* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download No Slide Title
Immune system wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Adaptive immune system wikipedia , lookup
Anaphylaxis wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Innate immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
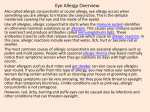
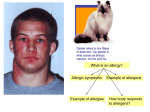
Allergic Disease Dr Garry M. Walsh, School of Medicine, University of Aberdeen Atopy • The predisposition to produce high quantities of Immunoglobulin (Ig)-E • Immediate (Type I hypersensitivity) • Mast cells, basophils, eosinophils, Th2 cells Allergy • Allergic Disease is mediated by IgE • First described by Prausnitz & Kustner in 1921 • Proposed the existence of “atopic reagin” in serum of allergic subjects • 45 years later Ishizaka described a new class of immunoglobulin - IgE Allergic Disease • • • • • • Seen in 30-35% of the population Perennial & seasonal allergic rhinitis Allergic (extrinsic asthma) Atopic and contact dermatitis Urticaria Food intolerance Allergy • Elevated IgE levels seen in allergy and parasitic infection • Binds to mast cells and basophils • Often specific for harmless environmental factors - allergens IgE Allergen Mast Cell Crosslinking Histamine release Allergic rhinitis • Seasonal (pollen, spores) or perennial (house dust mite) • Mucus production (Runny nose, nasal stuffiness • Itching & sneezing • Treat with antihistamines or nasal steroids Urticaria • • • • • • Wheal and flare Itching Allergen-induced Idiopathic – pressure, cold etc. Food – shellfish, strawberries, peanuts Treat with antihistamines Atopic dermatitis • Allergen –induced particularly milk protein from the gut enters blood stream –deposited in skin – mast cell degranulation • Exfoliating eczema and itching • Treat with antihistamines • May progress to asthma Anaphylaxis • • • • Very acute and severe reaction to allergen Peanuts, shellfish, penicillin, insect stings Allergen moves from gut to blood stream Massive histamine release from mast cells and basophils • Vasodilatation leads to dramatic drop in blood pressure • Often fatal if not treated with adrenaline Allergens • Environmental substances • Usually benign • Sub-group of individuals exhibit a hypersensitivity reaction (type 1) Allergens Mite faeces (digestive enzymes) Pollen Animal dander (cats) Insect stings Food Allergy Inflammation Beneficial Harmful Removal of insult Persistence or constant exposure RESOLUTION HYPERSENSITIVITY Allergy – an inappropriate immune response Allergy – an inappropriate immune response Allergy – an inappropriate immune response • Parasite larvae – proteases • House dust mite – faeces (skin) – proteases • Pollen – proteases • Cat saliva - proteases IgE Allergen Mast Cell Crosslinking Histamine release Mast cells and basophils Mast Cell Mast cells Release pre-formed mediators (histamine) and lipids together with several TH2 cytokines IgE • Very low serum concentration – 0.00005 mg/ml) • Sensitises mast cells and basophils by binding via Fc portion to high affinity receptor – FceR1 • Serum half life of a few days • Binding protects IgE from destruction by serum proteases • Sensitisation can last for many months • Detected by skin prick test or radio absorbant test (RAST) Skin prick test Allergic Inflammation • Much more complex than histamine release • Involvement of a whole host of cells, cytokines, chemokines and mediators Granule proteins MBP, ECP, EPO Cytokines IL-3, IL-4, IL-5 GM-CSF, IL-6 IL-12, TGF-b Epithelial damage/loss Muscarinic M2 dysfunction/ AHR Attract/activate eosinophils Airway remodelling, IgE, Th2 polarisation LTC4, PAF Chemokines Eotaxin, RANTES Mucus hypersecretion Airway narrowing Attract/activate pro-inflammatory cells Attract/activate eosinophils Mast Cells Mediators: histamine, prostaglandins, PAF, LTC4 & LTD4 Mucosal oedema, vasodilation, mucus secretion, bronchial smooth muscle contraction Mast Cells Cytokines (e.g. IL-4, IL-5, TNFa, IL-8): LTB4, PAF Attract and activate neutrophils & eosinophils Connective tissue Mast Cell Mucosal Mast Cell Gut & lung Ubiquitous T cell dependent Long lived >40 days Short lived <40 days 3x104 IgE receptors 25x105 IgE receptors High histamine content Lower histamine content Heparin & high tryptase Chondroitin sulphate Lower tryptase Histamine • • • • Skin – wheal, erythema, pruritis Eye - conjunctivitis, erythema, pruritis Nose – nasal discharge, sneeze, pruritis Lung – bronchospasm of smooth muscle Histamine • Therapeutic intervention in allergy often focused on blocking the effects of histamine • Histamine also functions as a neurotransmitter in CNS • Very important in maintaining a state of arousal or awareness First Generation Antihistamines • The first H1 antagonist synthesised by Bovet & Staub at the Institut Pasteur • Too weak or toxic • Phenbezamine first effective antihistamine • Mepyramine maleate, diphenhydramine & tripelennamine developed in 1940’s • Still in use today First Generation Antihistamines • Easily cross the blood–brain barrier. • Sedative and anticholinergic effects (sedating antihistamines). • Short half-lives. • Limited use in the treatment of allergic symptoms. • Still widely used, mainly as over-the-counter products, often in combination with other drugs. Second Generation Antihistamines • • • • • Highly effective treatments for allergic disease Do not cross blood-brain barrier Lack significant CNS & anticholinergic effects Long half life Among the most frequently prescribed and safest drugs - expensive Other treatments • Nasal steroids – must be given before season – relieve nasal blockade • Antihistamines combined with antileukotriene drugs • Avoidance -mattress covers, specialised Hoovers, wood floors, Allergic Disease • Dramatic increase in allergic disease over the past three decades, why is this? • Genetics • Environmental factors - pollution • Changes in Lifestyle • Occupational Genetics (1) • Family history of allergic disease is a strong risk factor for developing asthma • Danger of developing asthma particularly if one or both parents are atopic • Children with atopic dermatitis at risk of asthma -– “the allergic march” Genetics (2) • No single "allergy or asthma chromosome". Several markers demonstrated in small selected populations - much further work is required • The genetics of allergy and asthma are polygenic - influence many factors such as IgE secretion, cytokines and inflammatory cell profiles Environment (1) • Children & adults 90% spent time indoors • Allergens in dust (dust mite faeces) or pets (particularly cats) - increased risk of allergic sensitization in proportion to exposure. • Most children and adolescents with asthma sensitized to indoor allergens - avoidance often leads to improvement in airway disease. • Modern housing generally poorly ventilated with fitted carpets and central heating - house dust mite infestation Environment (2) • Children exposed to tobacco smoke more likely to develop wheezing and impaired lung function • Outdoor allergens –seasonal variation and weather • Account for 10-20% of allergic disease in Europe mainly hay fever. • Increased pollution not responsible for increase in allergic disease - pollutants worsen respiratory symptoms in asthmatics and reduce lung function Changes in Lifestyle (1) • Hygiene hypothesis - Past 30 years - changes in pattern of childhood infection, many no longer experienced • Exposure to certain infections may protect against the development of allergies. • Respiratory viruses may be a risk factor for the development of asthma • Vaccination programmes not thought to have direct effect on the development of allergic disease Changes in Lifestyle (2) • Intake of fresh fruit and vegetables has declined leading to lower anti-oxidant levels. • Certain fatty acids are able to shift the immune system towards allergic susceptibility • Food preservatives may effect gut flora leading to allergic sensitization rather than development of tolerance Changes in Lifestyle (3) • The immune system is severely compromised by poor nutrition • Paradoxically the vast improvement in nutrition in the last fifty years might have led to the immune systems of some individuals "over reacting" to benign substances i.e. allergens Conclusion • Atopy – propensity to produce high levels of IgE from B cells • Allergens mimic parasites – processed and presented by APC (e.g. dendritic cells) • Orchestrated by Th2 cells – cytokine release • Effector cells – mast cells, basophils • Mediators – cytokines, histamine, leukotrienes, PAF etc.