* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Reading Guide-InnateImmune (CH15)
Lymphopoiesis wikipedia , lookup
Inflammation wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Adaptive immune system wikipedia , lookup
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
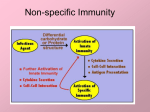
Reading Guide Innate Defense (CH15) The immune system is composed of two “branches”, the innate immune response and the specific immune response. This chapter focuses on the natural mechanisms at work to protect us from infections on a daily basis, the mechanisms that make up the innate immune response. This innate immune response consists of protective layers (such as the skin and mucus membranes), sensor systems in the body to detect the presence of invaders (such as toll-like receptors and complement proteins), and white blood cells (such as phagocytes and dendritic cells). Let’s take a closer look at some of the key concepts and ideas in this chapter. When you think about the components of the innate immune response, think of what a bacterial organism would need to do to enter into the body and cause disease. The first lines of defense (…think of the first structures that an organism must pass through to enter the body) are the skin and mucous membranes, and the antimicrobial secretions found in these areas. The skin is an amazing organ, made up of two layers, the epidermis and the dermis. The epidermis is where most of the “protective” mechanisms come into play with 20-30 layers of dead keratinized cells. The mucous membranes found in the interior regions of the body which open to the outside, such as the respiratory tract and digestive tract, are coated with secretions to continually wash the microbes from the surface. There are additional structures to help remove bacteria, the cilia in the respiratory tract, and peristalsis in the digestive tract. Many of the secretions found in these areas also have antimicrobial substances such as lysozyme, lactoferrin, and defensins. The normal microbiota also play a role at protecting the body from other bacterial organisms. These normal microbiota protect by competitive exclusion, making it hard for a new organism to grow and establish themselves in a particular environment. For example, E. coli produces toxins known as bacteriocins which kill closely related bacteria such as Salmonella and Shigella. Once an “invader” has made it past the first lines of defense, the next protective layer consists of cells, specifically the phagocytes. The two key types of phagocytes important in the innate response are the neutrophils and the macrophages. The neutrophils are considered the professional phagocytes, first to arrive at the scene of an infection and better at killing pathogens than macrophages. Not only do neutrophils have powerful granules but they can release the contents of their DNA along with the granules (remember these are a type of granulocyte) and trap bacteria in what is known as neutrophil enxtracellular traps (NETs). Macrophages are the second phagocyte to arrive at the scene of an infection. Good at cleaning up any cellular debris and eliminating any remaining bacteria. They are long lived and continually regenerate their lysosomes (the cellular structures that contain the digestive enzymes). These phagocytic cells are capable of phaogcytosis, a process in which the cell ingests the foreign cell/organism and destroys it. The key steps in the process of phagocytosis are outlined nicely on p 358, please review the steps and what happens at each step. One of the steps of phagocytosis is attachment, in order for a phagocytic cell to ingest something it has to BIND to it. I wanted to point out this step as it is critical to the entire process of phagocytosis. There are ways in which cells can bind directly (via receptors) and indirectly (via opsonization….a process that happens when complement proteins are activated). Some really virulent pathogens have evolved mechanism to evade the process of phagocytosis…can you think of some ways in which an organism could evade phaogcytosis? Cells of the immune system need to be connected and communicating with each other to coordinate complex responses. Communication between cells occurs through surface receptors, cytokines, and adhesion molecules. The surface receptors function to bind chemicals, such as cytokines, and the binding elicits a response by the cell. There are many different kinds of cytokines that are important in the innate immune response. Chemokines, for example, are important in chemotaxis and promote cell migration towards areas of inflammation. Review the function of the following kinds of cytokines, colony-stimulating factors, interferons, interleukins, and tumor necrosis factor. There are sensor systems that help detect the presence of foreign invaders and set in motion either other cells or a specific response. Toll-like receptors (TLRs) are really cool receptors that allow cells to “see” molecules that signify the presence of microbes. These receptors are found on many different kinds of cells and when bound by such parts of microbes as peptidoglycan, flagella, or LPS, they activate gene expression. LPS bound to TLR on macrophages asctivates the cell to produce chemokines that attract additional macrophages to the area. How cool to have a mechanism to alert the cell that an invader is present and produce a chemical to attract other phagocyte cells. The complement system consists of a collection of interacting proteins that are found in the blood and tissue fluids. They circulate in these body spaces in an “inactivated” form and are activated in a cascade-type fashion. The most important aspects of the complement system (for our discussion) is to recognize how the proteins are activated and the three different outcomes that occur when these proteins are activated. There are three main pathways to activate the complement system, the alternative pathway, the lectin pathway, and the classical pathway. The alternative pathway of activation occurs when protein C3b binds to cell surfaces and promotes the formation of an activation complex. The lectin pathway requires the binding of mannose-binding lectins to mannose to activate the complement proteins. The classical pathway of activation requires the presence of antibodies bound to antigen, this binding activates the complement proteins. Once the complement proteins are activated there are three things that happen, the targeted cell may lyse (this is a good thing if the targeted cell is a pathogen), inflammation occurs (again a good response, think of what happens in the process of inflammation), and opsonization occurs. Opsonization is necessary when a phagocyte tries to ingest an organism with a capsule. The capsule layer makes it hard for the phagocyte to “grab on” or bind to the pathogen…remember I said that one of the key steps in phagocytosis is binding..! Once the complement proteins are activated, one of them (C3b) can bind to the surface of the target cell. This binding of C3b promotes phagocytosis of the cell by phagocytes such as macrophages. The last group of sensor molecules are the interferons produced by body cells in response to the presence of long dsRNA molecules in a cell. Long dsRNA is not part of the host cell and often an indication that the cell is infected with a virus. Alpha and beta interferon are produced by the host cell infected with the virus (or the cell that has the dsRNA molecules). These proteins bind to neighboring cells and activate these cells to produce antiviral proteins. The antiviral proteins induce cellular suicide (apoptosis) if the neighboring cell is infected with the virus. This is a nice mechanism to target only cells that are infected with the virus for destruction and limit the ability of the virus to replicate. The last mechanisms to discuss in this chapter important in the innate response are inflammation and fever. Inflammation is an important process set in motion by cellular damage and the release of cytokines. There are four characteristic symptoms of inflammation and they are; redness, heat, pain, and swelling. The process of inflammation begins when pro-inflammatory cytokines promote the blood vessels to dilate, shunting the blood flow to the damaged area. The blood vessels also become leaky or more permeable, promoting the loss of fluid from the vessels into the tissue space. The loss of fluid also allows the flow of blood to slow down so that the neutrophils can attach to receptors on the inside of the blood vessel wall and migrate into the tissue space. This is called diapedesis. Once at the site of the infection the neutrophils ingest bacterial and other ell debris. Macrophages arrive later to ingest any remaining pathogens and clean up cellular debris so that the healing process can begin. See if you can determine the cause of each of the symptoms of inflammation. The fever response is also a key mechanism indicating a bacterial infection. How many times have you been sick and the physician will ask if you have a fever? There are pro-inflammatory cytokines that can cause a fever response and are also called pyrogens. Remember the LPS layer of gram negative cell walls can also promote a fever response in the body. A fever response helps with the immune response because it makes it harder for bacteria to scavenge iron, increases the rate of cellular reactions and hopefully promotes more “activated” cells, and the increase in temperature makes it harder for organisms to grow. We will use some of the key ideas in this chapter to build on the ideas in the next chapter on the specific immune response. Begin to think about the innate immune response mechanisms that can protect you against a bacterial infection….or even a viral infection.