* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Saladin 5e Extended Outline
Intracranial pressure wikipedia , lookup
Cardiac output wikipedia , lookup
Hemodynamics wikipedia , lookup
Homeostasis wikipedia , lookup
Freediving blackout wikipedia , lookup
High-altitude adaptation in humans wikipedia , lookup
Pre-Bötzinger complex wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Physiology of decompression wikipedia , lookup
Circulatory system wikipedia , lookup
Haemodynamic response wikipedia , lookup
Alveolar macrophage wikipedia , lookup
Organisms at high altitude wikipedia , lookup
Acute respiratory distress syndrome wikipedia , lookup
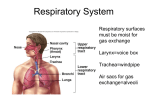
Saladin 5e Extended Outline Chapter 22 The Respiratory System I. Anatomy of the Respiratory System (pp. 864–875) A. Respiration has three meanings: (1) ventilation of the lungs (breathing), (2) exchange of gases between air and blood and between blood and tissue fluid, and (3) the use of oxygen in cellular metabolism. (p. 864) B. The respiratory system is an organ system that rhythmically takes in air and expels it from the body, supplying the body with oxygen and expelling carbon dioxide; however, it has many other functions. (p. 864) 1. It provides for oxygen and carbon dioxide exchange between blood and air. 2. It serves for speech and other vocalizations. 3. It provides the sense of smell. 4. By eliminating CO2, it helps control the pH of body fluids, which otherwise might become too acidic (acidosis). 5. The lungs carry out a step in synthesis of angiotensin II, which helps regulate blood pressure. 6. Breathing promotes the flow of lymph and venous blood between abdomen and thorax. 7. Breath-holding help expel abdominal contents during urination, defecation, and childbirth. C. The principal organs of the respiratory system are the nose, pharynx, larynx, trachea, bronchi, and lungs. (p. 864) (Fig. 22.1) 1. The air flows along a dead-end pathway in the lungs, stopping in the alveoli and then flowing back out along the same path. 2. The conducting division consists of passages that serve only for airflow, essentially from nostrils through the major bronchioles. 3. The respiratory division consists of the alveoli and other distal gas-exchange regions. 4. The airway from the nose through the larynx is often called the upper respiratory tract, and the regions from the trachea through the lungs compose the lower respiratory tract. D. The nose has several functions, including warming, cleansing, and humidifying inhaled air; detecting odors; and serving as a resonating chamber for the voice. (pp. 864–867) 1. It extends from the nostrils (nares) to a pair of posterior openings, the posterior nasal apertures, or choanae. 2. The facial part of the nose is shaped by bone and hyaline cartilage. Saladin Outline Ch.22 Page 2 a. Its superior half is supported by a pair of small nasal bones medially and the by maxillae laterally. b. The inferior half is supported by the lateral and alar cartilages. (Fig. 22.2) c. The flared portion at the lower end, called the ala nasi, is shaped by the alar cartilages and dense connective tissue. 3. The internal chamber, or nasal cavity, is divided into right and left halves, the nasal fossae. a. The dividing wall is a vertical plate, the nasal septum, of bone and hyaline cartilage. i. The vomer forms the inferior part of the septum. ii. The ethmoid forms its superior part. iii. The septal cartilage forms its anterior part. (Fig. 22.3c) b. The ethmoid and sphenoid bones form the roof of the nasal cavity, and the hard palate forms its floor. i. The palate separates the nasal cavity from the oral cavity, allowing one to breathe while chewing food. c. The paranasal sinuses and nasolacrimal ducts of the orbits drain into the nasal cavity. 4. The nasal cavity begins with a small chamber called the vestibule just inside the nostril and bordered by the ala nasi. a. The vestibule is lined with stratified squamous epithelium and has stiff guard hairs (vibrissae) that block debris from entering the nose. 5. Posterior to the vestibule, the nasal cavity expands into a much larger chamber that does not have much open space. a. It is occupied by three folds of tissue, the superior, middle, and inferior nasal conchae, or turbinates, that project from the lateral walls. (Fig. 22.3) b. Beneath each concha is a narrow air passage called a meatus. c. The narrowness of these passages and trubulence ensure that most air contact the mucous membrane on its way through to cleanse, warm, and humidify it. 6. Odors are detected by sensory cells in the olfactory epithelium on the roof of the nasal fossa and adjacent parts of the septum and superior concha. 7. The rest of the nasal cavity except for the vestibule is lined with respiratory epithelium. a. Both are ciliated pseudostratified columnar epithelia, but cilia in olfactory epithelium are immobile. b. The respiratory epithelium is similar to that shown in Figure 5.7 and has wineglass-shaped goblet cells that secrete mucus; its mobile cilia propel the mucus posteriorly. Saladin Outline Ch.22 Page 3 c. The nasal mucosa also contains mucous glands, located in the lamina propria that supplement mucus produced by goblet cells. d. Inhaled foreign matter sticks to the mucus and is swallowed. e. The lamina propria is well populated by lymphocytes and plasma cells and contains large blood vessels to help warm the air. 8. The inferior concha has an extensive venous plexus called the erectile tissue (swell body). a. Every 30 to 60 minutes, the erectile tissue on one side swells with blood and restricts airflow through that fossa, and air is directed through the other nostril. b. The engorged side then has time to recover from drying effects. E. The pharynx is a muscular funnel extending about 13 cm (5 in.) from the choanae to the larynx; it has three regions. (p. 867) 1. The nasopharynx lies posterior to the choanae and above the soft palate. a. It receives the auditory (eustachian) tubes from the middle ears and houses the pharyngeal tonsil. b. Inhaled air turns 90° downward as it passes through the nasopharynx. c. Particles larger than 10 μm generally cannot make the turn and become stuck to mucosa near the tonsil. 2. The otopharynx is a space between the inferior margin of the soft palate and the epiglottis; it contains the palatine tonsils. 3. The laryngopharynx lies mostly posterior to the larynx, extending from the superior margin of the epiglottis to the inferior margin of the cricoid cartilage, where the esophagus begins. a. The otopharynx and laryngopharynx, unlike the nasopharynx, pass air, food, and fluids and are lined by stratified squamous epithelium. F. The larynx, or voice box, is a cartilaginous chamber about 4 cm (1.5 in.) long. (pp. 867–869) (Fig. 22.4) 1. Its primary function is to keep food and drink out of the airway, but it evolved the additional role of sound production in many animals. 2. The superior opening of the larynx is guarded by a flap of tissue called the epiglottis. a. At rest, the epiglottis stands almost vertically. b. During swallowing, extrinsic muscles of the larynx pull the larynx upward toward the epiglottis, the tongue pushes the epiglottis downward to meet it, and the epiglottis closes the airway, directing food and fluid into the esophagus. c. The vestibular folds of the larynx play a greater role in keeping food and drink out of the airway. Saladin Outline Ch.22 Page 4 3. In infants the larynx is high in the throat, and the airway is more or less continuous from the nasal cavity to the larynx, allowing the infant to breathe continually while swallowing. 4. The framework of the larynx consists of nine cartilages. a. The first three are solitary and relatively large. i. The epiglottic cartilage, the most superior, is a spoon-shaped supportive plate in the epiglottis. ii. The largest, the thyroid cartilage, is names for its shieldlike shape; it covers the anterior and lateral aspects and forms the “Adam’s apple” peak in males. iii. The ringlike cricoid cartilage, located inferiorly, connects the larynx to the trachea; thyroid and cricoid cartilages constitute the box of the voice box. b. The remaining cartilages are smaller and occur in three pairs. i. Posterior to the thyroid cartilage are the two arytenoid cartilages. ii. Attached to the arytenoid cartilages’ upper ends is a pair of little horns, the corniculate cartilages; the arytenoid and corniculate cartilages function in speech. iii. A pair of cuneiform cartilages supports the soft tissues between the arytenoids and the epiglottis. 5. A group of fibrous ligaments binds the cartilages of the larynx together and to adjacent structures of the neck. a. Superiorly, a broad sheet called the thyrohyoid ligament joins the thyroid cartilage to the hyoid bone. b. Inferiorly, the cricotracheal ligament joins the cricoid cartilage to the trachea. c. Collectively the above ligaments are called the extrinsic ligaments because they link the larynx with other organs. d. The intrinsic ligaments are contained entirely within the larynx and link its nine cartilages to each other. e. Two pairs of intrinsic ligaments, the vestibular and vocal ligaments, extend from the thyroid cartilage anteriorly to the arytenoid cartilages posteriorly and support the vestibular folds and vocal cords. 6. The larynx has muscular walls. a. The deep intrinsic muscles operate the vocal cords, and the superficial extrinsic muscles connect the larynx to the hyoid bone and elevate the larynx during swallowing. b. The extrinsic muscles are also called the infrahyoid group. Saladin Outline Ch.22 Page 5 7. The interior wall of the larynx has two folds on each side that stretch from the thyroid cartilage in front to the arytenoid cartilages in back.. a. The superior vestibular folds play no role in speech but close the larynx during swallowing; they are supported by vestibular ligaments. (Fig. 22.4c) b. The inferior vocal cords (vocal folds) produce sound when air passes between them. i. The vocal cords and the opening between them are collectively called the glottis. (Fig. 22.5a) ii. The intrinsic muscles control the vocal cords by pulling on the corniculate and arytenoid cartilages, causing the cartilages to pivot. iii. Depending on their direction of rotation, the arytenoid cartilages abduct or adduct the vocal cords. (Fig. 22.6) iv. Air forced between the adducted vocal cords vibrates them, producing sound. v. In adult males, the vocal cords are usually longer and thicker, vibrate more slowly, and produce lower-pitched sounds than in females. vi. Loudness is determined by the force of the air passing through the cords. vii. The crude sounds from the larynx are formed into words by actions of the pharynx, oral cavity, tongue, and lips. G. The trachea, or “windpipe,” is a rigid tube about 12 cm (4.5 in.) long and 2.5 cm (1 in.) in diameter, anterior to the esophagus. (pp. 869–871) (Fig. 22.7a) 1. The trachea is supported by 16 to 20 C-shaped rings of hyaline cartilage. 2. The open part of the C faces posteriorly, where it is spanned by a smooth muscle, the trachealis. (Fig. 22.7c) 3. The gap in the C allows room for the esophagus to expand as swallowed food passes by; the trachealis muscles contract or relax to adjust airflow. 4. The inner lining of the trachea is a pseudostratified columnar epithelium composed mainly of mucus-secreting goblet cells, ciliated cells, and short basal stem cells. (Figs. 22.7b and 22.8) a. The mucus traps inhaled particles, and the upward beating of the cilia moves mucus toward the pharynx, where it is swallowed. b. This mechanism is called the mucociliary escalator. 5. The connective tissue beneath the tracheal epithelium contains lymphatic nodules, mucous and serous glands, and the tracheal cartilages. a. The outermost layer, the adventitia, is fibrous connective tissue that blends into that of other organs of the mediastinum. Saladin Outline Ch.22 Page 6 6. At the level of the sternal angle, the trachea forks into the right and left main bronchi. a. the lowermost tracheal cartilage has in internal median ridge called the carina that directs airflow right and left. (Fig. 22.5b) b. The bronchi subdivide in the lungs to form the bronchial tree Insight 22.1 Tracheostomy H. The lungs are somewhat conical with a broad concave base resting on the diaphragm and a blunt peak called the apex projecting slightly above the clavicle. (Fig. 22.9) 1. The costal surface is pressed against the rib case, and the smaller mediastinal surface faces medially. 2. The mediastinal surface exhibits a slit, the hilum, through which the lung receives the main bronchus, blood vessels, lymphatics, and nerves; these structures are termed the root of the lung. 3. The lungs are crowded by adjacent organs and do not fill the entire rib cage; they are also not symmetrical. (Fig. 22.10) a. Much of the space within the rib cage is occupies by the liver, spleen, and stomach inferior to the lungs and diaphragm. (Fig A.14) b. The right lung is shorter than the left because the liver rises higher on the right. c. The left lung, although taller, is narrower than the right because the heart tilts toward the left. d. On the medial surface, the left lung has an indentation called the cardiac impression. e. The right lung has three lobes—superior, middle, and inferior. i. A deep groove called the horizontal fissure separates the superior and middle lobes. ii. A similar oblique fissure separates the middle and inferior lobes. f. The left lung has only a superior and inferior lobe and single oblique fissure. 4. The bronchial tree is a branching system of air tubes within each lung; it extends from the main bronchus to about 65,000 terminal bronchioles. a. Arising from the fork in the trachea, the right main (primary) bronchus is about 2 to 3 cm long. i. It is slightly wider and more vertical than the left one, and so objects aspirated lodge here more often than in the left. ii. It gives off three branches: the superior, middle, and inferior lobar (secondary) bronchi, one to each lobe. b. The left main bronchus is about 5 cm long and slightly narrower. i. It gives off superior and inferior lobar bronchi to the two lobes. Saladin Outline Ch.22 Page 7 c. In both lungs, the lobar bronchi branch into segmental (tertiary) bronchi. i. There are 10 in the right lung and 8 in the left. ii. Each one ventilates a functionally independent unit called a bronchopulmonary segment. d. The main bronchi are supported, like the trachea, with C-shaped rings of hyaline cartilage, whereas the lobar and segmental bronchi are supported by overlapping crescent-shaped cartilaginous plates. e. All of the bronchi are lined with ciliated pseudostratified columnar epithelium. f. The lamina propria has an abundance of mucous glands and lymphocyte nodules (bronchus-associated lymphatic tissue, BALT). g. All divisions of the bronchial tree contain elastic connective tissue that provides recoil to expel air. h. The mucosa has a well developed layer of smooth muscle, the muscularis mucosae, which contracts or relaxes to constrict or dilate the airway. i. Branches of the pulmonary artery closely follow the bronchial tree on their way to the alveoli. i. The bronchial tree is services by the bronchial artery, which arises from the aorta and carries systemic blood. j. Bronchioles are continuations of the airway that lack supportive cartilage and are 1 mm or less in diameter. i. The portion of the lung ventilated by one bronchiole is called a pulmonary lobule. ii. Brionchioles have a ciliated cuboidal epithelium and a welldeveloped layer of smooth muscle in their walls. k. Each bronchiole divides into 50 to 80 terminal bronchioles, the final branches of the conducting division. i. These measure 0.5 mm or less and have no mucous glands or goblet cells; they do have cilia. l. Each terminal bronchiole gives off two or more smaller respiratory bronchioles that have alveoli budding from their walls; these are considered the beginning of the respiratory division. i. Their walls have scant smooth muscle, and the smallest are nonciliated. ii. Each divides into 2 to 10 elongated, thin-walled passages called alveolar ducts, which also have alveoli along their walls. (Fig. 22.11) Saladin Outline Ch.22 Page 8 iii. The ducts end in alveolar sacs, grapelike clusters of alveoli clustered around a space called the atrium. 5. The path of airflow in the conducting division is as follows: nasal cavity pharynx trachea main bronchus lobar bronchus segmental bronchus bronchiole terminal bronchiole. 6. In the respiratory division, all passages have alveoli along their walls or are alveoli themselves: respiratory bronchiole alveolare duct atrium alveolus. 7. An alveolus is a pouch about 0.2 to 0.5 mm in diameter. (Fig. 22.12) a. In contrast to frogs and amphibians with their simple single-sac lungs, mammals have lungs with 150 million little sacs, the alveoli, that provide about 70 m2 of surface for gas exchange. b. Thin, broad cells called squamous (type I) alveolar cells cover about 95% of the alveolar surface area. c. The other 5% is covered by round to cuboidal great (type II) alveolar cells. i. Although they cover less area, the type II cells greatly outnumber the type I cells. ii. Their functions are to repair the alveolar epithelium and to secrete pulmonary surfactant that prevents the alveoli and smallest bronchioles from collapsing during exhale. iii. Without surfactant, the walls of deflating alveoli would cling together like sheets of wet paper. d. The most numerous of all cells in the lung are alveolar macrophages (dust cells). i. These cells keep the alveoli free of debris by phagocytizing dust particles that escape entrapment by mucus. ii. In lungs that are infected or bleeding, they also phagocytize bacteria and loose blood cells. iii. As many as 100 million of them perish each day as they ride up the mucociliary escalator. e. Each alveolus is surrounded by a basket of blood capillaries supplied by the pulmonary artery. i. The barrier between the alveolar air and blood, called the respiratory membrane, consists only of the squamous alveolar cell, the squamous endothelial cell of the capillary, and their shared basement membrane. ii. These have a total thickness of only 0.5 μm, in contrast to the 7.5 um diameter of an erythrocyte. Saladin Outline Ch.22 Page 9 f. Fluid must be kept from accumulating in the alveoli because it interferes with gas diffusion. i. The alveolar wall has a thin film of moisture, and any excess liquid is absorbed by the blood capillaries. ii. The mean blood pressure of the capillaries is only 10 mm Hg, and the oncotic pressure is 28 mm Hg, so the osmotic uptake of water overrides filtration. g. The lungs have a more extensive lymphatic drainage than any other organ in the body. I. The surface of the lung is covered by the visceral pleura, a serous membrane that extends into the fissures. 1. At the hilum, the visceral pleura turns back on itself and forms the parietal pleura, which adheres to the mediastinum, inner surface of the rib cage, and superior surface of the diaphragm. (Fig. 22.10) 2. An extension of the parietal pleura, the pulmonary ligament, connects it to the diaphragm. 3. The space between the parietal and visceral pleurae is called the pleural cavity. a. The pleural cavity does not contain a lung, but rather wraps around it; the cavity contains nothing but a film of slippery pleural fluid. b. The cavity is thus termed a potential space, meaning there is normally no room between the membranes. 4. The pleurae and pleural fluid have three functions. a. Reduction of friction. Pleural fluid acts as a lubricant that eases lung expansion and contraction. b. Creation of a pressure gradient. Pressure in the pleural cavity is lower than atmospheric pressure. c. Compartmentalization. The pleurae, mediastinum, and pericardium compartmentalize the thoracic organs, preventing the spread of infection. II. Pulmonary Ventilation (pp. 875–886) A. Breathing, or pulmonary ventilation, consists of a repetitive cycle of inspiration (inhaling) and expiration (exhaling); one complete inspiration and exhalation is called a respiratory cycle. (p. 875) B. The lungs fill with air and empty of air when their volume expands and diminishes due to action of the respiratory muscles. (p. 876) C. Quiet respiration is the way one breathes at rest; forced respiration is unusually deep or rapid breathing, as in a state of exercise, singing, blowing, coughing, sneezing. (p. 876) Saladin Outline Ch.22 Page 10 D. The respiratory muscles are skeletal muscles of the trunk, especially the diaphragm and intercostal muscles. (p. 876–877) (Fig. 22.13) 1. The prime mover of pulmonary ventilation is the diaphragm. a. When relaxed, it bulges upward and the lungs are at their minimum volume. b. When the diaphragm contracts, it tenses and flattens somewhat, dropping about 1.5 cm in relaxed inspiration and as much as 7 cm in deep breathing. c. The diaphragm alone accounts for about two-thirds of pulmonary airflow. 2. Several muscles aid the diaphragm as synergists, chiefly the internal and external intercostal muscles. a. Their primary function is to stiffen the thoracic cage during respiration and prevent it from caving inward when the diaphragm descends. b. They also contribute to enlargement and contraction of the thoracic cage and add about one-third of the air that ventilates the lungs. c. During quite breathing, the scalene muscles of the neck fix ribs 1 and 2 while external intercostal muscles pull the other ribs upward like handles on a bucket. i. These actions increase both transverse and anterioposterior (AP) diameters of the chest. ii. In deep breathing, the AP diameter can increase by as much as 20%. 3. Other muscles of the chest and abdomen also aid in breathing, especially during forced respiration, and are termed accessory muscles of respiration: a. The erector spinae arches the back and aids in deep inspiration. b. Several muscles elevate the upper ribs: i. The sternocleidomastoids and scalenes of the neck. ii. the pectoralis minor, pectoralis major, and serratus anterior of the chest. iii. The intercartilaginous part of the internal intercostals. c. The scalenes elevate the upper ribs during forced inspiration. 4. Normal expiration is an energy-saving, passive process. a. The bronchial tree, attachments of ribs to spine and sternum, and tendons of diaphragm and other respiratory muscles spring back when the muscles relax. b. The muscles relax gradually in normal expiration, preventing the lungs from recoiling too suddenly. 5. In forced expiration, the rectus abdominus pulls down on the sternum and lower ribs, while the interosseous part of the internal intercostals pulls the other ribs downward. a. These actions reduce chest dimensions and expel air more rapidly and thoroughly. Saladin Outline Ch.22 Page 11 b. Many other muscles contribute to forced expiration, including lumbar, abdominal, and even pelvic muscles. c. Abdominal control of airflow is particularly important in singing and public speaking. 6. Thoracic pressure also affects abdominal pressure. a. Depression of the diaphragm raises abdominal pressure and helps expel the contents of certain abdominal organs, aiding in childbirth, urination, defecation, and vomiting. b. The Valsalva maneuver consists of taking a deep breath, holding it, and then contracting the abdominal muscles to raise abdominal pressure. E. Breathing is under neural control; the skeletal muscles of breathing cannot contract without nerve stimulation, and breathing involves a central coordinating mechanism. (pp. 877–880) 1. Breathing is controlled at two levels of the brain, one being cerebral and conscious, and the other being automatic and unconscious. 2. The automatic, unconscious cycle of breathing is controlled by three pairs of respiratory centers in the reticular formation of the medulla oblongata and pons. (Fig. 22.14) a. The ventral respiratory group (VRG) is the primary generator of the respiratory rhythm. i. It is an elongated nucleus in the medulla with two commingled webs of neurons: inspiratory (I) neurons and expiratory (E) neurons, each forming a reverberating neural circuit. ii. In quiet breathing (eupnea) the I neuron fires for about 2 seconds at a time. iii. Output travels by way of the phrenic and intercostal nerves. iv. As long as the I neurons are firing, they inhibit the E neurons. v. Eventually, I neuron activity wanes and E neurons begin firing; which further inhibit the I neurons and allow the inspiratory muscles to relax. vi. E neuron activity begins to wane after 3 seconds. vii. The respiratory rhythm produced is about 12 breaths per minute. b. The dorsal respiratory group (DRG) is another web of neurons that extends for much of the length of the medulla between the VRG and the central canal of the brainstem. i. The DRG is apparently an integrating center that receives input from several sources, including a respiratory center in the pons, a chemosensitive center in the anterior medulla oblongata, Saladin Outline Ch.22 Page 12 chemoreceptors in major arteries, and stretch and irritant receptors in the airway. ii. The DRG issues output to the VRG that modifies the respiratory rhythm to adapt to varying conditions. c. Each side of the pons has a pontine respiratory group (PRG) (formerly the pneumotaxic center) that modifies the rhythm of the VRG. i. The PRG receives input from higher brain center, including hypothalamus, limbic system, and cerebral cortex. ii. It issues output to both the DRG and VRG. iii. It hastens or delays the transition from inspiration to expiration, adapting breathing to special circumstances such as sleep, exercise, vocalization, and emotional responses. 2. The respiratory centers also receive central and peripheral input. a. Extreme anxiety, as one example, can produce hyperventilation that can lead to dizziness or fainting as CO2 is expelled quickly, causing a rise in pH. b. Multiple sensory receptors also provide information to the respiratory centers. i. Central chemoreceptors in the brainstem respond to changes in pH of cerebrospinal fluid. ii. Peripheral chemoreceptors in the carotid and aortic bodies of the large arteries respond to O2, CO2, and pH of the blood, conveying the information via cranial nerves to neurons of the DRG. iii. Stretch receptors in the smooth muscle of bronchi and bronchioles as well as visceral pleura respond to inflation of the lungs; excessive inflation triggers the inflation (Hering-Breuer) reflex that inhibits I neurons and stops inspiration. iv. Irritant receptors are nerve endings amid the epithelial cells of the airway that respond to smoke, dust, pollen, chemical fumes, cold air, and excess mucus; they transmit signals to the DRG that in turn initiates protective reflexes. 3. Voluntary control of breathing is important in singing, speaking, breath holding, and other circumstances. a. This control originates in the motor cortex of the frontal lobe of the cerebrum. b. Output neurons send impulses down corticospinal tracts to integrating centers in the spinal cord, bypassing the brainstem centers. c. Voluntary control has limits; holding one’s breath, for example, raises the CO2 level of the blood until a breaking point is reached and automatic control overrides one’s will. Saladin Outline Ch.22 Page 13 F. Laws of physics govern pressure, resistance, and airflow as well as transport of gases in the blood and their exchange with tissues. (pp. 880–883) (Table 22.1) 1. Respiratory airflow is governed by the same principles of flow, pressure, and resistance as blood flow: F ΔP/R. a. ΔP is the pressure difference that produces airflow. b. The pressure that drives respiration is atmospheric (barometric) pressure. i. At sea level, this pressure is 760 mm Hg, which is defined as 1 atmosphere. c. Pressure can be changed by changing the volume of the container. i. Boyle’s law states that at a constant temperature, pressure is inversely proportional to volume. ii. If lung volume increases, the internal pressure, or intrapulmonary pressure, falls. iii. If intrapulmonary pressure drops lower than atmospheric pressure, then air flows down its pressure gradient into the lungs. iv. If intrapulmonary pressure rises above atmospheric pressure, air flow out of the lungs. d. In discussions of the respiratory cycle, the difference between atmospheric and intrapulmonary pressure (relative pressure) is used. i. A relative pressure of –3 mm Hg means 3 mm Hg below atmospheric pressure. ii. A relative pressure of +3 mm Hg means 3 mm Hg above atmospheric pressure. 2. Inspiration is the flow of air into the lungs. (Fig. 22.16) a. At the beginning, there is no movement of the thoracic cage, no difference between air pressure inside and outside, and no airflow. b. As the thoracic cage expands, the two layers of pleura stick together like wet paper, and this stretches the alveoli within the lung; the entire lung expands. c. As the lung expands, its internal pressure drops, and air flow in. i. Between the two layers of pleura, the interpleural pressure is a slight vacuum at –4 mm Hg, and drops to about –6 mm Hg during inspiration. ii. Within the alveoli, the intrapulmonary pressure drops to about –3 mm Hg. d. Another force that expands the lungs is warming of inhaled air. i. According to Charles’s law, the volume of a gas is directly proportional to its absolute temperature. Saladin Outline Ch.22 Page 14 iv. On a day when the outside air temperature is 16°C (60°F), the air temperature will increase by 21°C (39°F) during inspiration as it warms to 37°C (99°F) by the time it reaches the alveoli. e. Inspiration stops when the intrapulmonary pressure is equal to the atmospheric pressure; in quiet breathing, the total volume increases by 500 mL. 3. Expiration is the flow of air out of the lungs. a. Relaxed expiration is a passive process achieved mainly by elastic recoil. i. Elastic recoil compresses the lungs, raising intrapulmonary pressure to about +3 mm Hg; air flows down its pressure gradient, out of the lungs. b. In forced breathing, the accessory muscles raise intrapulmonary pressure to as high as +30 mm Hg. c. The effect of pulmonary elasticity is evident in a pathological state of pneumothorax and atelectasis. i. Pneumothorax is the presence of air in the pleural cavity, such as due to a puncture of the thoracic wall, turning the potential space of the pleural cavity into an air-filled space. ii. Without negative intrapleural pressure, the lungs recoil and collapse (atelectasis). iii. Atelectasis can also result from airway obstruction, as blood absorbs gases from alveoli distal to the obstruction. 4. Resistance is another determinant of airflow: the greater the resistance, the slower the flow. a. Resistance in the lungs is governed by three factors: diameter of the bronchioles; pulmonary compliance; and surface tension of the alveoli and distal bronchioles. b. Diameter of the bronchioles. The ability of bronchioles to change their diameter make them the primary means of controlling resistance. i. An increase in the diameter of a bronchus or bronchiole is called bronchodilation, and a reduction is called bronchoconstriction. ii. Epinephrine and the sympathetic nerves stimulate bronchodilation. iii. Histamine, cold air, chemical irritants, and parasympathetic nerves stimulate bronchoconstriction. iv. Extreme bronchoconstriction may occur in anaphylactic shock or asthma. c. Pulmonary compliance. This term refers to the ease with which the lungs expand, or the change in lung volume relative to a given pressure change. Saladin Outline Ch.22 Page 15 i. The thoracic cage may produce the same intrapleural pressure in two different people, but lungs will expand less in the one with poorer pulmonary compliance. ii. Compliance can be reduced by degenerative lung diseases such as tuberculosis and black lung disease. d. Surface tension of the alveoli and distal bronchioles. The thin film of water over the epithelium of alveoli is necessary for gas exchange, but may be a problem for pulmonary ventilation if hydrogen bonding causes alveolar collapse. i. The great alveolar cells produce a surfactant, which disrupts hydrogen bonding and reduces surface tension. ii. This surfactant is composed of amphiphilic proteins and phospholipids, which are partially hydrophobic. iii. The molecules spread over the surface of the water film like floating ice cubes. iv. The surfactants resist compression as the alveolus deflates, retarding and then halting its collapse. v. Infant respiratory distress syndrome (IRDS) in premature infants is often treated by administering artificial surfactant. G. Gas exchange in alveoli, or alveolar ventilation, can be affected by different factors. (pp. 883– 884) 1. Not all air that is inhaled gets as far as the alveoli; about 150 mL of it fills the conducting division of the airway, which is termed the anatomical dead space since no gas exchange can occur there. 2. In pulmonary diseases, some alveoli may be unable to exchange gases because of reduced blood flow or thickened pulmonary membrane; physiological (total) dead space is the sum of anatomical dead space and any pathological alveolar dead space. a. In healthy people, the anatomical and physiological dead spaces are identical. 3. The anatomical dead space varies somewhat with circumstances. a. In a relaxed state, the parasympathetic stimulation keeps the airway somewhat constricted, minimizing the dead space. b. In a state of arousal, the sympathetic nervous system dilates the airway, increasing airflow, and the increased airflow outweighs the air wasted by filling the increased dead space. 4. The alveolar ventilation rate (AVR) is the amount of air that ventilates the alveoli times the respiratory rate. a. If 500 mL of air is inhaled, and 150 mL stays in the dead space, then 350 mL ventilates the alveoli. Saladin Outline Ch.22 Page 16 b. If the rate of respiration is 12 breaths per minute, then AVR = 350 mL × 12 breaths/min = 4,200 mL/min. 5. The alveoli never completely empty; there is always some leftover air called the residual volume, typically about 1,300 mL, that cannot be exhaled. a. This air mixes with fresh air, however, so the same air does not remain in the lungs cycle after cycle. H. Measurements of ventilation are commonly made using a spirometer, which recaptures expired breath and records rate and depth of breathing, speed of expiration, and rate of oxygen consumption. (pp. 884–885) (Fig. 22.17) (Table 22.2) 1. Respiratory volumes include tidal volume, inspiratory reserve volume, expiratory reserve volume, and residual volume. a. Tidal volume (TV) is the amount of air inhaled and exhaled in one cycle of quiet breathing, normally about 500 mL. b. The inspiratory reserve volume (IRV) is the amount beyond the TV that can be inhaled with maximum effort, typically about 3,000 mL. c. The expiratory reserve volume is the amount beyond the TV that can be exhaled with maximum effort, about 1,200 ML. d. The residual volume (RV) is the amount remaining after a maximum voluntary expiration, typically 1,300 mL. 2. Respiratory capacities are obtained by adding two or more of the respiratory volumes. a. Vital capacity (VC) is ERV + TV + IRV. b. Inspiratory capacity is TV + IRV. c. Functional residual capacity is RV + ERV. d. Total lung capacity is RV +VC. e. Vital capacity, the maximum ability to ventilate the lungs in one breath, is an important measure of pulmonary health. f. Respiratory volumes and capacities are usually proportional to body size, so they are generally higher for men than for women. 3. Spirometry is the measurement of pulmonary function and is an aid to diagnosis and assessment of restrictive and obstructive disorders. a. Restrictive disorders are those that reduce pulmonary compliance, limiting the amount to which the lungs can be inflated. i. They show as reduced VC. ii. Examples are diseases that cause pulmonary fibrosis, such as black lung disease and tuberculosis. b. Obstructive disorders are those that interfere with airflow by narrowing or blocking the airway. Saladin Outline Ch.22 Page 17 i. These diseases make it harder to inhale or exhale. ii. Examples are asthma and chronic bronchitis. iii. Emphysema combines elements of restrictive and obstructive disorders. iv. Obstructive disorders can be measured by having the subject exhale as rapidly as possible into a spirometer and measuring forced expiratory volume (FEV)—the percentage of vital capacity that can be exhaled in a given time interval. v. A healthy adult should be able to expel 75% to 85% of vital capacity in 1.0 second (the FEV1.0). vi. At home, patients can use a handheld meter to mearue peak flow, the maximum speed of expiration. 4. The amount of air inhaled per minute is the minute respiratory volume (MRV). a. The MRV largely determines the alveolar ventilation rate. b. It can be measured directly with a spirometer or obtained by multiplying tidal volume by respiratory rate. i. A TV of 500 mL times a rate of 12 breaths/min give an MRV of 6,000 mL/min. or 6 L/min. ii. During heavy exercise, MRV may be as high as 125 to 170 L/min, called the maximum voluntary ventilation (MVV), formerly the maximum breathing capacity. I. Respiratory rhythm may exhibit variations under different conditions. (pp. 885–886) 1. Relaxed, quiet breathing, or eupnea, is typically characterized by TV of 500 mL and respiratory rate of 12 to 15 breaths/min. 2. Conditions ranging from exercise or anxiety to various disease states can cause deviations such as abnormally fast, slow, or labored breathing. (Table 22.3) 3. Other variations serve purposes of speaking, expressing emotion, yawning, hiccupping, coughing, sneezing, etc. a. To cough, the glottis is closed and the muscles of expiration contract, producing high pressure; the glottis is suddenly opened and air is released in an explosive burst. b. Sneezing is triggered by irritants in the nasal cavity; the glottis is continually open, but the soft palate and tongue block the flow of air—when the soft palate is depressed, air is directed through the nose. c. Coughing and sneezing are coordinated by center in the medulla oblongata. III. Gas Exchange and Transport (pp. 886–896) Saladin Outline Ch.22 Page 18 A. Air is composed of about 78.6% nitrogen, 20.9% oxygen, 0.04% carbon dioxide, several minor gases such as argon, neon, helium, methane, and ozone, and a variable amount of water vapor (0% to 4%). (p. 886–887) 1. The total atmospheric pressure is a sum of the contributions of each gas in the mixture, a principle known as Dalton’s law. (Table 22.1) a. The separate contribution of each gas is called its partial pressure, which is symbolized by P followed by the gas formula, e.g. PN2. b. If sea level pressure is 760 mm Hg and nitrogen is 78.6% of this, then P N2 is simply 0.786 × 760 mm Hg = 597 mm Hg. c. For all major gases in the atmosphere, P N2 + PO2 + PH2O + PCO2 = 597 + 159 + 3.7 + 0.3 = 760 mm Hg. 2. The composition of air exhaled is not the same; it differs because of three influences. (Table 22.4) a. It is humidified, so its PH2O is 10 times higher. b. Its oxygen is diluted and it is enriched with CO2 from the residual air left in the respiratory system. c. Alveolar air exchanges O2 and CO2 with the blood, so the PO2 of alveolar air is about 65% that of inhaled air, and the P CO2 is more than 130 times higher. B. The back-and-forth traffic of oxygen and carbon dioxide across the respiratory membrane is called alveolar gas exchange. (p. 887–890) 1. Each gas diffuses down its pressure gradient until the partial pressure of each gas in the air is equal to its partial pressure in the water, namely the water film on the surface of alveoli and the blood plasma in surrounding capillaries. 2. Henry’s law states that at the air–water interface, at a given temperature, the amount of gas that dissolves in water is determined by its solubility in water and its partial pressure in the air. (Fig. 22.18) a. The greater the PO2 in alveolar air, the more O2 the blood picks up; and the greater the PCO2 in the blood, the more CO2 is released into alveolar air. b. The blood is said to unload CO2 and load O2. c. The diffusion of one gas does not influence the diffusion of another. 3. Both loading and unloading involve RBCs and how long an RBC spends in an alveolar capillary compared with how long it takes for each gas to reach equilibrium. a. It takes about 0.25 sec for gases to reach equilibrium. b. At rest, an RBC passes through an alveolar capillary in about 0.75 sec. c. Even in vigorous exercise, an RBC spends about 0.3 sec. in the alveolar capillary, which is still adequate. 4. Several variables affect the efficiency of alveolar gas exchange. Saladin Outline Ch.22 Page 19 a. Pressure gradients of the gases. Blood entering the lungs has a PO2 of 40 mm Hg and a PCO2 of 46 mm Hg; blood leaving has a PO2 of 95 mm Hg and a PCO2 of 40 mm Hg. i. These gradients differ under circumstances such as high elevation and hyperbaric oxygen therapy (treatment with oxygen at greater than 1 atm of pressure (Fig. 22.20) ii. Treatment in a hyperbaric oxygen chamber at 3 or 4 atm is used for conditions such as gangrene and carbon monoxide poisoning. iii. The PO2 in such a chamber may be between 2,300 and 3,000 mm Hg. b. Solubility of gases. Gases have different solubilities in water, with carbon dioxide being about 20 times as soluble as oxygen, and oxygen being about twice as soluble as nitrogen. i. Even though the pressure gradient of oxygen is higher, equal amounts of oxygen and carbon dioxide are exchanged because CO2 is so much more soluble. c. Membrane thickness. The respiratory membrane is only 0.5 um thick and presents little obstacle to diffusion, but some conditions can affect this. (Fig. 22.21a) i. In left ventricular failure, blood pressure back up into the lungs and causes the respiratory membranes to become edematous and thickened, similar to in pneumonia. (Fig. 22.21b) ii. Gases have farther to travel between blood and air, and cannot reach equilibrium quickly enough, so the blood leaving the lungs has high PCO2 and low PO2. d. Membrane area. Each healthy lung has about 70 m2 of respiratory membrane available. i. Several pulmonary diseases decrease the alveolar surface, such as lung cancer, tuberculosis, and emphysema. (Fig. 22.21c) e. Ventilation–perfusion coupling. Ventilation of the alveolus is required, but a good perfusion of its capillaries is also needed. i. As a whole, the lungs have a ventilation–perfusion ratio of about 0.8—a flow of 4.2 L of air and 5.5 L of blood per minute at rest. ii. Ventilation–perfusion coupling is the ability to match ventilation and perfusion to each other. (Fig. 22.22) iii. If part of a lung is poorly ventilated because of tissue destruction or airway obstruction, there is little point in directing blood there. Saladin Outline Ch.22 Page 20 iv. Poor ventilation causes local constriction of the pulmonary arteries, redirecting blood to better-ventilated alveoli. v. Good ventilation dilates the arteries and increases perfusion so that most blood is directed to regions where it can pick up the most oxygen. vi. This is the opposite from the reactions of systemic arteries, where oxygen deficiency causes vasodilation. vii. Poor ventilation also causes local carbon dioxide accumulation, which stimulates local bronchodilation and improves airflow; low carbon dioxide stimulates bronchoconstriction. C. Gas transport is the process of carrying gases from the alveoli to the systemic tissues and vice versa. (pp. 890–891) 1. Arterial blood carries about 20 mL of oxygen per deciliter. a. About 98.5% of the oxygen is bound to hemoglobin in RBCs and 1.5% is dissolved in the blood plasma. b. Hemoglobin is a molecule specialized for oxygen transport. i. It consists of four protein (globin) chains each with one heme group that can bind 1 oxygen molecule. ii. Each hemoglobin can therefore carry up to 4 O 2. iii. A hemoglobin with one or more oxygen molecules bound to it is called oxyhemoglobin (HbO2). iv. A hemoglobin with no oxygen bound to it is called deoxyhemoglobin (HHb). v. When hemoglobin is 100% saturated, every molecule carries 4 oxygens; if 75% saturated, an average of 3 oxygens; and so on. vi. The poisoning effects of carbon monoxide (CO) have to do with its competition with oxygen for the hemoglobin binding site. Insight 22.3 Carbon Monoxide Poisoning c. The relationship between hemoglobin saturation and P O2 is shown by the oxyhemoglobin dissociation curve. (Fig. 22.23) i. The curve is not a straight line. ii. At low PO2 the curve rises slowly; once the first heme group binds oxygen, however, the second oxygen is bound more quickly. iii. The same is true for the third and fourth oxygens, reflected in the rapidly rising midportion of the curve. iv. At high PO2 levels, the curve slows again because of saturation. 2. Carbon dioxide is transported in three forms: carbonic acid, carbamino compounds, and dissolved gas. Saladin Outline Ch.22 Page 21 a. About 90% of the carbon dioxide is hydrated to from carbonic acid, which then dissociates to form bicarbonate and hydrogen ions. b. About 5% binds to the amino groups of plasma proteins and hemoglobin to form carbamino compounds, chiefly carbaminohemoglobin (HbCO 2). i. Carbon dioxide does not compete with oxygen because it binds to a different site—namely the polypeptide chains, not the heme group. ii. Hemoglobin can therefore transport both O2 and CO2 simultaneously; however, each gas somewhat inhibits transport of the other. c. The remaining 5% of the carbon dioxide is carried in the blood as dissolved gas. d. The relative amounts of CO exchanged between the blood and alveolar air differ from the percentages just given. i. About 70% of the exchanged CO2 comes from carbonic acid, 23% from carbamino compounds, and 7% from the dissolved gas. ii. Blood gives up CO2 from dissolved gas and from the carbamino compounds more easily than it gives up the CO2 in bicarbonate. D. Systemic gas exchange is the unloading of O2 and the loading of CO2 at the systemic capillaries. (p. 891–892) (Figs. 22.19, 22.24) 1. Carbon dioxide loading occurs because aerobic respiration produces a molecule of CO2 for every molecule of O2 it consumes, and tissue therefore contains a relatively high PCO2. a. There is a gradient of 46 40 mm Hg from tissue fluid to blood. b. Consequently, CO2 diffuses into the blood stream and is carried in the three forms already noted. c. Most reacts with water to produce bicarbonate (HCO3–) and hydrogen ions (H+). i. This reaction occurs slowly in blood plasma, but more quickly in RBCs where it is catalyzed by carbonic anhydrase. ii. An antiport called the chloride–bicarbonate exchanger then pumps most of the HCO3– out of the RBC in exchange for Cl– from the blood plasma, an exchange called the chloride shift. d. Most of the H+ binds to hemoglobin or oxyhemoglobin, which buffers the intracellular pH. 2. Oxygen unloading begins as H+ binds to oxyhemoglobin, which reduces the affinity of hemoglobin for O2 and tends to make hemoglobin release it. Saladin Outline Ch.22 Page 22 a. Oxygen consumption by respiring tissues keeps the P O2 of tissue relatively low, so typically there is a pressure gradient of 95 40 mm Hg between arterial blood to the tissue fluid. b. Thus, the liberated oxygen along with dissolved gas, diffuses from the blood into the tissue fluid. c. As blood arrives at the systemic capillaries, its oxygen concentration is about 20 mL/dL and the hemoglobin is about 97% saturated. d. As it leaves the capillaries of a typical resting tissue, its oxygen concentration is about 15.6 mL/dL and the hemoglobin is about 75% saturated. i. It has given up about 4.4 mL/dL—about 22% of its oxygen load. ii. This fraction is called the utilization coefficient. iii. The oxygen remaining in the blood after it passes through the capillary bed provides a venous reserve of oxygen, whch can sustain life for 4 to 5 minutes in the case of respiratory arrest. e. At rest the circulatory system releases oxygen to the tissues at an overall rate of about 250 mL/min. E. Looking back at alveolar gas exchange, the reactions that occur in the lungs are essentially the reverse of systemic gas exchange. (pp. 892–893) (Figs. 22.4, 22.25) 1. As hemoglobin loads oxygen, its affinity for H+ declines, and these ions dissociate from the hemoglobin and bind with bicarbonate ions transported into RBCs. 2. Chloride ions are transported back out of the RBCs (a reverse chloride shift). 3. The reaction of hydrogen ions and bicarbonate reverses the hydration reaction and generates free CO2. 4. The CO2 diffuses into the alveolus to be exhaled, as does the CO2 gas dissolved in plasma and that released from carbaminohemoglobin. F. Oxygen release must be adjusted to meet the needs of individual tissues. (pp. 893–894) 1. Four factors adjust the rate of oxygen unloading to the metabolic rates of different tissues. a. Ambient PO2. An active tissue consumes oxygen rapidly, so the P O2 of its tissue fluid remains low, causing more oxygen to be released from HbO 2. b. Temperature. Elevated temperature, such as that in active tissue, causes more dissociation and release of oxygen. c. The Bohr effect. Active tissues generate more CO2, which lowers blood pH and causes more dissociation and thus release of oxygen. i. The increase in dissociation in response to low pH is called the Bohr effect. Saladin Outline Ch.22 Page 23 ii. It is less pronounced at the high PO2 present in the lungs, so it has little effect on pulmonary oxygen loading. iii. In the systemic capillaries, where PO2 is lower, the effect is more pronounced. d. BPG. Erythrocytes meet energy needs via anaerobic fermentation, and one of their metabolic intermediates, bisphosphoglycerate (BPG), binds to hemoglobin and promostes oxygen unloading. i. Elevated temperature as well as thryoxine, growth hormone, testosterone, and epinephrine all stimulate BPG synthesis and release of oxygen. 2. The rate of CO2 loading is also adjusted to varying needs of the tissues. a. A low level of HbO2 enables the blood to transport more CO2, an effect called the Haldane effect. b. It occurs for two reasons. i. HHb (deoxyhemoglobin) binds CO2 better than HbO2 does. ii. HHb binds more hydrogen ions than does HbO2, shifting the carbonic acid reaction to produce more bicarbonate and H+. G. Blood gases affect the respiratory rhythm. (pp. 894–896) 1. The PO2 of systemic arterial blood is normally 95 mm Hg and the P CO2 is 40 mm Hg, with a pH of 7.4 ± 0.05. (Fig. 21.21a) a. The rate and depth of breathing are adjusted to maintain these values. b. The chemoreceptors of the CNS and peripheral nervous system monitor blood composition and relay signals to the brainstem respiratory centers. c. The most potent stimulus for breathing is pH, followed by CO 2; the least significant is O2. 2. Pulmonary ventilation is adjusted ultimately to maintain the pH of the brain. a. Hydrogen ions do not cross the blood–brain barrier easily, but CO2 does, and once in the CSF, it reacts with water to produce H+. b. Central receptors in the medulla oblongata produce about 75% of the change in respiration due to pH; peripheral receptors about 25%. c. A blood pH lower than 7.35 is called acidosis, and a pH greater than 7.45 is called alkalosis. d. The PCO2 of arterial blood is normally 37 to 43 mm Hg. i. A PCO2 less than 37 mm Hg is called hypocapnia and is the most common cause of alkalosis. ii. A PCO2 greater than 43 mm Hg is called hypercapnia, and is the most common cause of acidosis. Saladin Outline Ch.22 Page 24 iii. The result of both shifts in PCO2 is pH imbalance, and they are termed respiratory alkalosis and respiratory acidosis. e. Increased breathing rate helps to correct acidosis by removing CO 2 from the blood so that the carbonic acid reaction shifts to the left. f. A slower breathing rate helps to correct alkalosis by shifting the reaction to the right. g. In diabetes mellitus, rapid fat oxidation releases acidic ketone bodies, causing an abnormally low pH called ketoacidosis. i. Ketoacidosis tends to induce a form of dyspnea called Kussmaul respiration. (Table 22.3) ii. This reduces the H+ to some extent and compensates somewhat for the H+ released by ketone bodies. 3. Aside from its role in pH, CO2 concentration has a more direct effect on breathing rate even when pH remains stable, such as at the beginning of exercise. 4. The PO2 has little effect on respiration, and only if arterial P O2 drops below 60 mm Hg. a. At low elevations, such a low PO2 seldom occurs. b. At about 10,800 feet (3,300 m), P O2 falls to 60 mm Hg, and the stimulatory effect of hypoxemia on carotid bodies overrides the inhibitory effect of the pH increase, and produce heavy breathing in those not acclimated. c. Long-term hypoxemia can lead to a condition called hypoxic drive, in which respiration is driven more by low P O2 than by pH or CO2. i. This occurs in conditions such as emphysema and pneumonia, and in mountain climbing of at least 2 or 3 days’ duration. 5. Increased respiration during exertion has causes other than pH or gas concentrations. a. When the brain sends motor commands to the muscles, it also sends information to the respiratory centers that then increase pulmonary ventilation. b. Exercise stimulates proprioceptors of muscles and joints, and these transmit excitatory signals to the brainstem respiratory centers. c. In this way, the blood gas values are kept near normal regardless of the increased O2 consumption and CO2 generation. IV. Respiratory Disorders (pp. 896–899) A. Oxygen imbalances include hypoxia and oxygen toxicity. (p. 896) 1. Hypoxia is a deficiency of oxygen in a tissue or the inability to use oxygen; it is not a respiratory disease but is often a consequence of respiratory disease. 2. Hypoxia is classified according to cause. a. Hypoxemic hypoxia is a state of low arterial P O2 and is usually due to inadequate pulmonary gas exchange. Saladin Outline Ch.22 Page 25 i. Some of its causes include atmospheric deficiency at high elevations, impaired ventilation as in drowning, respiratory arrest, and degenerative lung diseases. ii. It also occurs in carbon monoxide poisoning. b. Ischemic hypoxia results from inadequate blood circulation, as in congestive heart failure. c. Anemic hypoxia is due to anemia and inability of the blood to carry oxygen. d. Histotoxic hypoxia occurs when a metabolic poison such as cyanide prevents tissues from using the oxygen delivered to them. 3. Hypoxia may be indicated by cyanosis, a bluish tinge to the skin; its primary effect is necrosis of oxygen-starved tissues, especially critical in the brain, heart, and kidneys. 4. Oxygen toxicity can occur when pure oxygen is breathed at 2.5 atm or greater. a. It is safe to breathe 100% oxygen at 1 atm for a few hours. b. Excess oxygen generates hydrogen peroxide and free radicals that destroy enzymes and damage nervous tissue. c. Hyperbaric oxygen was formerly used to treat premature infants for respiratory distress syndrome, but it blinded many infants before it was discontinued. B. Chronic obstructive pulmonary disease (COPD) refers to any disorder in which there is a longterm obstruction of airflow and a substantial reduction in pulmonary ventilation. (pp. 896–897) 1. The major COPDs are chronic bronchitis and emphysema. a. COPDs are almost always caused by smoking, but occasionally result from air pollution or occupational exposure to irritants. b. Some classify asthma as a COPD, but the National Institutes of Health no longer do so. 2. In chronic bronchitis, the cilia are immobilized and reduced in number, while goblet cells enlarge and produce excess mucus. a. As a result, smokers develop a chronic cough that brings up sputum, a mixture of mucus and cellular debris. b. Thick, stagnant mucus in the respiratory tract provides a growth medium for bacteria, while cigarette smoke incapacitates alveolar macrophages and reduces defense mechanisms. c. Smokers therefore develop chronic infection and inflammation, with dyspnea, hypoxia, cyanosis, and coughing attacks. 3. In emphysema, alveolar walls break down and the lung exhibits larger but fewer alveoli. (Fig. 22.21c) a. There is less respiratory membrane available for gas exchange. Saladin Outline Ch.22 Page 26 b. The lungs become fibrotic and less elastic. c. The air passages open adequately during inspiration, but they tend to collapse and obstruct airflow during expiration. i. Over a period of time, a person becomes barrel-chested. ii. The overly stretched thoracic muscles contract weakly, which further contributes to difficult exhaling. iii. People with emphysema become exhausted simply from the effort needed to breathe. 4. COPD tends to reduce pulmonary compliance and vital capacity and causes hypoxemia, hypercapnia, and respiratory acidosis. a. Hypoxemia stimulates secretion of erythropoietin by the kidneys, which leads to polycythemia. b. COPD also leads to cor pulmonale, the hypertrophy and potential failure of the right heart due to obstruction of pulmonary circulation. C. Lung cancer accounts for more deaths than any other form of cancer, and its most important cause is cigarette smoking. (pp. 897–898) (Fig. 22.27) 1. Cigarette smoke contains at least 15 carcinogenic compounds. 2. Lung cancer commonly follows or accompanies COPD. 3. There are three forms of lung cancer. a. Squamous-cell carcinoma is the most common form; it arises in basal cells of the bronchial epithelium. i. The ciliated pseudostratified epithelium transforms into the stratified squamous type. ii. These invade the underlying tissues of the bronchial wall, causing bleeding lesions. iii. Swirled masses of keratin appear in the lung parenchyma and replace functional tissue. b. Adenocarcinoma is nearly as common as the first type. i. This cancer originates in the mucous glands of the lamina propria. c. Small-cell (oat-cell) carcinoma is the least common but most dangerous form. i. It is named for clusters of cells that resemble oat grains. ii. It originates in the main bronchi, invades the mediastinum, and metastasizes quickly to other organs. d. Over 90% of lung tumors originate in the mucous membranes of the large bronchi. i. As the tumor invades the bronchial wall and grows, it compresses the airway and may cause atelectasis of distal parts of the lung. Saladin Outline Ch.22 Page 27 ii. Growth of the tumor produces a cough, but smokers cough so much that this is seldom a cause of alarm. iii. Often, the first sign of serious trouble is coughing up blood. e. Lung cancer metastasizes so rapidly that it has usually spread to other organs by the time it is diagnosed. f. The chance of recovery is poor, with only 7% of patients surviving for 5 years after diagnosis. 4. Table 22.5 describes additional respiratory system disorders. Insight 22.4 Diving Physiology and Decompression Sickness Connective Issues: Respiratory Interactions Cross Reference Additional information on topics mentioned in Chapter 22 can be found in the chapters listed below. Chapter 2: Cellular respiration Chapter 10: The infrahyoid group of muscles Chapter 16: Olfactory epithelium Chapter 18: Structure of hemoglobin Chapter 18: Polycythemia Chapter 19: Cor pulmonale Chapter 24: Respiratory acidosis and alkalosis Chapter 26: Details of cellular respiration Chapter 29: Breathing difficulties of premature infants