* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Medically Unexplained Physical Symptoms
Treatments for combat-related PTSD wikipedia , lookup
Obsessive–compulsive personality disorder wikipedia , lookup
Gender dysphoria in children wikipedia , lookup
Sluggish cognitive tempo wikipedia , lookup
Memory disorder wikipedia , lookup
Autism spectrum wikipedia , lookup
Eating disorder wikipedia , lookup
Anxiety disorder wikipedia , lookup
Broken windows theory wikipedia , lookup
Causes of mental disorders wikipedia , lookup
Major depressive disorder wikipedia , lookup
Rumination syndrome wikipedia , lookup
Social anxiety disorder wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Mental disorder wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Excoriation disorder wikipedia , lookup
Bipolar disorder wikipedia , lookup
Separation anxiety disorder wikipedia , lookup
Panic disorder wikipedia , lookup
Child psychopathology wikipedia , lookup
Antisocial personality disorder wikipedia , lookup
Asperger syndrome wikipedia , lookup
Spectrum disorder wikipedia , lookup
Schizoaffective disorder wikipedia , lookup
History of mental disorders wikipedia , lookup
Depersonalization disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Conduct disorder wikipedia , lookup
Factitious disorder imposed on another wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Diagnosis of Asperger syndrome wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Narcissistic personality disorder wikipedia , lookup
Treatment of bipolar disorder wikipedia , lookup
Munchausen by Internet wikipedia , lookup
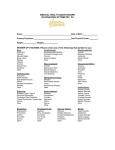
Medically Unexplained Physical Symptoms for GP trainees Dr Sarah Burlinson Consultant in Liaison Psychiatry Royal Oldham Hospital Pennine Care NHS Trust Aims Appreciate how common these are Increase assessment skills Recognise associated psychiatric diagnoses Strategies to manage in primary care Simple scenarios Complex patients List 8 common physical symptoms which are often medically unexplained? Common Medically Unexplained Symptoms Pain Fatigue Dizziness Headache Ankle swelling Breathlessness Insomnia Numbness What % of these are found to have a medical cause when followed up for 1 year? 76%-100% 51%-75% 25%-50% 0-24% These common symptoms….. At 1 year: only 10-15% due to organic cause (Katon 1998) Prompt < 50% of primary care consultations 10% of patients with ‘MUS’ diagnosed with organic disease at 18 months FU (Morriss 2007) How common are MUS in NP in Primary Care? 76%-100% 51%-75% 25%-50% 0-24% Are they more or less common in Secondary Care OP clinics? How common are MUS? Primary Care 20% of new GP consultations 1/3 of these persist Secondary Care 25-50% of new medical out-patients Chronic MUPS/ somatisation disorder 0.5-4 % community prevalence Impact of MUS Patients Psychological Physical Social Staff Frustration/ demoralisation ‘Heart sink’ patient Resources Investigations/ admissions/clinics/medication Possible mechanisms Autonomic arousal Muscular tension Hyperventilation Hyper-vigilance Mood disorder De-conditioning Predisposing/ precipitating & maintaining factors Female Parental ill-health/ childhood adversity Life events Past/ current psychiatric illness Health care response Secondary gain Name 6 psychiatric disorders which are associated with or which cause MUS. Associated Psychiatric Disorders Anxiety/ depressive illness Somatoform disorders Somatisation disorder Somatoform pain disorder Hypochondriacal disorder Dissociative disorder (Hysteria) Factitious disorder (Munchausen’s) Delusional disorder Substance misuse Detecting Depression in MUPS HOPELESS HELPLESS WORTHLESS Pervasive low mood Lack of enjoyment Poor concentration Irritability Guilty feelings Sleep disturbance Poor appetite Diurnal variation Low libido Reduced energy Anxiety: Physical Symptoms Palpitations Dizziness ‘Butterflies’ Nausea Tremor Tingling Dry mouth Wanting the toilet Muscle tension Hyperventilation Chest pain Lump in throat Somatisation Disorder >2 years multiple and variable medically unexplained physical symptoms Preoccupation & distress Repeated consultations Refusal to accept medical reassurance > 6 from a list Undifferentiated SD & Somatoform Pain Disorder Hypochondriacal disorder Persistent belief of the presence of a serious disease Preoccupation/ distress/ disability Refusal to accept medical reassurance Dissociative Disorder (Hysteria) Sudden loss of function Temporal link with stressful event/ situation No medical explanation Delusional Disorder Single or set of related delusions Hallucinations/ thought disorder rare Relatively well functioning Themes include Hypochondriacal Erotomanic Persecutory Factitious Disorder Intentional feigning of symptoms Aim is to receive medical care Often marked personality disorder & interpersonal difficulties (Malingering- different motive e.g: Financial Avoid court/ conscription) Management Case note review Clinical assessment and Ix Will simple explanation work? Is this depression/ anxiety? Is there another psychiatric disorder? Management Reattribution Acknowledging reality of symptoms Feeling understood Making the link Antidepressant May reduce symptoms even if not depressed Psychotherapy Cognitive behaviour therapy Psychodynamic interpersonal therapy Management of Chronic Somatisation Regular fixed intervals Bio-psychosocial approach Reduce drugs Treat mood disorder Limit referrals / investigations Reduce expectation of cure Summary MUS: common and treatable associated with mood disorders Mild/ recent onset: Reattribution techniques Antidepressants/ psychotherapy Chronic (somatisation disorder): Complex/ time consuming Clear management plan Resources http://www.rcpsych.ac.uk/expertadvi ce/problems/medicallyunexplainedsym ptoms.aspx http://www.neurosymptoms.org/