* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Type II Hypersensitivity: Antibody mediated cytotoxicity
Lymphopoiesis wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Complement system wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Autoimmunity wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Molecular mimicry wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
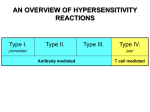
Type II Hypersensitivity: Antibody-mediated cytotoxicity • Results when Ig or IgM bind to cell surface Ag’s – Activating Complement – Binding Fc receptors on Tc cells promoting ADCC • Both processes result in lysis of the Ab-coated cell • Clinical examples of Type II responses include: – Certain autoimmune diseases where Ab’s produced vs membrane Ag’s • Grave’s Disease – Ab’s produced vs thyroid hormone receptor • Myasthenia Gravis – Ab’s produced vs acetylcholine recpetors • Autoimmune hemolytic anemia – Ab’s produced vs RBC membrane Ag’s – Hemolytic Disease of the Newborn – Hyperacute graft rejection • Blood Transfusion rxns • Graft rejection Type II Hypersensitivity: Transfusion reactions • Produced by mismatched blood types – Destroys foreign RBC by complementmediated lysis triggered by IgG • Produces fever, intravascular clots, lower back pain, Hgb in urine – Free Hgb produced has 2 fates: • passes to the kidneys – hemoglobinuria • Breaks down to bilirubin..can be toxic Type II Hypersensitivity: Hemolytic Disease of the Newborn • Occurs via maternal IgG Ab’s crossing the placenta • In severe cases causes erythroblastosis fetalis – Most commonly develops in Rh- mother with Rh+ fetus – Exposure to Rh+ fetal RBC’s stimualtes prod of memory/plasma – Activation of memory cells in subsequent pregnancy stim IgG Ab’s which can cross the placenta – mild-severe hemolytic anemia ensues along with bilirubin which affects the brain/CNS • Treatment centers on anti-Rh antibodies (Rhogam) • Mothers can be tested for anti-Rh antibodies to check for a rise in titre • Isolated fetal RBC’s can be checked for anti-Rh IgG w/ Coombs test Hemolytic Disease of the Newborn Type II Hypersensitivity: Drug-induced hemolytic anemia • Drugs such as aspirin and antibiotics can bind to the surfaces of RBC’s • These interactions act similar to hapten-carrier conj. • Such complexes can trigger Ab-mediated cell lysis by complement activation Type III Hypersensitivity: Immune Complex-mediated cytotoxicity • Caused by immune complex deposition in tissues – Small amts cleared by phagocytic cells – Activates complement which attracts neutrophils and stim Mast cell degranulation – Depending on location, rxn can be localized or systemic • Most damage stems from activity of Neutrophils – Immune complexes can adhere to tissue making it difficult for Neutrophils to phagocytize – Neutrophils continue releasing lytic enzymes, etc. Type III Hypersensitivity: Localized reactions • Arthus rxns: – Exposure to an Ag for which there already is a high [c] of Ab – Produces edema/erythema from damage to bv and tiss • Insect bites • Inhalation of bacteria, fungi, dried fecal matter Type III Hypersensitivity: Systemic (generalized) reactions • Produced when large amounts of Ag enter the bloodstream – The sites of deposition vary; usually in tissues where plasma is filtered – Esp. in kidneys, blood vessels, and joints • Can cause tissue damaging rxns: • Serum sickness • Autoimmune diseases • Drug reactions • Infectious diseases Type IV Hypersensitivity: Delayed-Type Hypersensitivity • Occurs 48-72 hrs after Ag contact and is mediated by Ag-specific TH1 cells and activated MØ • TH1 cells secrete: – IFN-γ activates MØ – TNF-α and β upregulate CAM’s on local b.v’s – Il-3 and GM-CSF stim bone marrow monocyte output Initial contact with Ag (sensitization) may induce memory TH1 cells without symptoms Phases of the DTH Response • Sensitization – TH1 cells triggered by contact with APC • Effector response – produces huge influx of activated MØ – Activated MØ is more efficient at antigen-presentation – Release of lytic enzymes lead to non-specific destruction of cells – Works well vs intra-cellular pathogens – If pathogen/particle lingers -> can lead to granuloma formation • Ex: Mycobacterial pathogens in TB and Leprosy DTH Response Cytokines released include: TNF-β, GM-CSF, and IFN – γ DTH Response Type IV rxns marked by time delay and recruitment of MØ instead of Neut’s and Eosino’s Contact Dermatitis Produced by a variety of substances Mostly small molecules attach to a protein in the skin The Ag-protein complex is processed and presented sensitize TH1 cells Subsequent exposure activates TH1 cells 48-72 hrs later MØ infiltrate Activation of MØ causes the inflammation that characterizes the disorder