* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Autacoids
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Serotonin syndrome wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
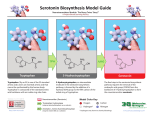
A UTACOIDS & T HEIR A NTAGONISTS , N ON -N ARCOTIC A NALGESIC A NTIPYRETICS & N ON - STEROIDAL A NTI -I NFLAMMATORY D RUGS I. INTRODUCTION Autacoids (auto-pharmacologic agents or local hormones) have widely differing structures & pharmacologic actions. An autacoid is a substance that is locally released & its action is limited to a specific site. The most extensively investigated autacoids are histamine & the prostaglandins. However, serotonin, bradykinin, & kallidin also function in a similar manner. Some autacoids (histamine & serotonin) function as neurotransmitters. II - HISTAMINE: Histamine is a bio-amine derived from dietary histidine (decarboxylated by l-histidine decarboxylase). Histamine has powerful pharmacologic actions, mediated by 2 specific receptor types: o H1-receptors mediate typical allergic & anaphylactic responses to histamine, (broncho-constriction, vasodilation, increased capillary permeability, & GIT spasms. o H2-receptors mediate other responses e.g. increased secretion of gastric acid, pepsin, & Castle's factor (intrinsic factor). ANTIHISTAMINICS: Antihistaminics can be classified as H1-receptor antagonists or H2-receptor antagonists. A- H1-receptor Antagonists: These are the classic antihistaminic agents. They competitively block H1-receptors, thus limiting the histamine's effects on bronchial smooth muscle, capillaries, & GI smooth muscle. These antagonists also prevent histamine-induced pain & itching of the skin & mucous membranes. Classification: H1-receptor antagonists have the general formula shown R R2 X – CH2 – CH2 – N R1 • R3 According to the “X” substituent, antihistaminics can be divided in 3 classes: Ethanolamines e.g. Diphenhydramine, dimenhydrinate, clemastine. X is CH Propylamines e.g. Chlorpheniramine, brompheniramine, acrivastine. X is Ethylenediamine e.g., pyrilamine, tripelennamine. – X is – – O N Three related classes, having the same formula as a part of a heterocyclic ring system are: – Phenothiazines e.g. promethazine (Phenergan). – Pipiperazines e.g., meclizine, cyclizine, hydroxyzine (Atarx), cetirizine (Zyrtec). – Piperidines e.g. terfenadine (Triludan), fexofenadine (Telfast), loratidine (Claritine), astemizole (Hismanal). 1 SAR of the antihistaminics: – A 3ry N is essential for activity (i.e. R2 & R3 = alkyl); 2ry amines are not active. – At R2 & R3 , methyl substitution most potent, as the chain length , the potency . – “ – CH2 – CH2 – ” gp. is essential for activity, and any slight modification in this gp. will the activity, with an only one exception in the phenothiazines (promethazine –Phenergan) with a branched ethyl [ – CH2 – CH (CH3) – ] gp. – R & R1 groups should be one of the following for maximum efficacy: – CH2 H2 Aryl Benzyl – CH2 H2 N N Hetero Benzyl Hetero Aryl • In case of ethanolamine & piperazine, maximum efficacy is when R & R1 are benzhydril. • In all of the above substitutions with an electron withdrawing group, in the para position will enhance the potency, e.g. chlorpheniramine is 20 times more potent than pheniramine. • Stereo chemistry: within the propylamine gp, (+) isomer is 4 times more potent than R (-) isomer. • The piperidines, acrivastine, & cetirizine comprise the 2nd-generation antihistaminics, which are less sedating than the older, 1st-generation drugs, due to their limited ability to cross the BBB. Uses: • Symptomatic relief of allergic symptoms, [seasonal rhinitis, conjunctivitis, & symptoms of rhinoviral infections (common cold)]. • Symptomatic relief of urticaria. • Agents with a high degree of anti-cholinergic activity (diphenhydramine, dimenhydrinate, meclizine, cyclizine) are sometimes used to treat nausea & vomiting associated with motion sickness & vertigo. • Promethazine is sometimes used as an anti-emetic. • Hydroxyzine is an anti-histaminic with an anti-anxiety effect. Adverse effects • CNS effects: e.g. CNS depression, sedation, fatigue, tinnitus, hallucinations, & ataxia • GI effects: e.g. nausea & vomiting • Antimuscarinic effects, e.g. dry mouth, urinary retention, & constipation • Teratogenic effects (possible with piperazine compounds) • Peripheral H1-receptor antagonists, terfenadine & astemizole, are devoid of significant sedative & antimuscarinic effects. However, elevated plasma levels of both astemizole & terfenadine have been associated with electrocardiographic cardiac arrest & ventricular arrhythmias. • Moreover, concomitant use of these agents with drugs or foods that inhibit their hepatic metabolism (ketonazole, macrolides, & grapefruit juice) is contraindicated because such a combination results in significantly elevated anti-histamine plasma levels. The incidence of arrhythmias was great enough to warrant the removal of terfenadine from the market. It has been replaced with its active metabolite fexofenadine. 2 B- H2-receptor Antagonists: • H2-receptor antagonists are heterocyclic congeners of histamine. These include: cimetidine (Tagamet), ranitidine (Zantac), famotidine, & nizatidine • These competitively block H2-receptors, thus limiting the effects of histamine on gastric secretions. • They are used to treat gastric hypersecretory conditions (duodenal ulcer). • They are effective in reducing pain associated with gastro-esophageal reflux disease (GERD), but they do not prevent actual reflux. Adverse effects: • CNS effects: e.g. confusion & dizziness. • Hepatic & renal dysfunction. • Inhibition of the hepatic microsomal drug-metabolizing enzyme system (with cimetidine). • Androgenic effects (with doses of cimetidine): e.g. impotence & gynecomastia in men & galactorrhea in women. C- The Proton Pump Inhibitors (Antisecretory Agents): • These are specific inhibitors of the proton pump H+, K+-ATPase, the ultimate mediator of gastric acid secretion. These include: Omeprazole (Losec) & Lansoprazole. • Structurally, these agents are substituted benzimidazoles linked to a pyridine ring by a sulfinyl bridge that is required for H+,K+-ATPase inhibition. • These agents are used to treat duodenal ulcers. Adverse effects • Diarrhea, GI pain, & headache. • May interfere with the metabolism of diazepam, warfarin, phenytoin, & theophylline. N.B. Exogenous histamine can be used as a diagnostic agent for testing gastric function. However, other stimulants of gastric secretion (pentagastrin) are more suitable & safer. 3 III- PROSTAGLANDINS In the body, prostaglandins (PGs) are principally synthesized from arachidonic acid, (from membrane phospholipids) by the enzyme cyclo-oxygenase (COX), which exists as 2 iso-zymes, COX I & COX II. • COX I functions constantly daily synthesis of PGs normal homeostasis, including protection of the gastric mucosa through PGs & hemostasis through the synthesis of thromboxane. • COX II is expressed only in response to inflammation or injury production of PGs for their role in the inflammatory response. The products of cyclo-oxygenase are then converted into either: PGs by PG synthase or Thromboxanes (TX) by thromboxane synthase. The only clinically relevant TX currently identified is TX A2, which causes platelet aggregation. Pharmacology PGs are released in response to many chemical, bacterial, mechanical, & other insults, & contribute to the signs & symptoms of the inflammatory process, including pain & edema. Physiologic responses to PGs include: • Vasodilatation in most vascular beds. • Inhibiting platelet aggregation. • Inhibition of gastric acid secretion. • Stimulation of gastric release of bicarbonate & mucus, protect gastric epithelium. • Relaxation of bronchial & GI smooth muscle. • Contraction of uterine smooth muscle. • Increase renal blood flow, promote diuresis & natriuresis, but paradoxically renin secretion. 4 NON-NARCOTIC ANALGESIC-ANTIPYRETICS & NSAIDS A. Salicylates • Salicylates are derivatives of salicylic acid, which is found as the glycoside salicin in willow bark. • Aspirin, (acetyl salicylic acid) hydrolyzes easily unstable in aqueous media / moisture. • More stable salicylates include diflunisal & methyl salicylate (wintergreen oil / topical). • Other salicylates: salsalate, Na thiosalicylate (injectable), choline salicylate (oral liquid), & the salicylate derivatives mesalamine, olsalazine, & sulphasalazine. • Most salicylates are weak acids their excretion is influenced by changes in urinary pH. • Salicylates inhibit cyclo-oxygenase inhibit local PG synthesis (esp. PG E2 which mediates inflammation) centrally analgesic for low-intensity pain, peripherally anti-inflammatory. • ASA acts on the subcortical sites of the CNS (hypothalamus). It inhibits PG synthesis in the thermoregulatory center of the hypothalamus antipyretic. • Aspirin is the only salicylate that irreversibly inhibits cyclo-oxygenase (by covalent acetylation). • Salicylates block platelet cyclo-oxygenase & subsequent formation of TX A2 inhibit platelet aggregation & thrombus formation. Therapeutic indications • Analgesic: 1g/day (musculoskeletal pain, headache, neuralgias, myalgias, spasmodic dysmenorrhea). • Anti-inflammatory: 3 – 6 g/day (various arthritis symptoms & acute rheumatic fever). • Antipyretic agents, for relief of fever. (Children with varicella or influenza-type viral infections should not be given salicylates because of the observed association between salicylate use in these situations and Reye's syndrome – fatty degeneration of liver with encephalopathy.) • Aspirin is indicated for prophylaxis of MI. • Methyl salicylate (wintergreen oil) is used topically as a counter irritant. • Low daily doses of salicylates (2 g), renal urate excretion & serum uric acid levels. High daily doses (5 g) have the opposite effect. • Sulphasalazine, olsalazine, & mesalamine are used to reduce the inflammation associated with inflammatory bowel disease & Crohn's disease. Adverse effects • Salicylism is salicylate toxicity that is usually marked by tinnitus, nausea, & vomiting. • GI effects, e.g. nausea, vomiting, & GI irritation, discomfort, ulceration, & haemorrhage. • Increased depth of respirations. • Excessive bleeding (inhibition of TX synthesis). • Uncoupling of oxidative phosphorylation, hyperglycemia, glycosuria, & reduced lipogenesis. • Delayed onset of labour. • Sulphasalazine has male reproductive effects, causing infertility. • Ingestion of one teaspoon of the topical agent methyl salicylate can cause fatal intoxication. 5 B. p-Aminophenol Derivatives • The prototypical p-aminophenol derivative is acetaminophen, an active metabolite of phenacetin. • p-Aminophenol derivatives inhibit central PG synthesis. • They are analgesic for low-intensity pain & are antipyretic. • Because they are less effective than salicylates in blocking peripheral PG synthesis, they have no anti-inflammatory activity & do not affect platelet function. Therapeutic indications • Acetaminophen & phenacetin are indicated for use as analgesics & antipyretics, particularly in the patient unable to tolerate salicylates. Patients allergic to A.S.A.: are advised to take paracetamol as antipyretic / analgesic or NSAIDs as analgesic / anti-inflammatory. • Acetaminophen may be safely used as an alternative antipyretic in the child with varicella or an influenza-type viral infection. Adverse effects: When given in therapeutic doses, adverse effects are limited to: Skin rash Hemolytic anemia (with long-term phenacetin use) Methemoglobinemia Renal dysfunction & tubular necrosis Acute acetaminophen overdose (10g) causes severe & fatal hepatotoxicity with necrosis & liver failure. (it is metabolized hepatically by conjugation to the glucoronide or SO4 metabolite). This can be treated by N-acetyl-cysteine (within 12 hrs). C. Pyrazolone Derivatives • The most important pyrazolone derivatives are phenylbutazone, its metabolite oxyphenbutazone, & the uricosuric agent sulfinpyrazone (Anturane). • They PG synthesis analgesic, antipyretic & anti-inflammatory effects. • Sulfinpyrazone inhibits proximal tubular absorption of urate & has a uricosuric effect. However, it is devoid of analgesic, antipyretic, or anti-inflammatory effects. Therapeutic indications • Phenylbutazone & oxyphenbutazone are used for short-term treatment of acute rheumatoid arthritic conditions & acute gout (should be given only after other therapeutic measures have failed). • Sulfinpyrazone is used to control hyperuricemia in the treatment of intermittent and chronic gout. Adverse effects: The adverse effects often limit their use and include: • GI effects: e.g. discomfort, nausea, vomiting, dyspepsia, & peptic ulceration. • CNS effects: e.g. drowsiness, agitation, confusion, headache, lethargy, numbness, weakness, tinnitus, & hearing loss. • Blood dyscrasias: e.g. agranulocytosis, thrombocytopenia, aplastic anemia, hemolytic anemia. • Cardiovascular effects: e.g. CHF with edema & dyspnea • Renal effects: e.g. nephrotic lithiasis, renal necrosis, impaired renal function, & renal failure • Hyperglycemia • Skin rash 6 D. Agents Used for Treatment of Gout • Acute attacks of gout result from elevates serum levels or urates deposition in joints an inflammatory response. Therapeutic agents counter this response by reducing plasma uric acid concentrations or inhibiting the inflammatory response. • Agents used for the treatment of gout have widely varying structures & include: Colchicine: • This is an alkaloid used in the treatment of acute attacks of gout. • Colchicine interferes with the inflammatory response of gout; it has anti-inflammatory effect. • Its mechanism of action is presumed to be related to its anti-mitotic activity. It inhibits tubulin synthesis, which is required for the movement of inflammatory cells. It appears to inhibit chemotaxis of leukocytes & other inflammatory cells in the affected joint inflammatory response to deposited urate crystals by inhibiting leukocyte migration & phagocytosis. It also interferes with kinin formation & reduces leukocyte lactic acid production. • Colchicine is used principally for the treatment of acute gout attacks (with NSAIDs). Allopurinol (Zyloric): • It reduces serum urate levels by blocking uric acid synthesis (competitively inhibits xanthine oxidase, which converts xanthine to uric acid). Also, it facilitates the dissolution of urate deposits. • It is used to prevent the development or progression of chronic gout. • Because it inhibits the xanthine oxidase enzyme, allopurinol may inhibit theophylline metabolism theophylline serum level toxicity. • Similarly if used with mercaptopurine we have to decrease its dose. Probenecid (Benecid): • It is a uricosuric agent, inhibits the proximal tubular reabsorption of uric acid, increasing uric acid excretion, thus reducing plasma uric acid concentrations. • It is used to treat chronic gout (also, in smaller doses to prolong the effectiveness of penicillin-type antibiotics by inhibiting their tubular secretion). Sulfinpyrazone (Anturan): • It has a uricosuric effect uric acid excretion by the kidney. It has no anti-inflammatory effect & is used in the treatment of chronic gout. Large doses of ASA have a uricosuric effect. Ticrynofen is a diuretic with a uricosuric effect. Gout attacks are treated with colchicine & any anti-inflammatory. Metabolism of A.S.A: is dose dependant, i.e. the the dose, the greater the metabolism. The pathway in the body is: A.S.A hydrolysis Salicylic acid converted to Salicyluric acid Genestic acid haemogestic acid (end product) glucoronide conjugation Phenolic glucorinate 7 E. NSAIDs 1. The Classic NSAIDs (Non-specific NSAIDs): • These consist of many structurally diverse acids. These include: o Propionic acid derivatives (fenoprofen, ibuprofen [brufen], ketoprofen [profenid], naproxen). o Acetic acid derivatives (diclofenac, indomethacin, ketorolac, sulindac [clinoril], & tolmetin). o Fenamates or anthranilic acid derivatives (meclofenamate & mefenamic acid [ponstan]). o Oxicams (piroxicam [feldene]). • These have anti-inflammatory effects (inhibit cyclo-oxygenase enzyme PG synthesis). • NSAIDs have analgesic / antipyretic effects & some have mild uricosuric activity. • NSAIDs, like aspirin, are agents of choice for the treatment of rheumatoid arthritis, osteoarthritis, & spondylitis. They may also be used as 2ry treatments in gouty arthritis. • Patients should not take aspirin during treatment with sulindac • NSAIDs are associated with these adverse effects: o GI effects: e.g. GI distress & irritation, erosion of gastric mucosa, nausea, vomiting, & dyspepsia o CNS effects: e.g. depression, drowsiness, headache, dizziness, visual disturbances, ototoxicity, & confusion o Hematologic effects: e.g. thrombocytopenia, altered platelet function, & prolonged bleeding time o Skin rash o Nephrotoxicity 2. Selective COX II inhibitors: • These are pyrazole derivatives & include: celecoxib (Celebrex) & rofecoxib (Vioxx). • These specifically inhibit PG synthesis associated with the inflammatory response. • Their ability to pain / inflammation in arthritic diseases is ~ equal to the non-selective NSAIDs. • By virtue of their selectivity, their actions on gastric mucosa & platelet aggregation are less than the non-selective NSAIDs. • They are approved for use in both rheumatoid arthritis & osteoarthritis. • They have incidence of adverse reactions vs. non-selective NSAIDs (lower incidence of GI upset, minimal GI ulceration). The potential for nephrotoxicity does exist & patients should be monitored. N.B. Dantrolone Sodium Injection (Dantrium): used to treat malignant hyperthermia. N.B. Zomeprac (Zomax): analgesic drug. It inhibits the cyclo-oxygenase enzyme in PG synthesis. N.B. Leukotriene antagonists e.g. zafirlukast (Accolate) & montelukast (Singulair) competitively inhibit leukotrienes at various receptor sites blocks effects of histamine, most notably bronchoconstriction & pulmonary edema associated with asthma & allergic reactions treatment of asthma. 8 Singulair 10 mg OD is used to control asthma. It interacts with refampicin & liver enzyme inducers (may be excreted in milk). Side effects include weakness, cough, headache, stomach pain, fever & earache. Accolate 20 mg BID prevents & treats chronic asthma. It is excreted in milk. Side effects are similar to Singulair. It interacts with terfenadine, astemazole, warfarin, aspirin & erythromycin. 9 IV- SEROTONIN Serotonin [5-hydroxytryptamine (5-HT)) is a bio-amine synthesized from the amino acid tryptophan. Serotonin exerts a wide range of effects via a family of receptors that includes at least 7 types & several subtypes. Major physiologic effects of serotonin include: • Vasoconstriction (5-HT 2), • Platelet aggregation (5-HT 2), • Increased release of acetylcholine in the enteric region (5-HT 4), • Nausea/emesis (5-HT 3), • Numerous behavioral actions that influence anxiety, depression, aggression, impulsivity, & appetite (5-HT1, 5-HT 2, 5-HT 3). Additionally, the 5-HT1D receptor acts as an autoreceptor to inhibit presynaptic activity at both serotonergic & adrenergic neurons in the CNS. Serotonin may also produce numerous other effects including the opposite of those stated above, depending on the specific receptor that mediates the event. SEROTONIN AGONISTS A- 5-HT 1D Receptor Agonists: (sumatriptan, rizatriptan, naratriptan, zolmetriptan) are indole derivatives structurally similar to serotonin. These mimic the actions of serotonin at this auto-receptor presynaptic neurotransmitter release release of serotonin &/or NE serotonin/NE-induced vasoconstriction of cerebral vessels cannot occur. B- Cisapride: is a benzamide that acts as a 5-HT 4 receptor agonist. It activates the serotonergic receptor (5-HT 4) release of acetylcholine. Although it has been removed from the market, structurally similar drugs may produce a similar effect. C- Ergot Alkaloids: (ergotamine) have some activity as a serotonin agonist/partial agonist. They produce a wide range of pharmacologic effects including both agonistic & antagonistic activity at adrenergic, dopaminergic, & serotonergic receptors. Therapeutic indications: • Numerous CNS active drugs utilize the serotonergic system to modulate behavior, e.g. the anorexiants (dexfenfluramine), anxiolytics (buspirone), & selective serotonin re-uptake inhibitors for depression (fluoxetine). These drugs act more on the neurotransmitter function of serotonin and will not be discussed here. • Some ergot alkaloids, sumatriptan & similar drugs, act to modulate the autacoid function of serotonin. They are used to prevent & treat migraine by altering serotonin's actions that result in changes in vascular tone. • Additionally, some ergot akaloids are used to prevent postpartum hemorrhaging (through both vasoconstrictive & uterine contractile actions) & to prevent postpartum breast engorgement (bromocriptine, through dopaminergic activity). • Cisapride was used in the treatment of GERD by increasing pyloric sphincter tone, which is mediated by acetylcholine release. 10 Adverse effects • 5-HT ID agonists may produce feelings of warmth, paresthesias, dizziness, & tightness or heaviness in the chest. Rarely, patients may experience chest pain. Since these agents may cause coronary vasoconstriction, they are contraindicated in angina patients & should be used cautiously in patients with hypertension or other risk factors for ischemic heart disease. • Cisapride may produce diarrhea as a side effect. Patients should be counseled to take cisapride with meals to increase its absorption. It also prolongs the QT interval causing life-threatening arrhythmias. This prompted its voluntary removal from the market in July, 2000. • Ergot alkaloids may cause GI upset & cold extremities. As toxicity progresses, the patient may experience emesis, diarrhea, peripheral pain 2ry to local ischemia, & hallucinations or delusions. SEROTONIN ANTAGONISTS A- Ergot alkaloids & derivatives with antagonist/partial agonist activity include ergonovine, dihydroergotamine, methysergide, & bromocriptine. B- 5-HT 3 antagonists may be either indole derivatives (ondansetron) or benzimidazoles (granisetron). Serotonin antagonists such as ondansetron and related drugs block the ion-channel coupled 5-HT 3 receptor, thus inhibiting the ability of serotonin to cause nausea and/or emesis. This action appears to occur both locally at the GIT & centrally in the area postrema. Therapeutic indications • Serotonin antagonists (ondasetron, granisetron, dolasetron) are used to prevent & treat nausea & emesis 2ry to antineoplastic therapy by blocking the actions of serotonin at the 5-HT 3 receptor. Adverse effects • The 5-HT 3 antagonists produce headache, constipation & dizziness. • Additionally, granisetron has been reported to produce somnolence & diarrhea. 1. Capsacine is: a. Pepper extract c. Used as analgesic (counter-irritant) b. Capsicum Extract d. Produces local heat 2. Cimetidine is: a. H2 antagonist. c. Used in peptic & duodenal ulcers b. Reduces gastric secretions 11