* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Heart
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Artificial heart valve wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
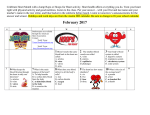
Chapter 15 Cardiovascular System Cardiovascular System • • • • Provides O2 & nutrients to all tissues Removes CO2 & wastes Consists of heart & b.v. The heart is a 4 chambered, hollow, muscular organ • Avg. size: 9 cm wide, 14 cm long Location • Located in the mediastinum, resting on the diaphragm • Base – top of heart beneath 2nd rib • Apex – point at bottom (points toward left) at 5th intercostal space • Bordered by lungs laterally & sternum anteriorly Coverings 1. Fibrous pericardium – tough, outer layer 2. Parietal pericardium – inner lining of pericardial cavity Pericardial cavity – space filled w/serous fluid; reduces friction 3. Visceral pericardium – membrane that covers the heart (same as epicardium) Coverings Fibrous pericardium→ Fibrous pericardium Visceral pericardium Layers of Heart Wall 1. Epicardium – same as vis. pericardium; thin connective tissue; protection & secretes fluid 2. Myocardium – thick; consists of cardiac muscle; contracts to pump blood 3. Endocardium – epithelial & connective tissue; lines all chambers & valves; helps keep surfaces smooth Heart – External Features • Auricle – ext. flaps • Sulci – grooves for b.v. • During an avg. lifetime, the heart beats approx. 2.5 billion times • It pumps an avg. of approx. 300 million L of blood Internal Anatomy • The heart has been described as 2 pumps that lie side by side • The 2 sides of the heart are separated by a wall called the septum • The 2 thinner-walled upper chambers that receive blood are called atria • The 2 thicker-walled bottom chambers that pump blood are called ventricles Internal Anatomy • The atria are separated from the ventricles by valves • Valves prevent the backflow of blood • Tricuspid – on rt. • Bicuspid (mitral) on left • Rt. side of heart receives deoxy. blood from body & pumps it to the lungs to get oxygenated (colored blue) • Left side receives oxygenated blood from lungs & pumps it to body (colored red) Heart Valves • 2 types: 1. Atrioventricular valves (A-V valves) – located between the 2 atria & ventricles: tricuspid & bicuspid (mitral) 2. Semilunar valves (S-L valves) – located in the b.v. leading away from the heart: pulmonary & aortic Chordae Tendinae • In the right and left ventricle chordae tendinae are strong fibers attached to the A-V valves. • They prevent the valve from extending into the atrium chamber. • Attached to papillary muscles. Heart Sounds • Produced by the closing of the heart valves • A typical heartbeat is heard as “lub-dup” • A-V sounds: • Mitral – heard at 5thintercostal space • Tricuspid – at tip of sternum • S-L sounds: • Aortic – at 2nd intercostal space on rt. • Pulmonary – 2nd intercostal space on left Blood Supply to the Heart (anterior view) • The left & rt. coronary arteries branch off the aorta to supply blood to the heart itself • The l.c. art. branches into circumflex & left ant. descending artery (or left interventricular artery) Blood Supply to the Heart (anterior view) • The rt. coronary artery branches into the marginal artery & the posterior interventricular artery (on posterior view – next slide) Coronary Circulation Blood Supply to the Heart • Blood leaves arteries & passes through capillaries of the myocardium • Blood then passes into cardiac veins • Cardiac veins empty into coronary sinus (lg. vein on post. side of heart) • Coronary sinus empties into rt. atrium Cardiac Conduction System • The heart has its own pacemaker that can initiate a heartbeat; called the sinoatrial node (S-A node) • Located in the upper rt.atrium; causes both atria to contract almost simultaneously Cardiac Conduction System • Impulse travels to the atrioventricular node (A-V) located in the interatrial septum • Impulse then moves to A-V bundle (or bundle of His) & then to bundle branches • Purkinje fibers carry impulse to distant parts of ventricles The Cardiac Cycle • A series of contractions & relaxations that constitute one heartbeat • Atria contract while ventricles relax & vice versa • Diastole – relaxation of a heart chamber • Systole – contraction of a heart chamber Electrocardiograms (EKGs) • Measures electrical activity of the heart • Results from depolarization & repolarization of the myocardium • 12 electrodes are placed on various places on the body • Changes can indicate arrhythmias & other heart-related conditions Parts of an EKG • P wave – contraction of the atria • QRS complex – contraction of ventricles • T wave – relaxation of ventricles • Relaxation of atria (repolarization) – not seen (hidden by QRS complex) EKG Measurements • P wave to P wave 1 complete ♥ beat • P-Q interval – time it takes impulse to travel from S-A node to A-V node EKG Measurements • Q-T interval - the period from the beginning of ventricular depolarization until the end of ventricular repolarization • The QT interval is prolonged if it clearly measures more than half the R-R interval • Called long QT syndrome Abnormal EKGs • Long QT syndrome Bundle Branch Block • The QRS complex is the time required to depolarize the ventricles. • A normal QRS is 0.08-0.12 s • > than 0.12 seconds is considered a BBB (block in a bundle branche, or the electrical impulse was conducted abnormally) Arrhythmias • Normally the ♥ contracts about 60-100 times/min • Each contraction represents one ♥ beat • Abnormal ♥ rates & EKGs – called arrhythmias Arrhythmias Sinus rhythm → 60-80 beats/min • • Tachycardia > 100 beats/min Bradycardia < 60 beats/min Arrhythmias • Atrial Flutter – many more P waves compared to QRS complexes • Atrial Fibrillation – P waves absent Arrhythmias • Junctional Rhythm – S-A node nonfunctional; P waves absent; heart being paced by A-V node (40-60 beats/min) • Ventricular Fibrillation – Chaotic depolarization of ventricles; extremely irreg. as seen in heart attack, elec. shock Blood Pressure • Pulse – alternate expansion & relaxation of arteries • Pulse pressure – difference b/t systolic & diastolic pressure • Central venous pressure – pressure in rt. atrium Factors That Affect B.P.BP An incr. in any of these causes an incr. in BP: 1. Heart Action – Cardiac Output (CO) = Vol. of blood discharged from the ventricles/min. – Stroke Volume (SV) = Vol. of blood discharged w/each contraction (approx. 70 ml at rest) – Heart Rate (HR) = number of beats/min – CO = SV X HR – CO = 70 ml X 70 beats/min – CO = 4900 ml/min Factors That Affect B.P.P 2. Blood Volume = sum of formed elements + plasma (usually 5L); (ex. - hemorrhage results in drop in B.P.) 3. Peripheral Resistance – force produced from the friction on blood from b.v. walls (expansion or dilation of b.v. changes resistance) 4. Viscosity = ease w/which blood flows (an incr. of RBCs incr. viscosity; anemia or hemorrhage decr. it) Blood Pressure • Force blood exerts against inner walls of b.v. (usually arteries) • Avg. = 120/80 • Measured w/a sphygmomanometer • 120 = systolic – maximum pressure during ventr. contraction • 80 = diastolic – lowest pressure during ventr. relaxation Measurement of BP Blood Vessels • Include arteries, veins & capillaries • Arteries & veins have 3 layers: 1. tunica intima – single layer squamous cells; secretes substances to stem blood flow 2. tunica media – makes up most of the b.v.; mostly smooth muscle & some connective tissue; allows for expansion 3. tunica externa – connective tissue; provides attachment to surrounding tissue Blood Vessels • 2 differences b/t arteries & veins: 1. thickness of tunica media 2. veins have valves Capillaries • Smallest b.v.; connect arterioles to venules • Resp. gases & other substances are exchanged in capillaries thru diffusion Capillary Bed Movement In Capillaries • Water & other substances leave capillaries at the arteriolar end b/c of a net outward pressure • Water & other substances leave at venular end b/c of a net inward pressure Movement in Capillaries Capillaries • Arrangement of capillaries control permeability of substances • In spleen, liver & red marrow, capillaries have large openings b/t cells; allow large subst. to diffuse • Blood-brain barrier – tight arrangement of capillaries around brain; few substances pass thru; protects brain