria TLR4, TLR2 Toll - like receptors • Example of PRRs • TLRs originally described in insects • Mammalian cells use to identify important bacterial components - LPS, CpG • After activation, TLR activate transcription factors - activation of immune response genes • Toll-like receptors, after PAMP recognition, activate signaling pathways inducing antimicrobial effector response Structure, Location, and Specificities of TLRs Fig. 4-2 © 2011 by Saunders, an imprint Elsevier Inc. Abbas, Lichtman, and Pillai. Cellular and Molecular Immunology, 7th edition. Copyright © 2012Copyright by Saunders, an imprint of ofElsevier Inc. Toll-like receptor (TLR)-mediated innate and adaptive immune responses and their roles in the immune system. • Clinical relevance of TLR • Toll-like receptors – role in the initiation of human diseases and represent potential targets for therapeutic intervention. – TLR ligands serve as components of common vaccine adjuvants – TLR9 recognition of nucleic acids may help trigger systemic lupus erythematosus and rheumatoid arthritis – TLR 1, 2, 4, and 5 are expressed in atherosclerotic plaques – TLR agonists can skew the immune response from a Th2allergic immune phenotype to a protective Th1 immune phenotype in asthma DRUGS WHICH STIMULATE TOLL-LIKE RECEPTORS • In several situations, it is desirable to stimulate the immune system. For example, it would be helpful to boost the immune response to cancers and some vaccines. Drugs have been developed which bind Toll-like receptors and give additional stimulus to the immune system. • For example, CpG is an unmethylated DNA sequence normally only found in bacteria. CpG binds to TLR9 and by activating the immune system can be used to help to treat cancers and improve responses to vaccines. 1. Phagocytes – granulocytes (neutrophil) Phagocytes, including neutrophils and macrophages, are cells whose primary function is to identify, ingest, and destroy microbes - typical effector cells - short lived cells - Chemotaxis - Killing mechanisms - – pH, enzymes: proteinases - elastase, kolagenase, gelatinase, lysozyme, kathepsin G, defensine, - oxygen radicals – metabolic burst lipid mediators- inflammatory cells influx (LTB4, PAF, TxA2) Neutrophils • Neutrophils, also called polymorphonuclear leukocytes, are the most abundant population of circulating white blood cells and mediate the earliest phases of inflammatory reactions • Major role – remove infectious agents • Most abundant cell in circulation – Normal – 55-75% of total WBCs • Nucleus – Mature PMN – multi-lobed (segmented) – Immature PMN – nonsegmented “bands” Neutrophils, Cont. (a) (b) FIGURE 2-2 (a) Segmented neutrophil, peripheral blood, Wright stain; (b) Segmented neutrophil and macrophage in Gram-stained smear. 2. Phagocytes – Monocytes, Macrophages Monocytes and macrophages develop from immature hemopoetic progenitor cells in the bone marrow. Mature monocytes enter to the circulation, resident macrophages are located in the tissue Monocytes and macrophages express class II MHC antigens (HLA DR, DP, DQ) Receptors for „foreign structures“ (PRR: TLR, lectins) Opsonisation: Fc receptors Complement receptors, CR 1 – 3 • The mononuclear phagocyte system consists of cells whose primary function is phagocytosis and that play central roles in innate and adaptive immunity • Once they enter tissues, these monocytes mature and become macrophages. Macrophages in different tissues have been given special names to designate specific locations Cellular components of innate immune response - Mononuclear phagocyte cells Maturation of mononuclear phagocytes and dendritic cells 3. Dendritic cells • Dendritic cells are the most important APCs for activating naive T cells, and they play major roles in innate responses to infections and in linking innate and adaptive immune responses. • They have long membranous projections and phagocytic capabilities and are widely distributed in lymphoid tissues, mucosal epithelium, and organ parenchyma Interdigitating dendritic cells constantly, quietly endocytose extracellular antigens • They became activated and behave as APC (when PAMP is recognized - LPS, mannose) • Activated by endogenous signal - release of IFN- (from virally infected cells), HSP from necrotic cells • Activation of DC will cause expression of B7 - costimulatory molecules ROLE OF DENDRITIC CELL IN INNATE IMMUNITY capture and processing of antigens in tissues DENDRITIC CELL migration into lymphatic nodes presentation of antigens to T cells Interactions between epithelial cells and dendritic cells in the airways • Dendritic cells (DCs) sample the airway lumen by forming dendritic extensions between epithelial cells. • DCs form tight junctions with epithelial cells through their expression of occludin (not shown) and claudin family members, as well as zonula occludens 1 (ZO1). Follicular Dendritic Cells • Follicular dendritic cells (FDCs) are cells with membranous projections that are found intermingled in specialized collections of activated B cells, called germinal centers, in the lymphoid follicles of the lymph nodes, spleen, and mucosal lymphoid tissues. • FDCs are not derived from precursors in the bone marrow and are unrelated to the dendritic cells that present antigens to T lymphocytes. • FDCs trap antigens complexed to antibodies or complement products and display these antigens on their surfaces for recognition by B lymphocytes. This is important for the selection of activated B lymphocytes whose antigen receptors bind the displayed antigens with high affinity Opsonisation of antigen – the role of antibody, complement etc. Phagocytosis ingestion INGESTION GRANULOCYTE BACTERIA Ig FcR Ag A C T I V A T I O N C3b CR lectin sacharide lectinophagocytosis T cell Activation by an Activated APC IL-1 IL-6 IL-12 IL-12 Receptor CD28 “Signal 3” CD4+ B7 T cell LPS T Cell Receptor “Signal 2” TLR4 “Signal 1” Peptide MHC II Signal 1: Specificity Signal 2: Activation Signal 3: Differentiation Antigen Presenting Cell (APC) Monocytes, macrophages and DC versus Neutrophils • Monocytes, macrophages and dominantly dendritic cells are capable to present Ag efficiently • Neutrophils do not present Ag! NK cells • Natural killer (NK) cells are lymphocytes distinct from T and B cells • important roles in innate immune responses mainly against intracellular viruses and bacteria. Natural killer cells destroy infected and malignant cells • The term natural killer derives from the fact that these cells are capable of performing their killing function without a need for clonal expansion and differentiation, which is required for effector responses of the immune system's other killer cells, the cytotoxic T lymphocytes (CTLs). 1. Possess Fc receptors that bind IgG: FcR - link to IgG coated target cells (process called antibody dependent cellular cytotoxicity ADCC) 2. The killer activating receptors recognize a number of different molecules, killer inhibitory molecules recognize MHC-I Functions of activating and inhibitory receptors of NK cells Granulocytes • A Neutrophil • B Mast cell • C Basophil • D Eosinophil Other inflammatory cells - function • Neutrophils – release enzymes - proteinase (elastase, kolagenase), oxygen radicals, lipid mediators • Eosinophils – weak phagocytes – on activation, kill parasites by releasing cationic proteins, reactive oxygen metabolites – secrete leukotrienes, prostaglandins, various cytokines • Basophils and mast cells - blood basophils do not develop into the tissue mastocytes. – On activation, (FcR) secrete inflammatory mediators Eosinophils • Eosinophils are blood granulocytes that express cytoplasmic granules containing enzymes that are harmful to the cell walls of parasites but can also damage host tissues • Some eosinophils are normally present in peripheral tissues, especially in mucosal linings of the respiratory, gastrointestinal, and genitourinary tracts, and their numbers can increase by recruitment from the blood in the setting of inflammation. Eosinophil migration to sites of allergic inflammation Mast cells • Mast cells are bone marrow-derived cells that are present in the skin and mucosal epithelium and contain abundant cytoplasmic granules filled with cytokines histamine, and other mediators. • Stem cell factor (also called c-Kit ligand) is a cytokine that is essential for mast cell development Basophils • Basophils are blood granulocytes with many structural and functional similarities to mast cells. • Like other granulocytes, basophils are derived from bone marrow progenitors (a lineage different from that of mast cells), mature in the bone marrow, and circulate in the blood. • Although they are normally not present in tissues, basophils may be recruited to some inflammatory sites. • Like mast cells, basophils express IgG and IgE receptors, bind IgE, and can be triggered by antigen binding to the IgE. • Because basophil numbers are low in tissues, their importance in host defense and allergic reactions is uncertain. Activation of mast cells and basophils The signal-transduction cascade induced after FcεRI aggregation