* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Type IV hypersensitivity
Complement system wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Immune system wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Adaptive immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
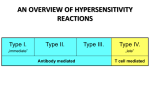
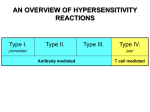
Type II Cytotoxic hypersensitivity • Reaction time is minutes to hours • mediated by antibodies of IgM or IgG • class and complement Phagocytes and NK cells may also play a role • (ADCC). Diagnostic tests include detection of • circulating antibody against tissues involved and the presence of antibody and complement in the lesion (biopsy) by immunofluorescence Directed against cell surface or tissue antigen • Clinical Examples • • • • • • • • • • • • Transfusion reactions Autoimmune Hemolytic anemia Hemolytic disease of newborn Drug induced hemolytic anemia Autoimmune thrombocytopenia Pemphigus vulgaris(desmoglein ) Goodpastures syndrome Myasthenia gravis Graves disease Insulin resistant diabetes Pernicious anemia others Drugs that can cause this type of hemolytic anemia include: • • • • • • Cephalosporins (a class of antibiotics) Levodopa Methyldopa Penicillin and its derivatives Quinidine Some nonsteroidal anti-inflammatory drugs (NSAIDs) Type III • The reaction may be general (e.g., serum sickness) or may involve individual organs including skin ( Arthus reaction), kidneys, lungs, blood vessels , joints or other organs. Type III • It is mediated by soluble immune complexes • The reaction may take few hours after exposure to the antigen • The lesion contains primarily neutrophils Immune complex mediated diseases • Immune complexes cause disease only: 1-in excessive amounts 2- not efficiently cleared 3- become deposited in tissues a) intermediate complexes tend to be deposited in vessels b) Cationic antigens bind to negatively charged components of the basement membranes of blood vessels and glomeruli,joints Tissue injury mechanisms • Antibodies may opsonize cells or activate the complement system Production of complement proteins that opsonize cells. These cells are phagocytosed and destroyed by phagocytes that express FcR and CR Main mechanism in autoimmune hemolytic anemia and thrombocytopenia and hemolysis in transfusion reactions. Cell Mediated Immunity • The effector cells involved in these processes are cytotoxic T-lymphocytes (CTLs), NK-cells and Th cells Phagocytosis and killing of intracellular pathogens Direct cell killing by cytotoxic T cells Direct cell killing by NK and K cells • These responses are especially important for destroying intracellular bacteria, eliminating viral infections and destroying tumor cells • Response to microbes residing within the phagosomes is mediated by effector CD4 Th1 cells • Microbes that infect and replicate in nonphagocytic cells,is mediated by CD8 • T cell dependent macrophage activation and inflammation may damage normal tissues • • • • Th1(IFN- ) Th2(IL-4,IL-5) Th17(TGF-,IL-1,IL-6) The most differentiation –inducing stimuli are IFN- ,IL-12 and IL-4 Killing by cytotoxic T cells • release some substances known as perforin ,Granzyme A,B ,C and serglycin and granulysin • the CTL may release lymphokines and/or cytokines • • • • • Recognition Activation Lethal hit Release(cathepsin B) Type IV hypersensitivity Type IV hypersensitivity • DTH (Delayed type hyper sensitivity) • Is a T cell mediated inflammatory response ,in which stimulation of T cells leads to macrophage activation and localised inflammation and edema within tissues. • This effector T cell response is essential for the control of intracellular and other pathogens. • If the response is excessive it can damage host tissues • Subsequent exposure of the sensitised individual to the exogenous Ag results in the recruitment of specific T cells to the site and development of a local inflammatory response over 24-72 hrs. Interferon production TDTH formation variants of type IV HS There are 3 variants of type IV HS reaction • Contact HS • Tuberculin type HS • Granulomatous HS Contact hypersensitivity • Occur within 72 hrs of Ag challenge • Characterized by an eczematous reaction in the skin at the point of contact with an allergen • Organic chemicals and inorganic metals such as nickel , chromate and rubber accelerator in latex gloves Contact hypersensitivity Has 2 stage • Sensitization • elicitation TUBERCULIN TYPE • Is induced by soluble antigens from organisms such as M.Tuberculosis and Leprae and leishmania tropica • Following ID tuberculin challenge memory T cells are recruited and activated to secrete IFN- ,which activates Macrophages to produce TNF and IL-1 • The initial influx at 4 hrs is neutrophils but replaced at 12 hrs by monocytes and T cells. PPD skin test Granulomatous HS • Clinically the most important form of type IV HS. • If the Ag persist(intracellular micro.,other particles such as ziconium and beryllium ,talc ,silica) ,chronic activation of T cells and macrophages lead to granuloma formation and tissue damage. Granulomatous HS The Granuloma contains : • Epithelioid cells (secret TNF) • Langhans giant cells(low ER and degeneration of lysosomes and mitochondria) • Macrophages IFN- and TNF are essential for granuloma formation Granulomatous HS • Crohn disease(chronic inflammatory disease of ileum and colon) • Leishmaniasis • Sarcoidosis • Leprosy • tuberculosis