* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download table of contents - Oregon State University
Psychoneuroimmunology wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adaptive immune system wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
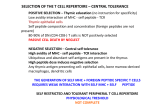
AN ABSTRACT OF THE THESIS OF Jacob Huber for the degree of Baccalaureate of Science in Bioresource Research, Toxicology Option, presented on June 12, 2007. Title: Method Development in In Vitro Immune Response Abstract approved: ________________________________________________________________________ Dr. Nancy I. Kerkvliet The AhR is a ligand-activated transcription factor that mediates the potent immunosuppressive effects of TCDD. AhR-dependent changes in gene expression appear to alter the differentiation of CD4+ T cells to induce a population of CD4+CD25+ T regulatory cells (Tregs) that suppress the immune response. Ascertaining if and how the AhR induces Tregs is clinically relevant. Tregs act to suppress activation of the immune system, maintain immune system homeostasis, and tolerance to self. If the immunosuppressive functions of Tregs could be controlled via activation of the AhR for example, autoimmune diseases could potentially be treated, and the immune system could be prevented from rejecting transplanted organs. An in vitro model was designed to test the hypothesis that TCDD acts directly on the AhR in T cells to induce CD4+CD25+ Tregs. A method was developed to extract dendritic cells from the spleens of B6D2F1 mice. T cells were isolated from the spleens of C57Bl/6 AhR-/- and AhR+/+ mice. Splenic dendritic cells are potent activators of T cells. TCDD was added to cultures at concentrations of 1x10-8, 1x10-9, 1x10-10, and 1x10-11. TCDD had no notable effect on T cell viability or CD25 expression. TCDD did however increase the percentage of dividing CD4+ T cells that downregulated CD62L, an effect that was also seen in vivo on CD4+CD25+ T cells. These results suggest that TCDD acts directly on CD4+ T cells to alter CD62L expression, but further differentiation into Tregs was not observed. Future studies will examine other culture conditions that may support direct AhR-dependent induction of Tregs. Method Development in In Vitro Immune Response by Jacob Huber A THESIS submitted to Oregon State University Bioresource Research in partial fulfillment of the requirements for the degree of Baccalaureate of Science in Bioresource Research, Toxicology Presented June 12, 2007 Commencement June 2007 Baccalaureate of Science in Bioresource Research, Biotechnology Thesis of Jacob Huber Presented on June 12, 2007 APPROVED: Nancy Kerkvliet, Mentor David Farrer, Secondary Mentor Anita Azarenko, Director of Bioresource Research I understand that my project will become part of the permanent collection of Oregon State University, Bioresource Research. My signature below authorizes release of my project to any reader upon request. Jacob Huber, Author ACKNOWLEDGEMENTS I would like to thank Dr. Nancy Kerkvliet for giving me the opportunity to work in her lab, for being a great teacher, and for guiding my research experience and making it the best it could be. I would also like to thank Dr. David Farrer for teaching me all about virtually everything in the lab, for running the (successful!) TCDD experiment for me at the last minute, and for all the time he put in helping me with experiment design and corrections to this thesis. Thanks go to Linda Steppan for helping me troubleshoot experiments, find reagents, and locate the right mice. I also owe thanks to Danielle King for all the help with flow cytometry. Thanks to everyone else in the lab for all their help and suggestions! In addition, I thank my family for supporting me throughout my undergraduate years. 2 List of Abbreviations AhR - Aryl hydrocarbon receptor AutoMACS – Automated magnetic cell sorter BM – Bone marrow BSA – Bovine serum albumin CD – Cluster of differentiation CFSE - Carboxyfluorescein succinimidyl ester DMSO – Dimethyl sulfoxide DC – Dendritic cell EMA – Ethidium monoazide FBS – Fetal bovine serum GM-CSF - Granulocyte-macrophage colony-stimulating factor GVH – Graft versus host H – Hours HEPES - 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid IACUC - Institutional Animal Care and Use Committee M - Molar MHC – Major histocompatibility complex Min – Minutes NK – Natural killer cell PBS – Phosphate buffered saline RCF – Relative centrifugal force S - Seconds TCDD - 2,3,7,8-tetrachlorodibenzo-p-dioxin Tregs – T regulatory cells TABLE OF CONTENTS Page 1. Introduction…………………………………………………............... 1 2. Materials and methods……………………………………….............. 5-9 2. Mice …………………………....................................................... 2.2 TCDD Treatment…………………………………….................. 2.3 Reagents and Incubation ……………………………………….. 2.4 AutoMACs Cell Sorter…………………………………………. 2.5 Bone Marrow Cultures…………………………………..……… 2.6 Splenic Dendritic Cell Isolation 1 ……………………................ 2.7 Splenic Dendritic Cell Isolation 2………………………….…… 2.8 Splenic T Cell Isolation………………………………………… 2.9 Immunofluorescent Staining and Flow Cytometry ………...…... 3.0 Statistics………………………………………………………… 3. Results………………………………………………………………... 5 5 5 6 6 7 7 8 8 10 11-17 3.1 T Cell Isolation…………………………………………………. 3.2 Dendritic Cell Isolation…………………………………………. 3.3 Dendritic Cell:T Cell Ratio Optimization ……………………… 3.4 TCDD Experiment 1……………………………. 3.5 TCDD Experiment 2………………………… 4. Discussion……………………………………………………………. 11 11 12 14 15 18-20 5. References……………………………………………………………. 21 LIST OF FIGURES Figure Page 1. Sample Flow Cytometry Histograms for Viability and Cell Division 9 Assessment 2. CD4 and CD8 T Cell Gating 9 3. Dendritic Cell Ratio Experiment 12 4. TCDD Experiment One, Lack of Division 13 5. Cellular Viability 14 6. CD25 Expression on Dividing CD4+ T Cells 14 7. Dividing CD4+ and CD8+ T cells, Percentage 15 8. Dividing CD4+ and CD8+ T cells, CD62L Downregulation 15 1. Introduction In vivo immunosuppressive effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) have been well documented. Most recently it has been shown that TCDD induces alloreactive CD4+ T cells to differentiate into T regulatory-like cells (Tregs) that functionally inhibit naïve T cell proliferation in suppression assays (3). Alloreactive cells are those that are specifically reactive to non-self major histocompatibility complex (MHC) molecules, and represent about 1-10% of naïve T cells. TCDD-induced Tregs express several cell surface markers in common with traditional Tregs. For example, TCDD-induced Tregs have high expression of CD25, GITR, and CD28. However, TCDDinduced Tregs differ from traditional Tregs in that they lack foxp3 expression and CD62L expression is downregulated. In the graft versus host model (GVH), donor T cells from a parent mouse strain are adoptively transferred into a host F1 mouse of which one parent is from the same strain as the donor mouse and the other parent is allogeneic to the donor strain. The donor T cells recognize the disparate polymorphisms at the MHC locus and respond by proliferation and differentiation into effector cells that attack the host (thus inducing GVH disease). In TCDD-treated mice, the T cells proliferate normally but differentiate into CD25-expressing Treg-like cells, and GVH disease is suppressed (2,3). This TCDDinduced change in T cell differentiation has been shown to be mediated by a liganddependent transcription factor known as the aryl-hydrocarbon receptor (AhR). The AhR belongs to the PER-ARNT-SIM family of transcriptional regulators. Its ligands are diverse and include products of cellular metabolism such as tryptophan and 2 arachidonic acid metabolites, as well as other dietary components. TCDD is the most potent agonist due to its high binding affinity and resistance to metabolism (3). When AhR knockout mice are used as the source of donor CD4+ T cells in the GVH model, TCDD does not alter T cell differentiation and there is no induction of Tregs (3). These results suggest that TCDD acts through the AhR in T cells to drive their differentiation into Tregs.. It has also been demonstrated that the AhR is needed in both CD4+ and CD8+ cells for complete suppression of the GVH, and that some of the effects on CD8+ cells are mediated by AhR-competent CD4+ T cells (7). I tested the hypothesis that TCDD acts directly on the CD4+ T cells via the AhR to alter their differentiation and induce a Treg phenotype. CD4+ T cells were treated with TCDD in vitro in order to ascertain whether it directly stimulates CD4+ T cell differentiation toward Tregs. The response of T cells from AhR-/- were used in parallel. If TCDD directly affects CD4+ T cells via the AhR, addition of TCDD to the cultures should cause effects in AhR+/+ but not AhR-/- T cells. Therefore, the goal was to develop an in vitro model that is able to recapitulate the effects of TCDD that are seen in the in vivo GVH model. An in vitro GVH model would have several advantages over the in vivo model. Foremost, it is very expensive to carry out in vivo animal experiments which require large numbers of animals as well as expensive reagents and equipment. Animal studies also take a considerable amount of time compared to in vitro studies. Last but not least, a suitable in vitro model could be used to quickly and economically screen for other potential ligands of the AhR since TCDD itself is unlikely to be used as a drug to treat human diseases. TCDD is a known potent immunosuppressive agent, but it has other significant toxic effects. It is a byproduct of combustion, and is also generated in the 3 production of chlorophenols and chlorophenoxy herbicides, and the bleaching of paper with free chlorine (1). It has been demonstrated that TCDD is a potent carcinogen in animal studies. Exposure in high doses can result in chloracne. TCDD has also been shown to be hepatotoxic, mutagenic, and teratogenic. Because of these properties it would not be suitable for clinical work where immunosuppression is desired. Ascertaining if and how the AhR induces Tregs is clinically relevant. Tregs act to suppress activation of the immune system, maintain immune system homeostasis, and tolerance to self. If the immunosuppressive function of Tregs could be controlled, via the AhR for example, autoimmune diseases could potentially be treated, and the immune system could be prevented from rejecting transplant organs. Current immunosuppressive drugs often broadly suppress the immune system, but it is possible suppression could be targeted with the use of specific Tregs through the AhR. This would allow the body to accept a transplant but also maintain its ability to fight disease, which is hindered by today’s immunosuppressive drugs. If another ligand could be found for the AhR that does not exhibit other toxic effects like TCDD, it could prove useful in such treatments. This further demonstrates the need for an efficient, quick in vitro screening model mimicking the GVH. An allo DC-T cell culture was used in these studies as an in vitro model of the early events that occur in vivo in the GVH model. The alloDCs from B6D2F1 mice stimulate CD4+ T cells from C57Bl/6 mice to proliferate and differentiate into effector cells. DCs express both class I and class II MHC antigens, and have been shown to be efficient presenters of antigen to both CD4+ and CD8+ T lymphocytes (7). Some of the T cells that proliferate will differentiate into Tregs with progressive rounds of cell division and express increased levels of CD25, which is a marker used to assess the endpoint. 4 CD62L, which is expected to show decreased expression levels with progressive rounds of division, was also used for endpoint assessment (3). How levels of expression of these two cell surface markers change with the addition of TCDD and the differences between AhR+/+ and AhR-/- T cells were the endpoints of interest. Hypothesis: TCDD acts directly on CD4+ T cells via the AhR to alter their differentiation 5 2. Materials and Methods 2.1 Mice Dendritic cells were collected from the spleens of male and female B6D2F1 mice. T cells were isolated from the spleens of male and female C57BL6 congenic Thy 1.1 mice AhR-/- and AhR+/+ mice. Donor and host mice were gender matched. C57BL6 AhR +/- mice were used in some optimization experiments. The mice were euthanized by asphyxiation using CO2. They were handled according to the rules of animal welfare as outlined by IACUC. 2.2 TCDD Treatment TCDD dissolved in DMSO was added to the tissue culture media at concentrations of 1x10-8, 1x10-9, 1x10-10, and 1x10-11. DMSO only at the same concentration as in the TCDD treatment, and controls without either treatment were cultured as well. 2.3 Reagents and Incubation RPMI-1640 (Hyclone Labs) supplemented with 10% Fetal Bovine Serum (FBS, Hyclone Labs), 2-ME (Sigma Cell Culture), Gentamicin (GIBCO), and L-Glutamine (Invitrogen) was used as a culture media. Spleens were processed in a media consisting of Hanks Balanced Salt Solution (Sigma Cell Culture) diluted to a working concentration in water, 2.5% FBS,, and Gentamicin, except during the collagenase digestion where the media consisted of HBSS with calcium and magnesium. Both calcium and magnesium are required by the Collagenase D (Roche Applied Science) enzyme. An RPMI-5 media was made up for the enrichment of dendritic cells by plastic adherence. This consisted of RPMI-1640, 5% FBS, HEPES, Gentamicin, and 2-ME. Trypan Blue was used occasionally to determine viability. A dense bovine serum albumin (BSA, Intergen) solution for the gradient was prepared from BSA, PBS, and water. All incubations were carried out at 37ºC and 5% CO2. 6 2.4 AutoMACs Cell Sorter The AutoMACs automated magnetic cell sorter is able to separate cells based on proteins that are variably expressed on the surface of different cells. Cells are labeled with antibodies (conjugated to biotin) based on their unique cell surface markers. Next, magnetic beads conjugated to anti-biotin antibodies are used to label the biotin conjugated antibodies. After this labeling the cells are allowed to pass through a column in a magnetic field. In this column, labeled cells are retained and unlabeled cells are allowed to pass through. Positive and negative populations can be isolated and further purified via the use of additional surface markers and magnetic beads. 2.5 Bone Marrow Cultures In initial studies, dendritic cells were derived from progenitors in the bone marrow of B6D2F1 mice. The bone marrow was collected from the femur and tibia of both rear legs. The femur and tibia were separated from each other, after which the heads of the bone were cut off at both ends. The marrow was then flushed out with a 25 gauge needle and a syringe filled with media. After the marrow was collected, the red blood cells were lysed. After RBC lysis, the cells were resuspended in RPMI culture media and seeded into a (non-TC) treated Petri dish. They were then cultured for 3 days, allowing many cells types, predominantly macrophages, and granulocytes to adhere to the dish. The non-adherent cells were collected and transferred to a new Petri dish with fresh RPMI culture media as well as granulocyte/macrophage colony-stimulating factor (GMCSF). GM-CSF stimulates the generation of three lineages of myeloid cells: granulocytes, macrophages, and dendritic cells from progenitors in the bone marrow (4). As the contaminating macrophages and granulocytes have been removed in the initial plastic adherence step, dendritic cells are left to mature. 7 2.6 Splenic Dendritic Cell Isolation 1 Dendritic cells were also isolated from the spleen. First, spleens were ground using microscope slides, and digested in collagenase D for 30 min to break up the capsule and increase DC recovery. This digested suspension was panned on antibody coated dishes to remove B cells. The plates were first coated with antibodies specific for B cell markers (such as CD19) and then the suspension was added. The dish was then swirled for 30 s to allow the B cells to stick to the antibodies coating the plate. Cells in the supernatant (non-adherent) were then collected and labeled with antibodies against CD11b. CD11b+ cells (primarily macrophages) were depleted with the AutoMACs sorter. Unlabeled cells that made it through the column were then labeled with antibodies against CD11c. A program that retains these cells on the magnetic column was then used to select for these cells. Since dendritic cells are CD11b- and CD11c+ the cells remaining were predominantly dendritic cells. 2.7 Splenic Dendritic Cell Isolation 2 A second method was used to isolate dendritic cells from spleens. Cells were first ground and digested with collagenase D as described in the first method. The digested suspension was then spun over a dense bovine serum albumin (BSA) gradient. The cells were suspended in the dense BSA and RPMI-1640 was layered on top. The gradient was then spun in a centrifuge at 900 RCF for 30 min. Cells were collected from the interface of the two liquids. Dendritic cells, being less dense than the BSA and denser than the RPMI-1640, collected at this interface. Many denser contaminating cells were pulled through the dense BSA. The enriched dendritic cell suspension was then further purified based on their property of transient plastic adherence. Cells were suspended in RPMI-5 media and plated on tissue culture plates. They were incubated for 90 min which allowed the dendritic cells to adhere. Contaminating non-adherent cells were then washed off. The medium was once again replaced with RPMI-5 media and put into an incubator overnight. After 12-20 h the dendritic cells became non-adherent and were gently washed off the plate, leaving other adherent contaminant cells behind. 8 2.8 Splenic T Cell Isolation T Cells were purified from the spleens of C57BL6 Thy 1.1 mice. Spleens were ground with microscope slides and the cells were labeled with magnetic beads. An AutoMACS cell sorter and Pan T isolation kit (Miltenyi Biotec) were used. Cells were labeled with an antibody cocktail consisting of CD11b, CD45R, DX5, and Ter-119 which were then conjugated to magnetic beads. CD11b mediates inflammation by regulating leukocyte adhesion, and is expressed by such cells as natural killer and macrophages. CD45R is signaling molecule expressed by various thymocytes. DX5 is a marker used to identify various subsets of NK cells, and Ter-119 is expressed by erythroids. T cells lack all of these markers so cells were passed through the AutoMACs column using negative selection in order to deplete them of the contaminating cells expressing these markers. This kept all contaminating cells on the columns and allowed the cells not expressing any of these markers (mostly T cells) to pass. Purity of the T cells was assessed by labeling them with CD4 and CD8 fluorescent antibodies and was determined to be greater than 90%. 2.9 Immunofluorescent Staining and Flow Cytometry Cells were stained with CD4, CD62L, and CD25. They were also stained with ethidium monoazide (EMA) to determine viability, and carboxyfluoroscein succinimidyl ester (CFSE) was used to assess T cell proliferation. EMA penetrates dead or dying cell membranes and stains DNA. Therefore, cells with EMA are determined to be dead and those without are viable (Fig 1). CFSE enters the cells, undergoes cleavage by esterases and is distributed evenly in the cytoplasm. Each time a cell divides the CFSE is distributed evenly among the two daughter cells. The amount of CFSE present in a cell is indicative of the extent to which it has divided (Fig 1). All T cells were labeled with CFSE before they were put into culture. 9 (B) Division R6 200 Number EMA 100 101 150 102 250 103 300 104 350 (A) Viability 0 -101 50 0 R3 0 200 400 600 800 FS -101 1000 (x 1000) 0 101 102 103 104 CFSE Figure 1. Example of flow cytometry histograms for viability and cell division assessment. (A) Forward Scatter (a measure of size) is on the X axis and EMA fluorescence intensity is on the Y axis. Cells stained with EMA are gated out, as is likely debris based on forward scatter (left). Viable cells are those in R3 (B) CFSE is on the X axis and number of events (cells) is on the Y axis. The majority of cells have not divided, and have retained their original CFSE (parent peak, right). Those that have divided (R6) lose half of their fluorescence intensity for each division they go through. CD4 was used to identify donor CD4+ T cells and CD8+ donor T cells. The flow cytometer used is limited to five colors per cell, and CD8 was eliminated in order to include the stain for CD62L. CD8+ T cells were identified as those stained with CFSE that were CD4- (Fig 2.). Since T cells are the only cells labeled with CFSE, those with CFSE and without CD4 must be CD8+ T cells. Listmode data was collected on a Beckman Coulter Cytomics FC500 flow cytometer. Data analysis including software compensation was carried out with Winlist software (Verity Software House). 103 104 R2 CD4 102 Figure 2. CD4 and CD8 T cell Gating. The X axis indicates level of CFSE intensity and the Y axis indicates level of CD4 expression. Those that are CD4 positive and are stained with CFSE (R2) are CD4 T cells. CD8 T cells are CFSE labeled and CD4 negative (R1) -101 0 101 R1 -101 0 101 102 CFSE 103 104 10 3.0 A Student’s T-test was used to determine statistical significance. P values less than 0.05 were considered statistically significant. 11 3. Results 3.1 T Cell Isolation T Cells were successfully isolated from spleens using the AutoMACs and Pan T Isolations Kit identified above. Purity was assessed each time and was consistently above 90%. Yields of ~15% of the spleen cells (approximately 1.2x107 per spleen) were achieved. 3.2 Dendritic Cell Isolation Three strategies were attempted to isolate dendritic cells. The first involved generation of these cells from progenitors in the bone marrow. Using this technique it was possible to isolate large amounts of high purity dendritic cells, although it required a lot of time. Two incubation steps and a total of nine days were required from the day the marrow was harvested to produce mature dendritic cells. These dendritic cells are also much less potent T cell activators. As a result, two additional strategies were attempted for isolation. The second method involved isolation of dendritic cells from spleen cells. This method employed a collagenase digestion, panning to remove B cell contaminants, and a run through the AutoMACs to select for cells that were CD11b- and CD11c+. Since dendritic cells are CD11b- and CD11c+ they should make up the majority of cells present at the end of the purification. The first problem encountered with this method was that the cells at the end of the purification were dead. All of the media was tested for the correct pH and determined to be within acceptable limits. After testing for viability with trypan blue before and after collagenase treatment, it was concluded that the cell were dying sometime during the 90 min incubation with collagenase. Steinman et. al recommended a 30-90 min incubation. As a result, an optimization experiment was performed in which spleens were digested for 30, 40, 50, and 60 min. Maximum recovery was achieved at 30 min, and cells began to die at some point between 40 and 50 min. It was determined that the 30 min time point would be the most suitable and it was used for all subsequent digestions. 12 The same procedure was attempted again, and cells remained viable throughout the entire purification. However, after the AutoMACs sorting steps, no cells were present. Dendritic cells make up a very small percentage of cells in the spleen, approximately 0.75% (3). This purification involved a large number of complicated steps, and it is likely that many dendritic cells could have been lost along the way, stuck on various plates and in the AutoMACs columns. The third method involved a different strategy of isolation of dendritic cells from spleens. It included the collagenase digestion as outlined previously. Dendritic cells were separated based on their density by the use of a BSA gradient. Finally, they were enriched even further through their property of transient adherence. This method has proven to be the best way to isolate these potent stimulators of T cell division. Yields of approximately 250,000 dendritic cells per spleen were achieved. 3.3 Dendritic Cell:T Cell Optimization Before experiments including TCDD treatment could be performed, the T cell to dendritic cell ratio that would provide optimal stimulation of T cells had to be determined. The best ratio will show clear divisions based on CFSE dilution as well as increased expression of CD25 with successive rounds of division. T cells were isolated from C57Bl/6 Thy 1.1 AhR heterozygous mice in the method previously outlined. Dendritic cells were isolated from the spleens of B6D2F1 following the method detailed in the second splenic isolation scheme. Cells were labeled with EMA, CFSE, CD4, CD8, and CD25. The cells were put into culture for 48 and 72 h at T cell:dendritic cell ratios of 300:1, 60:1, 30:1. These ratios and incubations times were based on previous work in our lab which indicated they would likely show the best division and CD25 expression. The 30:1 ratio proved to be the best to stimulate T cell division and CD25 expression and the 72 h incubation time proved to be the best for the same reasons (Fig 3). Splenic dendritic cells are much more potent activators of T cells than those derived from bone marrow. This was indicated from prior work in the lab as well. 13 104 (B) Dividing CD8s 30:1 Day 3 104 (A) Dividing CD8s 30:1 Day2 R7 R7 0 101 CD25 102 103 9% -101 -101 0 101 CD25 102 103 3.4% -101 0 101 102 103 104 CFSE ( -101 0 101 102 103 104 102 103 104 CFSE C (D) CD4s 30:1 Day 3 104 104 (C) CD4s 30:1 Day 2 R4 103 103 R4 8.4% -101 -101 0 0 101 101 CD25 CD25 102 102 3.9% -101 0 101 102 CFSE 103 104 -101 0 101 CFSE Figure 3. CFSE intensity is on the X axis and CD25 intensity is on the Y axis of all figures. (A) Only gated on CD8, clear divisions and increased CD25 expression (R7) with division is evident. (B) Only gated on CD8s, more distinct divisions are seen in this ratio, along with more CD25 expression (R7). (C) Only gated on CD4, little division and upregulatation of CD25 (R4) is apparent. (D) Only gated on CD4, clear divisions and increased CD25 expression (R4). 14 3.4 TCDD Experiment 1 CFSE labeled T cells were co-cultured with dendritic cells at a ratio of 30:1. Cultures with donor T cells from AhR+/+ mice received treatments of either 10-8 M, or 10-9 M TCDD or the vehicle treatment. The vehicle treatment consisted of DMSO in the same concentration given in the TCDD treatments. T cells from AhR -/- mice were also used, and these received either vehicle treatment or 10-8 M TCDD. All treatments were done in duplicate. Dendritic cells were not isolated in large enough number to allow a purity assessment, so it was assumed that the same level of purity had been reached as in a previous experiment to determine the ratio. After 72 h in culture, cells were harvested and stained for EMA (viability), CD4 (T helper cell), CD25 (IL-2 receptor), and CD62L (L-selectin). After collecting flow data for this experiment, it was found that no T cell proliferation had occurred (Fig 4). It is possible that this is due to inadequate stimulation resulting from too few dendritic cells. As previously mentioned, due to the lack of sufficient cells the presence and purity of dendritic cells was unable to be verified. (B) Normal Division 104 104 (A) No Division 103 103 R4 -101 -101 0 0 101 101 CD25 CD25 102 102 R5 -101 0 101 102 CFSE 103 104 -101 0 101 102 103 CFSE Figure 4. CFSE on the X axis and CD25 on the Y axis of both figures. (A) In this experiment, no division of T cells was seen, and only dividing cells upregulate CD25. (B) This figure is an example of expected division and upregulation of CD25 (R4). 104 15 3.5 TCDD Experiment 2 In the second experiment T cells were used only from AhR +/+ mice. Six treatments were used: TCDD concentrations of 10-8 M, 10-9M, 10-10M, and 10-11 M as well as vehicle and no vehicle. After 72 h in culture, cells were harvested and labeled with EMA, CD4, CD25, and CD62L. T cells were labeled with CFSE before going into culture. Higher yields of dendritic cells were realized, and as a result a 16:1 T cell:dendritic cell ratio was used in order to ensure stimulation and the resulting proliferation. Viability Figure 5. Cell viability at various TCDD concentrations. Percent viable cells is on the Y axis and molar TCDD concentration is on the X axis, error bars represent standard error. An asterisk (*) indicates p<0.05 n=3, comparing vehicle and each TCDD Treatment. There is no significant difference between the two controls. 35 Percent Viable 30 * 25 * * 20 15 10 5 0 `10^-8 `10^-9 `10^-10 `10^-11 Vehicle No Vehicle Molar Concentration TCDD CD4s Figure 6. CD25 expression of dividing CD4 T cells, CD 25 Median Channel Fluorescence (MCF) on Y axis, TCDD concentration on the X axis, error bars represent standard error. There does not appear to be any significant difference in CD25 expression resulting from TCDD treatment. Similar results were obtained for CD8 T cells. n=3 800 700 CD25 MCF 600 500 400 300 200 100 0 `10^-8 `10^-9 `10^-10 `10^-11 Molar Concentration TCDD Vehicle No Vehicle 16 (A) Dividing CD8s (B) Dividing CD4s Dividing CD8s Dividing CD4s 2.5 4.5 * 4 2 % Dividing CD4s % Dividing CD8s 3.5 3 2.5 2 * * 1.5 1 1.5 0.5 1 0.5 0 0 `10^-8 `10^-8 `10^-9 `10^-10 `10^-11 Vehicle `10^-9 `10^-10 `10^-11 Vehicle No Vehicle Molar Concentration TCDD No Vehicle Molar Concentration TCDD Figure 7. Dividing CD8s and CD4s, X Dividing Cells is on the Y axis and TCDD concentration is on the X axis. (A) Cells cultured in the two lower concentrations of TCDD did not appear to divide to the extent that others did. (B) There are significant differences in the extent of division in CD4s in the two highest concentrations. An asterisk (*) indicates p<0.05 n=3, comparing vehicle and each TCDD Treatment. There is no significant difference between the two controls. (A) CD8s (B) CD4s CD4s (CD62L Downregulating) 5 2 4.5 1.8 4 1.6 3.5 1.4 %Dividing CD4s %Dividing CD8s CD8s (CD62L Downregulating) 3 2.5 2 * * 1.2 1 0.8 1.5 0.6 1 0.4 0.5 0.2 0 0 `10^-8 `10^-9 `10^-10 `10^-11 Molar Concentration TCDD Vehicle No Vehicle `10^-8 `10^-9 `10^-10 `10^-11 Vehicle Molar Concentration TCDD Figure 8. Dividing CD8s and CD4s which downregulate CD62L. (A) Higher concentrations appear to cause a higher percentage of CD8 T cells to downregulate CD62L. (B) Here this trend is more evident, and significant. An asterisk (*) indicates p<0.05 n=3, comparing vehicle and each TCDD Treatment. There is no significant difference between the two controls. No Vehicle 17 There is no significant difference between vehicle and no-vehicle treatments in all variables reported. TCDD appears to have a significant effect on cell viability at three concentrations, although this is not likely to be biologically significant due to the lack of a trend (Fig. 5). TCDD does not appear to affect CD25 expression significantly, although there is a small trend of increasing CD25 expression with higher concentrations of TCDD (Fig. 6). There is a significant difference in the percentage of CD4+ T cells that divided when compared to the vehicle; they divided less than the vehicle (Fig. 7). There is a significantly higher percentage of CD4+T cells that downregulated CD62L at the two highest TCDD concentrations (Fig. 8) 18 4. Discussion Various strategies were attempted to isolate dendritic cells and ultimately the one involving a collagenase digestion of spleens followed by the BSA gradient and plastic adherence steps appeared to be the most effective and simple solution. Initially the 90 min collagenase digestion resulted in the death of all splenocytes. This could be attributed to either its enzyme activity or its presence as a solute. It seems most likely that its solute effects contribute to the creation of a hypertonic environment which would cause flow of water out of cells and lead to their dessication. The treatment was subsequently reduced to 30 min at which point the capsule was sufficiently broken up for increased recovery and cells remained viable. The BSA gradient was effective at removing all cells that had a higher density than dendritic cells such as red blood cells. After the BSA step, undesired T cell and macrophage contaminants were present but they were removed through the plastic adherence step. After plastic adherence, predominantly B cells and dendritic cells were present. B cells are of less concern than other contaminants as they also act as antigen presenting cells and are able to stimulate proliferation. Splenic dendritic cells have proven to be more potent stimulators than bone marrow derived dendritic cells, as was indicated by previous work in the lab. T cell to dendritic ratios of 30:1 were proven to effectively stimulate proliferation and differentiation. Earlier experiments demonstrated that many more bone marrow-derived dendritic cells were required to observe the same effect: effective ratios of around 5:1 were necessary. Since the number of dendritic cells required was smaller and the process to isolate dendritic cells from the spleen is a much faster process than maturing progenitors from the bone marrow, it was determined that the use of splenic cells was most desirable. No proliferation was observed in the first experiment in which some cultures were treated with various concentrations of TCDD. As previously stated, the purity of dendritic cells present was unable to be determined due to the lack of sufficient numbers for flow cytometry. It was assumed that they were the same as those present in the dendritic cell ratio optimization experiment. It seems likely that the T cells did not proliferate because they were provided insufficient stimulation. This would result from the purity of dendritic cells being much less than assumed. It is also possible that the number of cells the cell 19 counter indicated were present was incorrect. The counter used is not accurate at low cell concentrations and it is possible that error could come from this source. Since expression of CD25 requires proliferation and cells did not proliferate no upregulation of CD25 was seen. No CD62L was seen as it too requires proliferation for expression. More success was achieved in the second experiment involving TCDD. A large amount of proliferation was evident, possibly due to the use of the higher T cell to dendritic cell ration of 16:1 used to ensure that there would be sufficient stimulation. TCDD did appear to affect cellular viability although it is doubtful that this is a biologically significant effect, and it did not cause significant upregulation of CD25 beyond that of vehicle and no vehicle controls. A slight trend of increasing upregulation of CD25 was seen with increasing concentrations of TCDD but due to the large standard deviation of the vehicle control it was not significant. CD4+ T cells divided to a lesser extent in the two higher concentrations of TCDD. CD8+ T cells in the cultures with the two lower concentrations of TCDD (10-10M, and 10-11M ) did not appear to divide to the extent seen in other cultures. Changes in CD62L expression was observed among both CD4+ and CD8+ T cells. With increasing concentrations of TCDD more dividing CD4+T cells showed downregulation of CD62L. This is a promising result as CD62L downregulation also occurs with TCDD treatment in the graft versus host model. Due to limited time only one significant experiment including TCDD was able to be performed. This experiment should be performed several more times to ensure that the effects observed in this experiment were not merely due to chance as well as to ensure that other effects were not missed. This model appears to be suitable for continued research. Lack of increased upregulation of CD25 could indicate that Tregs are not present, although this may not be the case. There could be various reasons that Tregs do not appear to differentiate in vitro, even if TCDD does act directly on T cells as I have hypothesized. For instance, the AhR could induce a primary change in T cells that begins the process, but other cells are necessary to react to the change and get full Treg development. There are many cell types that could act to facilitate this that are not present in the in vitro model that was used. It could also be due to the fact that cell-to-cell orientations are crucial that are not recapitulated in vitro, or that the induction of other signals are not 20 optimized so they do not feed back correctly. Signals affecting Treg differentiation could also be diluted out in the culture media to the extent that they would not be effective. An exhaustive in vitro study would have to be performed in order definitively state that TCDD does or does not act directly on CD4+ T cells. If definitive TCDD effects can in fact be shown in vitro, the models used in such experiments could be used to screen other potential AhR ligands. If strong activators of the AhR can be found that are less toxic than TCDD they could have potential clinical applications in the treatment of autoimmune disease and the facilitation of organs transplants as mentioned previously. Current immunosuppressive therapies are global and passive, such as Cyclosporin A, and act broadly to suppress immune response by preventing T cell activation. If the immune response could be controlled actively through Tregs it would be possible to only turn off the immune response to a transplanted organ for instance, and avoid global suppression that results in susceptibility to disease. It was believed that TCDD acts directly on CD4+ T cells via the AhR to alter their differentiation. The research fell short on testing these TCDD effects on AhR dependency, and there is also insufficient evidence to determine if TCDD has a direct effect on CD4+ T cells. Further research is needed to reach a reasonable conclusion on both of these effects. 5. References 21 (1) Baccarelli A., A.C. Pesaori, S.A. Masten, D.G. Patterson Jr., L.L. Needham, P. Mocarelli, N.E. Caporaso, D. Consonni, J.A. Grassman, P.A. Bertazzi, M.T. Landi. 2004. Aryl-hydrocarbon Receptor-Dependent Pathway and Toxic Effects of TCDD in Humans: A Population-based study in Seveso, Italy. Toxicology Letters. 149:287-93 (2) Funatake, C.J., N.B. Marshall, L.B. Steppan, D.V. Mourich, N.I. Kerkvliet. 2005. Cutting Edge: Activation of the Aryl Hydrocarbon Receptor by 2,3,7,8Tetrachlorodibenzo-p-dioxin Generates a Population of CD4+CD25+ Cells with Characteristics of Regulatory T Cells. The Journal of Immunology. 175:41844188 (3) Inaba, K., W.J. Swiggard, R.M. Steinman, N. Romani, G. Schuler. 1998. Isolation of Dendritic Cells. Current Protocols In Immunology. 3.7.1-3.7.6 (4) Inaba, K., M. Inaba, N. Romani, H. Aya, M. Deguchi, S. Ikehara, S. Muramatsu, R. Steinman. 1992. Generation of Large Number of Dendritic Cells from Mouse Bone Marrow Cultures Supplemented with Granulocyte/Macrophage Colonystimulating Factor. Journal of Experimental Medicine. 176:1693-1702 (5) Kerkvliet, N.I., D.M. Shepherd, L.B. Steppan. 2002. T Lymphocytes are Direct, Aryl Hydrocarbon Receptor (AhR)-Dependent Targets of 2,3,7,8Tetrachlorodibenzo-p-dioxin (TCDD): AhR Expression in Both CD4+ and CD8+ T Cells is Necessary for Full Suppression of a Cytotoxic T Lymphocyte Response by TCDD. Toxicology and Applied Pharmacology. 185:146-152 (6) Vorderstrasse B.A., N.I. Kerkvliet. 2001. 2,3,7,8-Tetrachlorodibenzo-p-dioxin Affects the Number and Function of Murine Splenic Dendritic Cells and Their Expression of Accessory Molecules. Toxicology and Applied Pharmacology. 171:117-125 (7) Vremec, D., M. Zorbas, R. Scollay, D.J. Sanders, C.F. Ardavin, L. Wu, K. Shortman. 1992. The Surface Phenotype of Dendritic Cells Purified from Mouse Thymus and Spleen: Investigation of the CD8 Expression by a Subpopulation of Dendritic Cells. Journal of Experimental Medicine.176:47-58