* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Lab Dx Day 1 Intro to Hematopoietic System
Adaptive immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Innate immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
X-linked severe combined immunodeficiency wikipedia , lookup
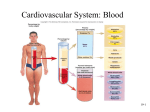
Intro to Hematopoietic System Dr. Melanie Osterhouse 1040 – blood/immune Function of blood components ___ - oxygen transportation (by hemoglobin) ___ - mobile elements of the body’s defense system ____ - cell fragments important for blood clotting Blood Components Organization of Total blood volume Blood componenets plasma 55% (91% water) WBC (Leukocyte) Largest Cellular 45% RBC (erythrocyte) Middle Platelet (thrombocyte) Smallest Volume of Blood __ L of blood circulating 1/3 of body weight RBC lifetime = ____ days RBCs are the heaviest resulting in the bottom layer after centrifuging Buffy coat - WBC and platelets - layer above RBCs Plasma - on top after centrifuging Erythrokinetics Kidney stimulates erythropoietin response to low oxygen Bone Marrow RBC production Lung Oxygenation Tissues supplied with oxygen and nutrients Spleen (and liver) destroys old RBCs Marrow Production All bones - 0-5years of age Pelvis (40%), vertebrae (28%), cranium/mandible (13%), ribs (8%), sternum (2%) - 20+ years of age Red marrow = _____ yellow marrow = _______ Overview of ________ number of blood cells in the blood stream depends on three factors: Rate of production Rate of release Length of survival Embryogenesis _______________________ 3rd gestational week - stem cells in yolk sac 3rd gestational month - liver becomes site blood cell formation, with the help of spleen, lymph nodes, and thymus 4th gestational month - bone marrow becomes functional Location of cell line __________ - central marrow __________ - osteoid/marrow junction _____________ (discharge platelets) - line sinusoids directly into blood stream Pluripotential stem cell terminolgy stem cell Stem Cell Lymphoid LIne erythroid Non-lymphoid line (myeloid) granulocyte megakaryocyte monocyte/macrophage Erythropoesis maturation process Unipotential StemCell (bone marrow) Erythroblasts 6 days Reticulocytes (from marrow to blood) 1day:1day Erthrocytes 120 days Three mechanisms to increase erythrocytes: Increase number of stem cells decrease maturation time release ________into the bloodstream earlier _________ Due to oxygen demand, erythropoetin stimulates hastening of RBC maturation and early release of reticulocytes into the bloodstream ___________ Young RBCs with extruded nucleus but maintaining lots of RNA Normal reticulocyte count is 1% with an average half-life of 4.8 hours Reticulocytes The RNA is responsible for producing _______.(RNA is not in mature RBCs) Reticulocyte produces 30% of total hemoglobin The other 70% is made in the pre-reticulocyte stages Reticulocytes have ________ receptors Transferrin carries iron to hemoglobin-producing immature erythrocytes Mature RBCs don’t have the receptors due to their inability to synthesize hemoglobin Reticulocytes VS mature RBC RNA and ribosomes Loss or RNA and transferrin receptors ribosomes Loss of transferrin receptors No more hemoglobin synthesis (carries previously made Hb from reticulocyte stage) bringing iron via transferrin hemoglobin synthesis ____ – depression _________ - elevation Polycytosis – increase in RBCs Polycytopenia – decrease in RBCs Break down of leukocytes WBC leukocyte (WBC) agranulocyte (mononuclear leukocyte) Lymphocyte monocyte granculocyte (polymorphonuclear leukocyte) neutorophil basophil eosinophil WBC 5-10,000 = normal range granulocytes are called polymorphonuclear due to the multilobed nucleus leukocytes live ______ days, destroyed by lymphatic system and excreted in feces Function = ____________ phagocytosis produce, transport and distribute antibodies WBC Differential count = number of different types of leukocytes ________ = WBC>10,000 severe leukocytosis in: •leukemia •leukemoid reaction = temporary –seen in measles, pertussis, sepsis _________ = WBC<4000 Seen in: infection bone marrow disorders hypersplenism IDA __________ - avoid infection avoid contamination by fresh fruits and veggies WBC panic values (<500 or >30,000) WBC value variables ___________ - low in morning and high in late afternoon Newborn normal (1020,000) and gradually decreases until age 21 Differential WBC count ________ -> pyogenic infections _________ -> allergic disorders and parasitic infection ________-> parasitic infections _________ -> viral infecion __________- -> severe infections by phagocytosis Summary of Immune System Immune proteins are the most diverse proteins known. Immune system required to survive infection Antibodies-aka ___________ vast number of antibodies made by re-shuffling a small set of gene fragments Immune system The other immune proteins are ___ receptors recognizes only cells that have self and nonself markers. Lymphocytes lymphocytes Origin =bone marrow B cells maturation=bone marrow memory cell plasma cell antibodies immunoglobulins T cells maturation complete in thymus gland cytotoxic T cells Helper T cells suppressor T cells _ cell line Antibodies mark foreign organisms for destruction Complement system responds to this mark by perforating the cell membrane. Antigen-antibody complexes attract macrophages to engulf and digest foreign particles B cell line Diversity in B cells comes from combinational and mutational mechanisms Diversity increases the number of distinct antigen binding sites T cell line ________ T cell =kill target directly ________T cell=recognize antigen and stimulate B and T cells ______ T cell=opposite helper T cell. ______________ (MHC) The third class of proteins in immune system (B and T cells and MHC) MHC - found on all cell surfaces T cells require recognition of both antigen and a self MHC protein MHC causes T cells to be attracted to infected cells not free bacteria (to prevent replication of infection) __________ Smooth discs enclosed in a plasma membrane. Two types of granules inside: 1.alpha containing fibrinogen 2. electron dense bodies-storage site for ADP/ATP, Ca, histamine, serotonin, epinephrine With injury to a vessel, platelets undergo three reactions: ______- - attachment of platelets to sites of endothelial cell injury __________-- release of platelet granules – ADP induces platelet aggregation Platelet ___________ – Thromboxane released by platelets causing aggregation and vasoconstriction ____________ platelet contraction - fused mass stimulated by the combination of ADP, thrombin, and thromboxane Thrombin causes fibrinogen to convert to fibrin within the platelet aggregate making “platelet bricks” Platelet sequence sequence of events endothelial injury recognized by platelets platelets secrete granules synthesize thromboxane A2 activation of extrinsic coagulation sequence due to release of tissue factor from injured cells ADP stimulates aggregated platelets sequence of events endothelial injury recognized by platelets platelets secrete granules synthesize thromboxane A2 activation of extrinsic coagulation sequence due to release of tissue factor from injured cells ADP stimulates aggregated platelets platelet brick formed due to deposition of fibrin platelet brick formed due to deposition of fibrin Coagulation sequence transformation of proenzymes to activated enzymes via intrinsic and extrinsic pathway resulting in thrombin formation _________ occurs on the surface of activated platelets ____________ = reduced platelets (normal 150,000300,000/mm3) spontaneous bleeding occurs below 20,000/mm3 of platelets. Post-traumatic bleeding results in platelets in the range of 20,00050,000/mm3 Thrombocytopenia causes small vessel bleeding m/cly. M/C sites: skin mucous membranes of GI and GU Intracranial bleeding Thrombocytopenia - etiology Decreased platelet production – marrow dz • aplastic anemia • leukemia – drug/ alcohol – AIDS • antiplatelet antibodies due to molecular mimicry – megaloblastic anemia • ineffective megakaryopoiesis Decreased platelet survival – autoimmune dz (SLE) – drug – Infection Sequestration – hypersplenism Dilutional mechanical injury – prosthetic heart valve Dilutional ________ - blood stored for longer than 24 hours has virtually no viable platelets Defective platelet function _____ has antiplatelet effect and is thus used in Tx of recurrent MI DIC - _______________ secondary thrombohemorrhagic disorder Ch. by activation of the coagulation sequence leading to diffuse formation of microthromi endothelial injury - major trigger M/Cly seen in obstetric complications, malignancy, sepsis, and major trauma – malignancies include leukemiaa, CA of lung, pancreas, colon, stomach • tumors releasing thromboplastic substances DIC deposition of fibrin within microcirculation – causes _____-due to the squeezing of RBCs through the narrowed microcirculation – ischemic organs bleeding – due to consumption of platelets and clotting factors and plasminogen DIC ________are found in decreasing order: – brain, heart, lung, kidney, adrenals, spleen, liver 50% of DIC is from complications of ________ (such as toxemia) – reverses with delivery of fetus Signs/Symptoms of DIC Respiratory – dyspnea, cyanosis, distress Neurologic – convulsions, coma Renal – oliguria, acute failure Circulation – shock Acute DIC from trauma or obstetric tends to be bleeding dominant Chromic DIC from cancer tends to be thrombotic dominant DIC Tx Depends on if bleeding or thrombosis predominates anticoagulants like heparin coagulants like fresh-frozen plasma Sometimes platelet transfusion Specific anemic states Dr. Melanie Osterhouse Logan College of Chiropractic ____________ Decrease in the red cells caused by too little iron most common anemia 20%women, 50%pregnancy,3%men Risk factors for IDA Women who menstruate pregnancy or lactation children in rapid growth phases low dietary intake (no meat or egg) Blood loss (peptic ulcer dz, aspirin, colon CA, uterine CA, blood donation IDA symptoms Pallor fatigue irritability weakness SOB low BP sore tongue brittle nails pica decreased apetite headache ___________ Failure of blood cell forming capacity in marrow affecting all blood cell types Causes Aplastic Anemia Chemotherapy/ congenital drugs radiation toxins pregnancy disorders SLE infectious hepatitis idiopathic Aplastic anemia symptoms Fatigue pallor SOB tachycardia arrhythmia rash bruising/bleeding Signs Enlarged spleen tender sternum low Hb and hematocrit low retic low platelet abnormal marrow biopsy Tx Bone marrow transplant transfusions prognosis is death without treatment Complications Infection cerebral hemorrhage bleeding Causes of ____________ Alcohol abuse Liver dz (defective folate or B12 def DNA synthesis with accelerated erythropoiesis) bone marrow disorders hypothyroidism chemotherapy/drugs hemolysis/bleeding macrocytosis results from: Erythropoietin-mediated acceleration of erythrocyte production, cell wall synthesis defects and aberrant responses to erythropoietin stimulation symptoms Anorexia Headache diarrhea glossitis paresthesia jaundice pallor fatigue __________ causes polyneuropathy, myelopathy and altered mental state due to: Damage in the dorsal and lateral columns of the spinal cord signs Abnormal reflexes decreased proprioception and vibration low hematocrit with high MCV low B12 Elevated ferritin Tx of B12 def Intramuscular B12 injections Normal hematology in 2 months Neurological compromise can be permanent