* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download What is the median eminence? The median eminence is the nucleus
Progesterone wikipedia , lookup
Sexually dimorphic nucleus wikipedia , lookup
Mammary gland wikipedia , lookup
Endocrine disruptor wikipedia , lookup
Women's Health Initiative wikipedia , lookup
Triclocarban wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Polycystic ovary syndrome wikipedia , lookup
Hormonal breast enhancement wikipedia , lookup
Hormone replacement therapy (female-to-male) wikipedia , lookup
Adrenal gland wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Xenoestrogen wikipedia , lookup
Hypothalamus wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Breast development wikipedia , lookup
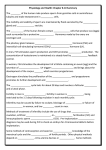
1. What is the median eminence? a. The median eminence is the nucleus at the base of the hypothalamus where releasing hormones enter the hypothalamo-hypophysial portal system in order to be transported to the pituitary gland. 2. What is the hypothalamo-hypophysial portal system? a. It is a specialized blood vessel system that transports releasing hormones from the median eminence through the infindibulum to the anterior pituitary 3. What structure produces releasing hormones? a. The hypothalamus 4. What are hormones that act “toward” a number of endocrine glands around the body controlling the production and release of hormones from these endocrine glands? a. Tropic hormones 5. What structure produces tropic hormones? a. The anterior pituitary 6. What is the target tissue of ACTH and what does it do? a. Target tissue: adrenal cortex, b. controls the production and release of the sex steroids (estrogens, androgens and progesterone), the glucocorticoids and the mineralocorticoids by the adrenal cortex 7. What is the target tissue of TSH and what does it do? a. Target tissue: thyroid gland, b. controls production and release of thyroid hormones which control metabolic rate 8. What is the target tissue of GH and what does it do? a. Target tissue: liver, musculature and skeleton b. affects growth rate 9. What is the target tissue of MSH and what does it do? a. Target tissue: melanocytes, b. affects skin pigmentation 10. What does BLPH do? a. precursor from which natural opiates like endorphins is produced 11. What are the two functions of FSH? a. stimulates the growth of the ovarian follicles b. Works with LH to stimulate ovulation 12. When is FSH most abundant in the menstrual cycle? a. At the beginning of the month b. Major surge at ovulation 13. What does FSH do in men? a. Stimulates the production of sperm 14. What are the four functions of LH? a. Stimulates estrogen production by the ovarian follicle b. Works with FSH to simulate ovulation c. Stimulates the formation of the corpus luteum d. Stimulates estrogen production by the corpus luteum 15. When is LH most abundant in the menstrual cycle? a. At ovulation, but generally pretty present all throughout cycle 16. What does LH do in men? a. Stimulates the production of testosterone 17. What are the two functions of Prolactin? a. Stimulates progesterone production by the corpus luteum b. Stimulates milk production by mammary glands 18. Can a woman have excessively high or excessively low prolactin levels and still be fertile? a. Probably not 19. What are the two hormones needed in breastfeeding and what are their functions? a. Oxytocin (produced by the paraventricular nucleus of the hypothalamus and released by the posterior pituitary) stimulates milk letdown b. Prolactin (produced in the anterior pituitary) stimulates the alveoli of the mammary glands to begin producing milk 20. When is progesterone most abundant in the menstrual cycle? a. During the postovulatory phase 21. How is the hypothalamus related to the anterior pituitary? a. The hypothalamus produces hormones called releasing hormones that control the production and release of the tropic hormones by the anterior pituitary 22. What are releasing hormones and what do they do? a. Releasing hormones are hormones produced in the hypothalamus which travel through the hypothalamo-hypophysial portal system to the anterior pituitary and stimulate and inhibit the production and release of the tropic hormones. 23. What are the seven releasing hormones (RH)? a. Corticotropic releasing hormone (CRH) b. Thyrotropic hormone releasing hormone (TRH) c. Somatostatin d. Growth hormone releasing hormone (GHRH) e. Gonadotropin hormone releasing hormone (GnRH) f. Dopamine g. Prolactin stimulating hormone (PSH) 24. What does CRH do? a. Stimulates the production and release of ACTH 25. What does TRH do? a. Stimulates the production and release of TSH 26. What does Somatostatin do? a. Inhibits the production and release of GH 27. What does GHRH do? a. Stimulates the production and release of GH 28. What does GnRH do? a. Stimulates the production and release of both FSH and LH 29. Where is inhibin produced and what does it do? a. Inhibin is produced by the ovarian follicle and the corpus luteum b. it acts at the anterior pituitary to inhibit the production and release of FSH 30. What does Dopamine do? a. inhibits the production and release of prolactin 31. What does PSH do? a. stimulates the production and release of prolactin 32. What RH releases two tropic hormones? a. GnRH releases both LH and FSH 33. What tropic hormones are affected by two RH? a. GH is stimulated by GHRH and inhibited by Somatostatin b. prolactin is stimulated by prolactin stimulating factor and inhibited by dopamine 34. In the adult female, how does very low estrogen affect GnRH? a. Stimulates the production of GnRH 35. In the adult female, how does moderate estrogen affect GnRH? a. Inhibits GnRH 36. In the adult female, how does very high estrogen affect GnRH? a. Stimulates GnRH 37. What type of feedback system regulates most of the hormonal systems in the body? a. Negative feedback 38. What is the feedback loop between FSH/LH and GnRH? a. Negative feedback: GnRH stimulates LH/FSH, increased levels of LH/FSH inhibit GnRH 39. When is the one time of the month when estrogen overrides the “negative feedback” system and makes it go to a “positive feedback” loop and why? a. Estrogen overrides the system 24 hours before ovulation when the Graafian follicle that is pushing against the ovary sends a signal that the ovum is ready for ovulation by dumping all of its remaining estrogen into the bloodstream. This very high level of estrogen stimulates GnRH release, which then stimulates production of both FSH and LH which is needed in order to trigger ovulation. The GnRH level in this case is so high that it overwhelms the effect of inhibin. So, massive release of E massive release of GnRH massive release of LH and FSH ovulation 40. List the Estrogen levels across the monthly cycle: a. Levels start to increase on Day 1 and gradually increase throughout the preovulatory phase (because the follicles are growing) b. Surge (sharp increase) 24 hours prior to ovulation. c. Levels decrease after surge (through ovulation). d. Levels rise during the postovulatory phase as the corpus luteum develops. e. Drop off just before menses when the corpus luteum dies. 41. List the Progesterone levels across the monthly cycle: a. Levels low on Day 1 b. Stay very low throughout the preovulatory phase c. Increase during the postovulatory phase with the development of the corpus luteum d. Drop off just before menses with the death of the corpus luteum 42. List the FSH levels across the monthly cycle: a. Begin to rise at the end of the postovulatory phase. b. Decrease in late preovulatory phase. c. Surge at the exact time of ovulation because of massive surge of estrogen by GnRH. d. Decrease after ovulation and stays low throughout most of the postovulatory phase 43. List the LH levels across the monthly cycle: a. Begin to increase on Day 1 to stimulate estrogen b. Rise to moderate level and stay relatively steady for the rest of the preovulatory phase c. Surge at ovulation. d. Declines right after ovulation to make CL e. Increases toward the end of the luteal phase and then declines again 44. What is the adrenal gland and where is it located in the body? a. The adrenal gland is a structure of two simultaneously present independent glands, the adrenal cortex and the adrenal medulla, and sits in the abdominal cavity right above the kidney 45. What is the adrenal medulla and what is its function? a. Gland (may or may not be an endocrine gland) at the inner core of the adrenal gland that produces adrenaline and noradrenalin in response to stress like being hungry, hot, scared, etc. 46. What is the adrenal cortex and what is its function? a. Endocrine gland at the outer cortex of the adrenal gland that produces and releases adrenocortical hormones in response to stimulation from the tropic hormone ACTH that is stimulated by the releasing hormone CRH. So, CRH ACTH adrenocortical hormones 47. What are the three classes of hormones that the adrenal cortex releases and what are their functions? a. Glucocorticoids controls glucose metabolism and food intake b. Mineralocorticoids regulate levels of minerals and electrolytes such as sodium or potassium c. Sex steroids (androgen, estrogen and progesterone) various actions on the body 48. Are steroid hormones fat soluble or water soluble? a. Fat soluble 49. What is the major source of androgen for women? a. The adrenal cortex 50. What is the best known and strongest androgen (most prevalent in men)? a. Testosterone 51. What is the most prevalent form of androgen in women? a. Androstenedione 52. How does androstenedione have a testosterone effect in women without having the overall masculinizing effect of testosterone? a. Once androstenedione enters into its target tissue it is converted to testosterone. This way, the testosterone acts only on the specific tissue it is meant for and does not masculinize the rest of the body on its way to the specific target tissue. 53. What are the three actions of androgen? a. Controls sex drive b. Controls acne c. Stimulates the growth of pubic and underarm hair 54. What is the precursor from which all sex steroids including progesterone, androstenedione, testosterone and estrogen are produced? a. Cholesterol 55. Are the sex steroid chemicals and their hormone precursors chemically very different or very similar from one another? a. Chemically very similar. This is why some synthetic hormones, like synthetic estrogen, can have progesterone-like or androgen-like activity in addition to their estrogen-like activity. 56. What is the difference between puberty and adolescence? a. Puberty refers to the biological maturation of an individual from being unable to reproduce to being able to reproduce while adolescence refers to the social transition in which an individual moves from a dependent, child like role to an independent, adult role. 57. What is the concern about the disparity between puberty and adolescence? a. The concern is that girls who reach biological maturity early will face pressures to engage in adult-like behaviors (dating, sex, smoking, drinking) before their decision-making and social skills have matured enough to deal with these issues. 58. What do Frisch and Tanner report about the age of menarche? a. The age of menarche has decreased over time 59. What do we know about the relationship between race/ethnity and the timing of puberty/menarche? a. Some studies show Latina or African-American girls going through puberty or menarche at earlier ages than Caucasian girls but these findings are controversial. Stresses related to minority status and/or socioeconomic conditions may account for the differences reported so far. 60. What are Tanner’s five stages of pubertal development? a. Start of the adolescent growth spurt b. Thelarche c. Simultaneous adrenarche and peak of the growth spurt d. Underarm hair formation e. Menarche 61. What hormone(s) are involved in the adolescent growth spurt? a. Estrogen, androgen and growth hormone 62. What is thelarche and what two things occur in this stage? a. Thelarche= the budding of the breasts i. Areola increases in size ii. Increased breast fat deposition 63. What hormone(s) are involved in thelarche? a. Estrogen and prolactin 64. What is adrenarche and what hormone(s) are involved? a. Adrenarche= increased hormone production by the adrenal cortex b. First sign is pubic hair formation - an androgen effect 65. What hormone(s) are involved in underarm hair formation? a. Androgen only 66. What is menarche? a. The first menses 67. What are factors have been found to correlate with early menarche? a. increased menstrual distress b. more worry about menstruation c. poorer preparation for menses d. increased risk of depression e. more negative body image and disordered eating f. increased risk of substance abuse g. higher risk for poor school performance h. increased social popularity i. earlier onset of dating and sexual behavior 68. Draw a picture of the relative hormone level changes that occur during puberty: a. Pre-puberty Post-puberty 69. What does this picture mean? (Explain it in words) a. Estrogen, LH and FSH hormone cycles begin before puberty, but they increase in amplitude during puberty 70. What does Frisch suggest about body fat and menarche? a. Body fat is a determinant of menarche (have to reach a certain percentage to begin menstruation) and that intense athletic training can inhibit puberty because it keeps body fat lower 71. Hormonally, how does body fat influence the onset of menarche? a. Because androgens are converted to estrogen in body fat tissue, the more body fat there is the more androgens are converted into estrogen. If estrogen levels get high enough to decrease the sensitivity of the hypothalamus then this estrogen level can stimulate the ovary to produce adult levels of estrogen and thus menarche 72. What is the word that means lack of menstruation? a. Amenorrhea 73. What is exercise-induced amenorrhea and what happens hormonally in this stage? a. Failure to menstruate as a result of intense athletic or dance training b. GnRH, LH and FSH and estrogen levels are suppressed so ovulation does not occur 74. Is exercise-induced amenorrhea reversible? How? a. Yes, ending strict athletic/ dance training can cause a return of cyclicity and menstruation 75. What are three causes of exercise-induce amenorrhea? a. Low body fat b. Change in the muscle: fat ratio (muscle > fat) as a result of an increase in muscle or decrease in fat c. Nutritional deficit state: energy output > energy input (can be caused as a result of increasing exercise without eating extra to compensate for the energy loss) 76. What are the risks associated with amenorrhea? a. Loss of bone density as a result of low estrogen which increases the risk of osteoporosis 77. What was the effect of societal stereotypes about premenstruum on scientific research on mood and the monthly cycle? a. Relaxed standards on scientific procedures in the study of mood or behavior and the monthly cycle which led to the publication of many studies that were poorly designed and yielded dubious results 78. In recall studies, what symptoms do women report to be associated with the menstrual cycle? a. An increase in negative moods and behaviors premenstrually b. And sometimes an increase in positive moods during the follicular phase or midcycle 79. In concurrent studies, what relationships between mood and behavior and the monthly cycle do women report? a. More positive moods and behaviors during the follicular phase or at midcycle. b. They report no correlation between negative moods and behaviors and the premenstrual phase of the cycle 80. Between recall and concurrent studies, which is a more accurate measure of mood and behaviors during the menstrual cycle? Why? a. Concurrent studies because by having women keep daily diaries of their moods, behaviors and cycle phases the responses are less tainted by stereotypes of moods/ behaviors 81. About how many women actually experience PMDD as defined by the DSM IV? a. 5-10% of the general population 82. Give some examples of physical, behavioral and mood symptoms of PMS: a. Physical: breast tenderness, bloating, headache b. Behavioral: sleep disturbances, poor concentration, and social withdrawal c. Mood: Irritability, mood swings, anxiety, depression 83. What is the difference between PMS and PMDD? a. PMS is a more laxly defined set of symptoms which can include physical as well as psychological symptoms. PMDD is more rigorously defined for research purposes. 84. PMDD can only be diagnosed as such if the person has at least one of four behavioral symptoms. What are they? a. Irritability b. Tension or anxiety c. Depressed mood or hopelessness d. Sudden mood swings 85. What are the four symptomatology requirements for PMDD? a. Symptoms must occur during most cycles for at least one year b. Symptoms must interfere with work, social activities and/or relationships c. Symptoms must be restricted to the perimenstrual time period (7 days before to 3 days after the onset of menses) d. Symptoms must be confirmed by daily diary for at least two cycles 86. Name some non-pharmacological and pharmacological interventions for PMDD a. Non-pharmacological: i. Awareness ii. Improved social support iii. Cognitive behavioral therapy iv. Increased aerobic exercise v. Changed diet: a. high carbs/ low protein, decreased caffeine and sodium, increased calcium intake b. Pharmacological: i. Selective Serotonin Reuptake Inhibitors ii. Antianxiolytics iii. Hormonal contraceptives and GnRH agonists that stop the cycle 87. What is menstrual synchrony and what is the cause? a. Menstrual synchrony is the tendency for women who live together’s cycles to become more synchronous (existing or occurring at the same time). It is apparently a response to pheromonal secretions (like those found in underarm perspiration). 88. Who first described menstrual synchrony and when? a. McClintock, 1971 89. Stern and McClintock (1998) found that women exposed to underarm secretions from women in their late follicular phase (post menses to the day before LH surge) resulted in what? a. Earlier LH surge (ovulation) and shortening of the cycle 90. Stern and McClintock (1998) found that women exposed to underarm secretions from women who had just ovulated resulted in what? a. Delayed LH surge and lengthened cycle in recipient 91. Do all cohabitating women become synchronous? a. No, factors leading to menstrual synchrony are not fully clear, but a greater number of shared activities may result in greater likelihood of synchrony 92. Did McClintock (1971) suggest that cycle length may be increased, decreased or become more regular when a woman has contact with males at least 3 times per week? a. Decreased 93. Did Burleson suggest that cycle length may be increased, decreased or become more regular with intercourse at least once a week? a. Cycle length becomes more regular 94. Extreme stress during the preovulatory phase results in what? a. Increased cycle length and delayed ovulation 95. Extreme stress during the postovulatory phase results in what? a. Decreased cycle length and earlier menses 96. What is the most commonly used form of contraception overall in the US? a. sterilization 97. What is the most commonly used form of contraception by women in the US who desire more children? a. hormonal contraceptives 98. What hormones are contained in hormonal contraceptives? a. estrogen & progestin or progestin only 99. What are the ways in which hormonal contraceptives are administered? a. pills, injections, implantable capsules, intrauterine devices (IUD), vaginal ring, and patch 100. What are the main action of estrogen in contraceptives? a. inhibits ovulation through inhibiting production of GnRH. 101. What are the five actions of progestin in contraceptives? a. prevents ovulation by inhibiting LH ad FSH production in the anterior pituitary b. stimulates the production of a thick, pasty cervical mucus. c. inhibits capacitation of sperm d. slows the rate of ovum transport through the oviduct e. prevents adequate build-up of the endometrium such that implantation is unlikely. 102. What is capacitation? a. An enzyme-initiated change in sperm that typically occurs inside the woman’s body and is required before fertilization can occur 103. If a contraceptive contains both estrogen and progestin, what is the net effect of the rate of ovum transport through the oviduct? a. the estrogen speeds transport but the progestin slows it down so the net result is no effect on the rate of transport 104. Which is more effective: a contraceptive containing only progestin or one containing both progestin and estrogen? a. both are extremely effective in the 98-100% range 105. What are the risks of estrogen in contraceptives? a. increased risk of blood clots, stroke, and heart attack; b. the effect on risk of breast cancer is unclear 106. What are the risks of progestin-containing contraceptives? a. increased risk of cardiovascular disease due to increase plasma lipids 107. What is Yasmin? a. a combination oral contraception that uses a different progestin that has an anti-androgenic and anti-mineralocorticoid effect 108. What is an additional risk associated with Yasmin? a. the new progestin used can result in elevated potassium levels, which can have adverse effects in someone who already has high potassium levels or who has kidney or liver problems b. recent research shows an increased risk of blood clots in women using Yasmin contraceptives 109. What are the advantages of hormonal contraceptives? a. may reduce the risk of ovarian cancer during and after use b. decreased risk of endometrial and colorectal cancer during use c. non-intrusive; it doesn’t interrupt sex d. easy to use e. highly effective f. reduction of menstrual blood loss g. reduced dysmenorrhea 110. What are the disadvantages of hormonal contraceptives? a. no protection from STDs b. may cause irregular menses or amenorrhea [particularly progestin-only contraceptives] c. reduced estrogen levels may reduce bone density 111. What forms of emergency contraception are available? a. Progestin only pills (Plan B and Next Choice), IUDs, and Ella 112. When must emergency contraception pills be taken in order to be effective? a. within 72-120 hours of unprotected sex depending on the pill 113. When must an IUD be inserted to be effective as an emergency contraceptive? a. within 5 days of unprotected sex 114. How does Plan B/NextChoice work? a. prevents ovulation b. slows the rate of ovum or sperm transport c. reduces endometrial buildup, making the endometrium unsuitable for implantation 115. If a fertilized ovum has already implanted, will Plan B/Next Choice work? a. no – they only works before implantation 116. How does Ella work? a. It contains a progesterone agonist/antagonist which blocks ovulation and inhibits progesterone actions at the uterus breaking down the endometrium 117. If a fertilized ovum has already implanted, will Ella work? a. Yes, it will destroy the uterine lining. It cannot be used if there is a positive pregnancy test 118. At what time in the cycle did Harvey find an increase in female autosexual behaviors? a. A clear peak at ovulation 119. What effect of the cycle did Harvey find on male partners of women? a. Partner initiated behavior follows the pattern of female autosexual behavior. They are more likely to initiate sex at ovulation, perhaps in response to chemical or behavioral signals from the woman. 120. What effect of the cycle did Matteo & Risman find on female partners of women? a. The pattern of partner initiated behavior did not follow that of female autosexual behavior. 121. Was the peak in female autosexual behaviors also seen in women on hormonal contraceptives? a. No, no such peak was found. 122. What was the difference for the peak in female autosexual behaviors between women using barrier method contraceptives and those using IUDs? a. Sex drive peak for women using IUDs was higher, perhaps due more confidence in effectiveness of contraceptive method. 123. What is the correlation between estrogen level and sex drive? a. No correlation. 124. What is the correlation between androgen level and sex drive? a. Positive correlation between a women’s average sex drive across an entire month and her average androgen level during that month .