* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinical Indications
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Environmental persistent pharmaceutical pollutant wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
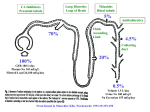
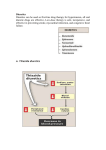
Diuretic Agents Carbonic Anhydrase Inhibitors Carbonic Anhydrase Inhibitors Carbonic anhydrase is in the PCT, where it catalyzes the dehydration of H2CO3 By blocking carbonic anhydrase, drugs block NaHCO3 reabsorption and cause diuresis Carbonic anhydrase inhibitors are now rarely used as diuretics They have several specific applications The prototypical drug is acetazolamide Carbonic Anhydrase Inhibitors the inhibition of enzyme causes HCO3– losses and metabolic acidosis the major clinical applications of acetazolamide involve sites other than the kidney. The ciliary body of the eye secretes HCO3– from the blood into the aqueous humor. formation of CSF by the choroid plexus also involves HCO3– secretion. Clinical Indications Glaucoma (dorzolamide, brinzolamide) Urinary Alkalinization Uric acid, cystine, and other weak acids are reabsorbed from acidic urine. renal excretion of cystine (in cystinuria) can be enhanced by increasing urinary pH. Metabolic Alkalosis + Edema Acute Mountain Sickness Toxicity Metabolic Acidosis Renal Stones Calcium salts are relatively insoluble at alkaline pH Renal Potassium Wasting Drowsiness and paresthesias after large doses Contraindications alkalinization of the urine decreases urinary excretion of NH4+ (converts it to rapidlyreabsorbed NH3) in patients with cirrhosis this contributes to hyperammonemia and hepatic encephalopathy. Loop diuretics Loop Diuretics Loop diuretics selectively inhibit NaCl reabsorption in the TAL Loop diuretics are the most efficacious diuretics because: large NaCl absorptive capacity of TAL The two prototypical drugs of this group are furosemide and ethacrynic acid. bumetanide and torsemide are also loop diuretics. The duration of effect for loop diuretics is short. Pharmacodynamics Loop diuretics inhibit the Na+/K+/2Cl– transporter in the TAL They reduce both the reabsorption of NaCl and lumen-positive potential that comes from K+ recycling. This positive potential normally drives divalent cation reabsorption in the loop So loop diuretics cause an increase in Mg2+ and Ca2+ excretion. Pharmacodynamics Prolonged use can cause significant hypomagnesemia intestinal absorption of Ca2+ can be increased and Ca2+ is actively reabsorbed in the DCT So loop diuretics do not generally cause hypocalcemia in disorders that cause hypercalcemia, Ca2+ excretion can be usefully enhanced by loop diuretics combined with saline infusions Both furosemide and ethacrynic acid have also been shown to reduce pulmonary congestion and LVEDP in heart failure before diuretic effect. Clinical Indications The major application of loop diuretics is in the treatment of edematous states heart failure, ascites, and acute pulmonary edema They are sometimes used in hypertension if response to thiazides is inadequate, but the short duration of action of loop diuretics is a disadvantage in this condition Clinical Indications A less common but important application is in the treatment of severe hypercalcemia Acute Renal Failure They increase urine flow and enhance K+ excretion. they can flush out pigment cast in the tubules. Toxicity Hypokalemic Metabolic Alkalosis They increase salt delivery to the collecting duct. This leads to increased secretion of K+ and H+ Ototoxicity dose-related hearing loss may happen and is usually reversible. It is most common in diminished renal function or those who are using other ototoxic drugs. Toxicity Hyperuricemia They may cause hyperuricemia and precipitate attacks of gout. This is caused by hypovolemia-associated enhancement of uric acid reabsorption in the PCT. Hypomagnesemia Occurs in dietary magnesium deficiency. It can be reversed by oral magnesium. Toxicity Allergic & Other Reactions Most of the loop diuretics are sulfonamides. skin rash, eosinophilia, and interstitial nephritis are occasional adverse effects. This usually resolves rapidly after drug withdrawal. Thiazides thiazides inhibit NaCl transport in the DCT. Thiazides All thiazides are secreted in the proximal tubule They compete with the secretion of uric acid So thiazides may elevate serum uric acid level. Thiazides block the Na+/Cl– transporter (NCC). thiazides actually enhance Ca2+ reabsorption. thiazides may rarely cause hypercalcemia They are useful for kidney stones caused by hypercalciuria. Thiazides Clinical Indications Hypertension heart failure nephrolithiasis due to idiopathic hypercalciuria Toxicity Hypokalemia, Metabolic Alkalosis and Hyperuricemia Hyperglycemia due to impaired release of insulin. Hyperlipidemia as a 5–15% increase in total serum cholesterol and LDL. Allergic Reactions (the thiazides are sulfonamides). Dilutional Hyponatremia is an important adverse effect of thiazides Potassium-Sparing Diuretics Potassium-Sparing Diuretics Spironolactone Eplerenone Amiloride Triamterene Potassium-Sparing Diuretics Potassium-Sparing Diuretics They antagonize the effects of aldosterone. Inhibition may occur by: direct antagonism of receptors (spironolactone, eplerenone) inhibition of Na+ influx (amiloride, triamterene). Eplerenone is more selective so has less side effects. They cause metabolic acidosis. Clinical Indications Compensation of thiazide-induced hypokalemia They are useful in primary and secondary hyperaldosteronism eplerenone has been found to reduce myocardial perfusion defects after MI. eplerenone reduced mortality rate by 15% (compared with placebo) in heart failure after MI. Toxicity They can cause life-threatening hyperkalemia. This risk is greatly increased by: renal disease the use of drugs that inhibit renin (β blockers) the use of drugs that inhibit angiotensin II activity (ACEIs, angiotensin receptor blockers (ARBs)). Combinations of K+-sparing and thiazides ameliorate thiazide-induced hypokalemia and alkalosis Toxicity Metabolic Acidosis Gynecomastia, impotence is reported with spironolactone but not with eplerenone. Patients with chronic renal insufficiency are especially vulnerable to hyperkalemia. Agents That Alter Water Excretion Osmotic Diuretics Antidiuretic Hormone (ADH) Agonists Antidiuretic Hormone (ADH) Antagonists Osmotic Diuretics Any osmotically active agent promotes a water diuresis. Such agents reduce intracranial and intraocular pressure The prototypic osmotic diuretic is mannitol. Oral mannitol causes osmotic diarrhea so for systemic effect, it is given parenterally. Osmotic Diuretics they also oppose the action of ADH. They reduce Na+ as well as water reabsorption. The natriuresis is of lesser magnitude than the water diuresis, leading to hypernatremia. Clinical indications It is used to prevent anuria from large pigment loads to the kidney. Reduction in ICP in neurologic conditions & IOP before ophthalmologic procedures. Toxicity Mannitol is rapidly distributed in the extracellular compartment and extracts water from cells. Prior to the diuresis, this leads to expansion of the extracellular volume and hyponatremia. This can complicate heart failure and may produce pulmonary edema. ADH Agonists & Antagonists ADH Agonists Vasopressin and desmopressin are used in the treatment of central diabetes insipidus. The renal action appears to be mediated primarily via V2 receptors They are ineffective in nephrogenic diabetes insipidus Treatment involves salt restriction, water restriction, thiazides and loop diuretics ADH Antagonists Syndrome of Inappropriate Antiduiretic Hormone (SIADH) secretion, causes water retention. Conivaptan is an antagonist against both V1a and V2 ADH receptors. Tolvaptan is an antagonist with more selectivity for V2 ADH receptors than V1a. Lithium & demeclocycline have anti-ADH effects, but have many side effects and are not used. Clinical Indications In SIADH when water restriction has failed. Toxicity Nephrogenic Diabetes Insipidus