* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Transcript
Epigenetics of human development wikipedia , lookup
Genetic engineering wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
History of genetic engineering wikipedia , lookup
Cancer epigenetics wikipedia , lookup
Frameshift mutation wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
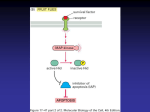
Therapeutic gene modulation wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Designer baby wikipedia , lookup
Genome (book) wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Microevolution wikipedia , lookup
Oncogenomics wikipedia , lookup
Pathology Neoplasia II, Molecular Neoplasia 09-23-08 Brian Bolerjack toomanyminutos 1: Continuation of last week, which was terminology and pictures. This time it’s molecular neoplasia, how these things come about. 2: The fundamental principles that you need to be familiar with. Tumors are monoclonal, resulting from accumulation of nonlethal genetic damage. A single cell undergoes some mutagenic event, has alteration of its genetic material, this is passed on to all offspring, and mutations accumulate. Targets of genetic damage include Protooncogenes (growth promoting), Tumor suppressor genes (growth inhibiting), Apoptosis regulating genes, Genes regulating repair. Carcinogenesis is a multistep process with an accumulation of mutations. 3: This is a cartoon from the book, and is of an isoform of an enzyme. The woman has two versions of the enzyme, an A form and a B form. This could be of any informative enzyme that you have two isoforms of. If we look at a neoplasm that arises, we would expect to see that all the cells in the neoplasm are either one isoform or the other. The whole tumor arises from a single cell. You wouldn’t expect to see a mixture of the isoforms. You don’t have polyclonal neoplasms. 4: This is a schematic of what we are going through today. We have acquired DNA damage that can be caused by many agents. These affect a normal cell, cause DNA damage. A repair mechanism may be initiated, but if it fails the mutation is passed on and they accumulate. With accumulation mutations you have progression of the tumor. So it’s a heterogeneous tumor even though it arises from one stem cell. It acquires new mutations so the cells are variable within a tumor. 5: How do tumors become malignant? It arises from self sufficiency in growth signals. Division of the cells is not under the normal regulatory controls of cell division. Cells are insensitive to growth inhibition. They can evade cell death, divide limitlessly (to an extent). They have to be able to sustain angiogenesis, or blood vessel production, to provide the tumor with the nutrients it needs. They have to have the ability to invade the basement membrane if it’s an epithelial tumor, to metastasize it must invade the blood vessel, travel to a distant point, evade the immune system, implant wherever it goes, and cause angiogenesis to provide nutrients. So it’s a complex system that has to happen for a tumor to metastasize. 6: Oncogenes. Oncogenes are the first genes we’ll talk about that drive neoplastic transformation. Protooncogenes, oncogenes’ normal counterpart, are genes which function to promote normal growth and differentiation. Their products drive the normal cell cycle. Oncogenes are derived from protooncogenes with activation and loss of normal regulatory control. And so transcription and production of oncoproteins is independent of growth factors or other external signals. 7: There are lots of different oncogenes, this looks at the families of oncogenes. You can have growth factors, growth factor receptors, signal transducing proteins, nuclear transcription activators, and cell cycle regulators. And we’ll look at examples of these. Oncogenes may be activated by overexpression, amplification, translocation, or point mutation. We will talk about examples of each of those so we can talk about how this actually works. Pathology Brian Bolerjack Neoplasia II, Molecular Neoplasia toomanyminutos 09-23-08 8: Some activation of oncogenes relies on a change in structure of the gene. This can happen through translocation or point mutation. There can be changes in regulation of gene expression, so you can have elevated levels of a normal protein. 9: This is a cartoon from the book looking at RAS, which is membrane bound in the MAP kinase pathway and is associated with a growth factor, and drives the cell cycle through activation of the MAP kinase pathway. Growth factor binds to growth factor receptor, which is membrane protein, and you have membrane bound RAS that is initially inactive binding GDP. With activation, GPD is released, GTP binds with RAS activating it. Activated RAS activates the MAP kinase pathway, kinase is a phosphorylation protein, and this activates transcription through the myc nuclear transcription factor. With mutations in RAS, which is by a point mutation that alters the proteins structure, we block the hydrolysis of GTP, so RAS stay in its activated form, continuing activation of the cell cycle unabaided. Point mutations, or direct mutation of the protein, is one mechanism of oncogenes. 10: Video of previous slide, skip. 11: Another way oncogenes can be activated is by translocation. It can cause an increased transcription of a normal gene product. This is Burkitt’s Lymphoma. We have a translocation from chromosome 8 to chromosome 14. The myc oncogene, a nuclear transcription factor, is next to the IgG gene, a very active area of transcription. You get increased myc production as a result. So increased transcription secondary to a translocation. 12: Translocation can also result in an altered protein. CML, where we have a translocation between chromosome 9 and 22. The abl oncogene, a tyrosine kinase, is translocated to the breakpoint cluster locus, and the two foci fuse to form a hybrid gene. It results in a tyrosine kinase that isn’t under normal regulatory control. We have an oncogene activated by a translocation, free from regulatory control. 13: Oncogenic activation by amplification. Don’t remember the tumor, it’s a neural tumor. You have amplification of myc just by increasing the number of copies of the gene. If you do a chromosomal prep you can see there is an elongated band, known as a homogeneous staining region. You have multiple copies of the gene within the chromosome, and you can also have transcriptionally active extrachromosomal genetic material known as double minutes, and with increased copy numbers you will have increased transcription of the gene. 14: Another gene that is clinically important is HER2/neu which is important in breast cancer. This is an example of amplification by increased copy numbers. With amplification of HER2/neu, patients did worse. Initially this was reported as a poor indicator of breast cancer. But more recently a drug that targets this membrane receptor has been developed and is called Receptin. We have a targeted therapy for the oncogene if the patient expresses the specific oncogene. We are entering an age where you can give specific drugs based on the antigenic expression of a tumor. 15: This is a membrane bound protein, so we can look at it through Ab staining, immunoperoxidase stain to see if there is overexpression. Overexpression of the membrane bound protein will highlight the cytoplasmic membrane. Pathology Brian Bolerjack Neoplasia II, Molecular Neoplasia toomanyminutos 09-23-08 16: You can also do direct probing by in situ hybridization to look at copy numbers. This is an example of FISH the dots on the left are in a non-amplified cell. You wouldn’t expect to see more than two copies of the gene. On the right there are multiple copies the HER2 gene. 17: Tumor suppressor genes, known as antioncogenes, cancer suppressor genes, inhibit the cell cycle. Important to remember: Knudsen’s two-hit hypothesis, which states that both alleles of the tumor suppressor gene must be mutated for loss of inhibitory function. If one allele is mutated you will have 50% of the product and that will usually be enough. You have to lose both alleles. The classic example is the Retinoblastoma protein. 18: This is a cartoon showing the normal function of the retinoblastoma protein. It serves as the gatekeeper of the cell cycle for progression from G1 to S. In its phosphorylated or activated form, the cell can progress from G1 to S and continue through the cell cycle. 19: This is a little more complex. The phosphorylation allows release of the E2 transcription factor, which allows transcription to occur. In its hypophosphorylated form E2F is bound and it blocks transcription. Anything that activates would be in the oncogene category and anything that inhibits would be in the tumor suppressor gene category. 20: Retinoblastoma is a rare ocular tumor of childhood. It is a prototype of cancer cause by loss of tumor suppressor genes. Most are sporadic, but 40% are familial born. 21: Gross (tan fleshy masses) and histological (small blue cell tumor) pictures. 22: In its sporadic form, all somatic cells have the normal retinoblastoma alleles. A mutation occurs in a single allele, and at that point there is normal function. But if there is another mutation in that cell or its offspring, you lose the inhibitory function of the gene, and you develop the tumor. In its familial form, there is already a single allele mutation. All the somatic cells have one mutated allele. If there is a single mutation in the other allele, then you will develop the tumor. 23: TP53 (p53) is the single most common target for genetic alteration in human tumors. In LiFraumeni Syndrome, individuals are born with one defective p53 gene. This makes them susceptible to many tumor types, mainly bone soft tissue sarcomas. P53 starts to apply the brakes on the cell cycle and allow DNA repair. 24: This is a cartoon from the book. In a normal cell you have DNA damage to some degree, and when this happens p53 is activated and binds to the DNA. It upregulates certain target genes, cyclin dependent kinase inhibitor, growth arrest and DNA damage 45 that is responsible for DNA repair, upregulation of p21 results in G1 arrest. This gene is involved in repair, if there is repair you have a normal cell. p53 also regulates the bax/bcl2 ratio. Bax drives apoptosis, and with failure of repair the cell undergoes apoptosis. This is with normal p53 function. You have an attempt at repair, with failure of repair you get apoptosis, so the damage can’t be passed to offspring. With a mutated p53, we can’t put the brakes on the cell cycle, you have less repair, and you get mutations passed on to future cells, so you have neoplastic transformation. 25: Apoptosis is controlled cell death, important in embryogenesis and passing on mutations. Bcl-2 prevents apoptosis, bax promotes apoptosis. The regulation of the two is under p53. Pathology Neoplasia II, Molecular Neoplasia 09-23-08 26: Brian Bolerjack toomanyminutos When the ration of bax to bcl2 is high, apoptosis occurs. 27: The layering gets complex. You have cyclin dependent kinase feeding into retinoblastoma and its formation. You also have cyclin kinase inhibitors that regulate the cyclin dependent kinases. You don’t need to know all the details. 28: Central ideas. Carcinogenesis is a multistep process requiring accumulation of multiple genetic alterations. Molecular targets for carcinogenesis include protooncogenes, tumor suppressor genes, genes regulating apoptosis, and genes involved in DNA repair. As a rule, cancers exhibit multiple genetic alterations involving activation of several oncogenes and loss of two or more tumor suppressor genes. 29-30: A few more concepts in neoplasia we need to understand. 31: Early in neoplastic transformation, we have a single cell that divides, so with each generation you have a doubling of the tumor size. As the tumor grows, a number of cells drop into the nonproliferative pool. Some will acquire lethal mutations, some will outrun their blood supply and necrose. Some become senescent and drop out, could be nutritional. Some will undergo more mutation and differentiation. Initially all the cells are growing and dividing. As the tumor grows, the majority of tumors are not actively dividing. That’s important because most chemo therapy is only effective against growing, dividing cells. So most cells of a mature tumor will not be affected. Things are done to drive a larger percentage of cells into the proliferative pool. Surgical debulking, you take away a lot of the mass and more cells will move into the proliferative pool, and radiation debulks the tumor to drive the cells into the proliferative phase. You kill off a large number and drive the remainder into the proliferative pool so the therapy is more effective. 32: Tumor progression. Subclones are generated from the original malignant cells. The most fit survive and predominate in the tumor. The rate at which subclones with additional phenotypes develop is variable. 33: A normal cell undergoes neoplastic transformation, becomes a malignant cell. This tumor requires fewer growth factors, which would be a survival advantage. So the tumor begins to grow faster without requiring as many nutrients. Some will undergo nonviable mutation so there are no offspring produced. Additional features may be acquired, the ability to evade the immune system, invade. We have a heterogeneous tumor with an accumulation of mutations, which will provide some advantage which will allow it to metastasize. 34: This is very complex, and you think how could it ever happen. The tumor is able to invade through the basement membrane and blood vessel, it evades the immune system, travels to another site, extravasates through the blood vessel, sets up, and induces angiogenesis so it has a blood supply. The lesson is that mutations occurring all the time. Some of the early mutations in neoplastic transformation sets you up to be able to have more mutations. Once you have a p53 mutation, you are more likely to pass on mutations because you no longer have the ability to regulate when cells should apoptose. Pathology Brian Bolerjack Neoplasia II, Molecular Neoplasia toomanyminutos 09-23-08 35: Why do we get mutations? Carcinogens! There are chemical agents, direct (directly affect the DNA) or indirect (must undergo some metabolic transformation before they are carcinogenic) acting. They can be inhaled toxins like in cigarette smoke, things we put in our bellies or things we put on our skin. The ras gene is commonly affected by chemical carcinogens (dietary). 36: There are viral carcinogens. We have RNA viruses, HTLV-1 which is associated with leukemia. Hepatitis C virus is associated with hepatocellular carcinoma. DNA viruses, human papillomavirus is associated with cervical cancer, certain oropharyngeal squamous cell carcinomas, particularly tonsilar carcinomas. Epstein-Barr virus with nasopharyngeal carcinomas. Hep B virus with hepatocellular carcinoma. 37: Radiation can be a carcinogen by causing cross linking of DNA. UV from sunlight is associated with skin cancer: squamous cell carcinoma, melanomas, basal cell carcinomas are associated with sun exposure. Ionizing and nuclear radiation increased rates of leukemia and tumors in Hiroshima and Nagasaki. Chernobyl children have increased rates of papillary thyroid carcinoma. There is a long latent period because there must be an accumulation of molecular events in order to get neoplastic transformation. 38: Colorectal carcinoma serves as a model to explore the progression of tumors. It has well defined clinical progression and correlating histology. First, you have normal mucosal surface and crypt epithelium. You uniform crypts lined by goblet cells with mucus toward the lumen of the crypt and nuclei basally oriented. The earliest histological sign you can see is aberrant crypt foci (histologic, no clinical correlation). We see these in patients with other lesions. You see decreased mucus production and stratification of nuclei. They are starting to go to different levels throughout the cell. Then we develop an adenomatous polyp, a clinical lesion that can be seen. A polyp is a raised lesion from an epithelial surface. It can be attached broad (sessile) or it can be pedunculated on a stalk. This is the earliest clinical sign and this is why older people have colonoscopies. You can determine risk of cancer and small polyps can be removed at the time of colonoscopy. Then you have invasive carcinoma and can develop the ability to metastasize. 39: What do you see here? This is longitudinally opened colon. There is a little lesion on a stalk with a dark brown cap. It is an adenomatous polyp. A pedunculated polyp in the colon. 40: You can see two polyps here. Normal colonic epithelium. 41: Histologically, you see normal epithelium, and it is fairly clear there because of abundant mucus content. If you look in the cap of the stalk of the polyp it become much darker because you have decreased mucin production and you have the nuclei moving throughout the cells. 42: High magnification, nuclei are sitting toward the lumen, and should not be there. So these are the characteristics of an adenoma. 43: This is a large lesion in the colon, maybe 3cm. Can’t tell if it is malignant or not grossly. It could be a large sessily adenoma, or an adenocarcinoma. Must look histologically. 44: Another large lesion with central ulceration, so it is almost certainly an invasive adenocarcinoma. Pathology Neoplasia II, Molecular Neoplasia 09-23-08 Brian Bolerjack toomanyminutos 45: Here is a cross section of a carcinoma and you can see invasion through the muscularis propria out into the soft tissues, probably have lymph node metastasis. 46: Histologically you would see this. You know it’s an adenocarcinoma, a malignant neoplasm of epithelial tissue of glandular origin, because you see glandular differentiation. It’s infiltrating. And there is a bit of atypia, decreased mucin production and distributed nuclei. 47: We can look at molecular events at genes at each step and see how they are affected. We have talked about ras and that it undergoes activating point mutations. 48: If we look at colorectal carcinomas, it seems to drive progression. Specific point mutations are identified in 50% of colorectal adenomas larger than 1 cm. ras mutations are rarely observed in smaller adenomas. These findings suggest that ras mutations are involved in adenoma progression. 49: We will start a scheme with all the steps we looked at, from normal colonic epithelium to metastatic carcinoma, and we have ras mutation between early and intermediate adenoma. 50: p53 and its role as a tumor suppressor gene. Tumor suppressor gene on chromosome 17p13.1 Among the most common targets for genetic mutation in human cancers (Li-Fraumeni syndrome). p53 normally functions to inhibit cell cycle activity in response to DNA damage and to regulate apoptosis (bax/bcl-2). 51: 17p losses and mutations are observed in 75% of invasive colorectal carcinomas. These changes at the p53 locus are rarely observed in adenomas. Inactivation of p53 appears to be a late event in the development of colorectal carcinoma. 52: So this is between the progression for a late adenoma to a carcinoma, so the ability to invade. 53: Deleted in Colon Cancer gene is located on 18q. The protein product of this gene acts as a cell surface adhesion/receptor molecule. Loss of DCC expression is seen in over 70% of colorectal carcinomas and half of large adenomas suggesting role as a tumor suppressor gene. Loss is rarely seen in small adenomas. 54: There are other genes in this area, but there is something in 18q21 that is acting as a tumor suppressor gene so deletions are common. 55: We can put that in progresson of adenomas. 56: The APC (adenomatous polyposis coli) gene is located on chromosome 5q. Inherited genetic mutation is associated with the familial polyposis coli syndrome. In this disease at childhood there will be thousands of polyps that carpet the colon, and maybe the small intestine. There is 100% leading to carcinoma if not treated. It is treated by total colectomy. The APC protein is a transcription regulator through interactions with beta-catenin. 57: This is an example. There is no normal colonic mucosa here. It is all adenomatous polyps. Pathology Brian Bolerjack Neoplasia II, Molecular Neoplasia toomanyminutos 09-23-08 58: We find APC gene mutation in over 80% of sporadic colorectal adenocarcinomas. The mutation rate in adenomas is similar to that in carcinomas. Mutations of the APC gene have been identified in the earliest histologically defined lesions (ACF). These findings suggest that APC mutation is an early, perhaps initiating event in colorectal carcinoma. 59: So we can add that in the transition from normal colonic epithelium to the aberrant crypt foci. 60: There are many other genes that can be implicated. We continue to acquire mutations that lead to progression of the tumor. Sporadic cases of myc, myb, NEU, and cyclin amplification have been identified in colorectal carcinoma. These oncogenes probably contribute to tumor progression, particularly at late stages. Tumors are monoclonal but genetically heterogeneous. 61: Those are added into the schematic there. 62: We have loss of DNA methylation of posttranscriptional modification, which appears to be early in adenoma formation. 63: We are left with this cartoon from the book that is a little simplified. We have normal colonic epithelium, homozygous loss of the APC locus on 5q (the cells don’t look normal, this happens in aberrant crypt foci). This is a tumor suppressor gene so you must lose both alleles. You have a mutation on ras of 12p that leads to formation adenomas. Homozygous loss of dcc or something on 18q, another tumor suppressor gene leads to increase in adenoma size. Other mutations, loss of p53, leads to invasive carcinoma and metastasis. Does it have to happen in this order? No. There’s no way to predict it. This is a general scheme based on statistics. You could start with the p53 mutation and it go from there. Tumors are monoclonal but heterogeneous. Tumor progression is from accumulation of mutations that allows invasion of blood vessels, metastasis, and angiogenesis.