* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download HH15_Reproductive organs
Testosterone wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Hormone replacement therapy (female-to-male) wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Progesterone wikipedia , lookup
Hyperandrogenism wikipedia , lookup
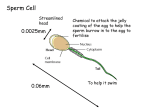
Hypothalamus wikipedia , lookup
Ch15: Sex Organs & Hormonal Control Higher Human Biology Male Reproductive System Testes are the site of: • sperm production • manufacture of the male sex hormone testosterone Sperm Production Sperm are formed by meiosis in the tiny seminiferous tubules of the testes, which unite forming coiled tubes that connect to the sperm duct. Sperm duct Sperm forming by meiosis Pathway of sperm Pathway of sperm during sexual intercourse Sperm are motile. This requires a fluid medium & a source of energy. Image source: www.fertility.com Testosterone ….the male sex hormone • Produced by interstitial cells, in the tissue between the seminiferous tubules of the testes • Released directly into the bloodstream Image source: http://faculty.une.edu Seminal Vesicles Males have 2 seminal vesicles, which secrete a thick liquid rich in: • fructose – a sugar that provides sperm with energy for motility • prostaglandins – hormone-like compounds that stimulate contractions of the female reproductive tract. Help sperm to move more quickly towards the egg. Prostate Gland Secretes a thin lubricating liquid containing enzymes. The enzymes keep the fluid at the optimum viscosity (thickness) for sperm motility. Semen is a milky liquid composed of: •sperm, •fluid from seminal vesicles •fluid from prostate gland Female Reproductive System Oviduct / Egg tube Where the egg is fertilised Ovary Produces eggs Uterus / Womb Where the baby grows Vagina The penis is put here when mating. Uterus lining Lining of the womb Cervix The neck of the uterus which connects to the vagina. Developing Egg Eggs are formed by meiosis in the ovaries. Each ovum (egg) is contained by a developing Graafian follicle which secretes oestrogen (a hormone). After ovulation (release of the egg), the Graafian follicle develops into a corpus luteum which secretes the hormone progesterone. Image source: http://resources.schoolscience.co.uk Hormones Hormones are chemical messengers, produced in the endocrine (ductless) glands (e.g. pituitary and thyroid glands) then secreted into the bloodstream. Thyroid gland Pituitary gland When a hormone reaches its target tissue it brings about a specific effect Gonadotrophic hormones The gonads (reproductive organs) are the target organs of two of the hormones produced by the pituitary gland, thus these hormones are called gonadotrophic hormones: 1. FSH: follicle-stimulating hormone 2. ICSH: interstitial cellstimulating hormone (males) LH: Luteinising hormone (females) These hormones begin to be released from the anterior pituitary at puberty. Male Gonadotrophic hormones The functions of the testes are regulated by these hormones: FSH Anterior (front) lobe In bloodstream stimulates interstitial cells to produce ICSH testosterone promotes sperm production in the seminiferous tubules Testosterone Activates secretion from prostate gland + seminal vesicles Self Regulation of Testosterone The body has self-regulating mechanisms, called negative feedback control, that allows the body to correct changes. When the concentration of testosterone gets to a certain level it inhibits the secretion of FSH & ISCH, which in turn causes a decrease in testosterone concentration. Negative Feedback Control When a factor affecting the body’s internal environment deviates from its norm (or set-point) the body responds to correct the change. Image source: www.hw.ac.uk Female Gonadotrophic hormones FSH stimulates: • Development and maturation of each Graafian follicle • Secretion of oestrogen from ovary tissue LH triggers: • Ovulation • Development of corpus luteum • Secretion of progesterone Oestrogen & Progesterone are the ovarian hormones. Oestrogen Oestrogen stimulates: • cell division (proliferation) of the endometrium (inner layer of the uterus) allowing it to repair after menstruation. • the secretion of LH by the anterior pituitary Image source: www.beliefnet.com Progesterone Progesterone stimulates: • the thickening of the endometrium • inhibits the secretion of FSH & LH by the anterior pituitary Effect of Hormones in females GnRH = Gonadotrophin Releasing Hormone Menstrual Cycle • 28 day cycle • each cycle continuous with previous cycle and next cycle Ovulation • 2 phases View the animation on menstruation: http://resources.schoolscience.co.uk/abpi/n Endometrium ew/resources/hormones/horm4.asp Image source: www.medicine4faith.net follicular phase luteal phase Menstrual Cycle: Follicular Phase • First half of cycle • FSH from pituitary stimulates development & maturation of a Graafian follicle and production of oestrogen from ovarian tissues • Repair & proliferation of the endometrium (due to increase in Oestrogen) • At day 14 - high Oestrogen levels cause a surge in the production of LH (& FSH) causing ovulation. Ovulation • Occurs on day 14 • Surge in LH causes the wall of the Graafian follicle to rupture & release the egg • after ovulation the egg moves along the oviduct • for 3-4 days the egg can be fertilised if it meets a sperm Ruptured follicle Protective cells Egg Menstrual Cycle: Luteal Phase FSH LH oestrogen • Second half of cycle • LH stimulates Graafian follicle to become corpus luteum, which then secretes oestrogen & progesterone • Endometrium becomes thick, vascular & spongy, due to increase in progesterone, ready to accept & nourish the embryo if fertilisation has occured • FSH drops due to high oestrogen + progesterone so no new follicles Menstrual Cycle: Luteal Phase FSH LH • Low LH causes degeneration of corpus luteum (day 22) • Followed by rapid drop in progesterone (& oestrogen) oestrogen • If NO fertilisation, Menstruation begins at Day 28 because the ovarian hormones (oestrogen + progesterone) are so low that the endometrium can’t be maintained Why do pregnant women not menstruate? The fertilised egg secretes a hormone called human chorionic gonadotrophin (HCG) which maintains the corpus luteum which secretes progesterone preventing menstruation. After 6 weeks the placenta secretes progesterone instead. Pregnancy tests, test for the presence of HCG in urine. Image source: staff.um.edu.mt Role of cervix The cells that line the cervix secrete mucus which lubricates the vagina. High levels of oestrogen stimulate these cells to secrete a watery mucus which help sperm enter the reproductive tract. to transport, nourish & filter sperm Endometrium (food lining) develops High levels of progesterone cause the cervical mucus to Prostaglandins in the thicken. During pregnancy semen also help transport this forms a semi-solid Endrometrium plug (+ some blood) is discharged the sperm by inducing to protect the fertilised muscular contractions in egg from infection. the uterus & oviduct. Image source: www.fertilityet.org.uk Body Temperature Body temperature rises by 0.5°C at ovulation and stays high during the luteal phase. Changes in viscosity of cervical mucus & body temperature are used by some people as indicators for the rhythm method of birth control. Image source: http://en.wikipedia.org Continuous v Cyclical Fertility Male fertility is continuous because they secrete a steady level of testosterone and produce a steady quantity of sperm. Female fertility is cyclical due to the delicate balance of gonadotrophic and ovarian hormones. Females are usually only fertile for 3-4 days immediately after ovulation.