* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chronic Mitral Regurgitation
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Marfan syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Artificial heart valve wikipedia , lookup
Infective endocarditis wikipedia , lookup
Rheumatic fever wikipedia , lookup
Cardiac surgery wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
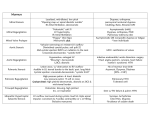
二尖瓣及主动脉瓣疾病的诊断与治疗 浙江大学医学院附属第一医院 张芙荣 Valvular heart disease • • • • MITRAL STENOSIS AORTIC STENOSIS MITRAL REGURGITATION -Acute and Chronic AORTIC REGURGITATION -Acute and Chronic • • • • TRICUSPID REGURGITATION TRICUSPID STENOSIS PULMONARY STENOSIS PULMONARY REGURGITATION • MIXED LESIONS 病因和流行病学 • 病因:风湿性疾病,退行性疾病,感染性疾病,炎症性疾 病,新型瓣膜病(如AIDS,药源性以及遗传性) • 流行病学: Bernard Iunga*, A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. European Heart Journal (2003) 24, 1231–1243 总 病人评估: 论 诊断 ↓ 严重程度评估 ↓ 预后评估 ↓ 干预指征 Strategy for Evaluating Heart Murmurs Bonow, R. O. et al. J Am Coll Cardiol 2008;52:e1-e142 Cardiac murmurs • Cardiac murmurs are often the first sign of underlying valvular disease. • May be systolic or diastolic, pathological or benign. • Systolic murmurs may be due to physiological increases in blood velocity or might indicate as yet asymptomatic cardiac disease. • Diastolic murmurs are usually pathological and require further evaluation. • ECG and CXR are readily available, but provide limited information. 临床评估 • 症状分析 • 体征:杂音 • 超声心动图 KEY TO DIAGNOSIS与患者临床情况相结合 评估内容: 所有瓣膜及升主动脉、房室大小和功能 狭窄性瓣膜病:瓣膜开口面积,平均压差,最大流速 返流性瓣膜病:ERO TEE:血栓形成,人工瓣膜功能障碍,感染性心内膜炎,手术 结果监测 3D超声:解剖结构评估 临床评估 • X线→钙化评估 • 放射核素造影→窦律下EF值评估(返流性VHD) • 负荷试验→ 负荷ECG:潜在症状,AS风险分层 负荷超声心动图:返流量改变的评估 • CT→钙化评估,CTA可排除CAD • MRI→作为超声的替代,对某些指标较精确 • 生化指标→BNP CAG:术前排除CAD • 心导管:非侵入性检查不理想时可考虑 Mitral Stenosis Mitral Stenosis Etiology Rheumatic (nearly all adult MS) other etiologies are very rare: Degenerative (Mitral valve annular calcification,elderly) Congenital (parachute MV), MS+atrial septal defect=Lutembacher syndrome. Others: post-inflammatory, metabolic syndromes , Other causes of LV inflow obstr.,atrial myxoma, LA ball thrombus, cor triatriatum. etc. MITRAL STENOSIS-Pathology Fusion of the comissures, cusps or chords. Contracture and thickening of the cusps. Shortening and fusion of the chordae tendinae. Funnel –shaped orifice. Posterior cusp Mitral annulus Anterior cusp Chordae tendinae Papillary muscles Mitral Stenosis Overview • Definition: Obstruction of LV inflow that prevents proper filling during diastole • Normal MV Area: 4-6 cm2 • Transmitral gradients and symptoms begin at areas less than 2 cm2 • Rheumatic carditis is the predominant cause • Prevalence and incidence: decreasing due to a reduction of rheumatic heart disease. Pathophysiology • • • • • • • • Obstruction between LA and LV. Pressure gradient. Elevated LA pressure. LA pressure increases at elevated HR. Pulmonary vascular resistance elevated. Pulmonary hypertension Right ventricular hypertrophy, enlargement. Systemic venous congestion. Mitral stenosis-Classification s √ Mitral Stenosis Clinical Presentations Asymptomatic symptomatic Dyspnea, PND, Orthopnea Hemoptysis – usually pulmonary venous hypertension -rupture of alveolar capillaries. -pulmonary infarction. -ruptured of dilated bronchial veins. -chronic bronchitis. Signs of right-sided heart failure: in advanced disease Atrial fibrillation Systemic embolization Mitral Stenosis Diagnosis • Clinical - and P2 (pulmonary hypertension) - Low-pitched mid diastolic rumble - Opening snap (OS)开瓣音and Loud S1 indicating pliable leaflets - short OS-S2 interval indicates severe MS -Mitral facies -other auscultatory signs as per co-existing disease ECG - P mitrale: broad, notched P wave in II and biphasic in V1 - RVH and rightward axis if significant PHT Mitral Stenosis Diagnosis • CXR - LAA and LA enlargement - increased upper lobe vascularity - Kerley B and A lines - dilated PA - MV calcification •ECHO: The GOLD STANDARD for diagnosis. Asses mitral valve mobility, gradient and mitral valve area MS echo Mitral stenosis- complications • Atrial fibrillation/flutter. • Embolism: Systemic:cerebral, coronary, preipheral; • Acute pulmonary edema. • RV heart failure. • Infective endocarditis. • pulmonary infection. Mitral Stenosis Management Principles • Asymptomatic - no specific therapy - endocarditis prophylaxis - if appropriate, rheumatic fever prophylaxis • Mild and Mod MS ( MVA > 1.5 sq cm and 1.0 to 1.4 sq cm) - Normal physical activity - No specific therapy, restoration of NSR in case of AFib - restoration of NSR and anticoagulation in case of Afib - intervention if PASP > 60 mm of Hg or exertional symptoms Simultaneous LV and LA pressure tracing Mitral Stenosis Management Principles • Severe MS - is usually symptomatic - Percutaneous mitral commissurotomy (PMC) is the treatment modality of choice in the vast majority - PMC in optimal anatomy has acturial survival rate of 95% after 7 years - PMC in skilled centers has a mortality of < 1% - Success of PMC depends on the pre-PMC valve anatomy - Commissural calcification is a predictor of suboptimal outcome - Complications: severe MR, embolization and cardiac perforation Mitral Stenosis Management Principles • Surgical treatment - commissurotomy (only occasionally indicated, usually PMC) - valve replacement √ Aortic Stenosis Aortic Stenosis Etiology • Most common surgical valve disease in the developed world • Degenerative/calcification - most common cause in the industrialized world - under 70 years of age ~ 70 % bicuspid and ~ 15 % tricuspid - over 70 years of age, >50 % tricuspid and ~ 25 % bicuspid • Rheumatic - most common cause in the developing world - almost always associated with MV disease • Other - associated with other congenital cardiac abnormalities (Co-arctation, VSD, Hypoplastic left heart, etc.,,) Pathophysiology of Aortic Stenosis • A pressure gradient develops between the left ventricle and the aorta. (increased afterload) • LV function initially maintained by compensatory pressure hypertrophy • When compensatory mechanisms exhausted, LV function declines. Pathophysiology of aortic stenosis Aortic stenosis LV outflow obstruction LV systolic pressure Aortic pressure LV hypertrophy LV dysfunction Myocardial ischaemia LV failure Aortic Stenosis Overview: • • Normal Aortic Valve Area: 3-4 cm2 Symptoms: Occur when valve area is 1/4th of normal area. • Types: – Supravalvular – Subvalvular – Valvular Aortic Stenosis Diagnosis • Clinical -pulsus parvus et tardus细迟脉 (absent in hypertensives and elderly) -Reduced systolic and pulse pressure - systolic thrill and typical heaving apical impulse - S4 and late peaking ejection systolic murmur - paradoxical split of 2nd HS in severe AS - other auscultatory signs modified by co-existing disease Syncope: (exertional) Angina: (increased myocardial oxygen demand; demand/supply mismatch) Dyspnea: on exertion due to heart failure (systolic and diastolic) Sudden death Aortic Stenosis Diagnosis •ECG - LVH with strain, conduction abnormalities • CXR - dilated ascending aorta (post-stenotic dilatation) - Valve calcification Aortic Stenosis Diagnosis • Echo (primary diagnostic modality) - AV anatomy (tricuspid, bicuspid, calcification) - Mild Vs. Moderate Vs. Severe AS - AVA and gradients can be calculated - progression of disease can be monitored - assessment of LV function and coexisting lesions • Cath - ususally done to assess coronaries prior to valve surgery - helpful to assess severity in complex situations Evaluation of AS 常以左心室-主动脉收缩期压差判断狭窄程度,平均压差 >50mmHg或峰压差≥70mmHg为重度狭窄 Cardiac catheterization: Should only be done for a direct measurement if symptom severity and echo severity don’t match OR prior to replacement when replacement is planned. Aortic Stenosis Management Principles • Asymptomatic - no specific therapy - endocarditis prophylaxis - if appropriate, rheumatic fever prophylaxis • Mild and Mod AS ( AVA > 1.5 sq cm and 1.0 to 1.4 sq cm) - Normal physical activity - No specific therapy, restoration of NSR in case of AFib - approx. progression is a decrease by 0.1 sq cm per year - annual echo follow-up Aortic Stenosis Management Principles General- IE prophylaxis in dental procedures with a prosthetic AV or history of endocarditis. Medical - limited role since AS is a mechanical problem. Vasodilators are relatively contraindicated in severe AS Aortic Balloon Valvotomy- shows little benefit. Surgical Replacement: Definitive treatment Aortic Stenosis Management Principles • Severe AS - usually symptomatic within 2 years - asymptomatic severe AS : no surgery - asymptomatic severe AS: exercise symptoms=?surgery - symptomatic severe AS: surgery - symptomatic severe AS if not operated has an average life expectancy of 2 to 3 years - severe AS with HF has mortality of nearly 100% in 1 to 2 years if not operated Management Strategy for Patients With Severe Aortic Stenosis Bonow, R. O. et al. J Am Coll Cardiol 2008;52:e1-e142 Mitral Regurgitation Acute MR Etiology • Endocarditis • Acute MI • Malfunction or disruption of prosthetic valve Management of Acute MR • Myocardial infarction: Cardiac cath or thrombolytics • Most other cases of mitral regurgitation is afterload reduction: – Diuretics and nitrates – nitroprusside, even in the setting of a normal blood pressure. Treatment of Acute MR • Balloon Pump • Nitroprusside even if hypotensive • Emergent Surgery Chronic Mitral Regurgitation • • Definition: Backflow of blood from the LV to the LA during systole Mild (physiological) MR is seen in 80% of normal individuals. Chronic Mitral Regurgitation Etiology • • • • Myxomatous degeneration (MVP) Ischemic MR Rheumatic heart disease Infective Endocarditis Pathophysiology of MR • Pure Volume Overload • Compensatory Mechanisms: Left atrial enlargement, LVH and increased contractility – Progressive left atrial dilation and right ventricular dysfunction due to pulmonary hypertension. – Progressive left ventricular volume overload leads to dilation and progressive heart failure. Chronic Mitral Regurgitation •Clinical • Auscultation: soft S1 and a holosystolic murmur at the apex radiating to the axilla – S3 (CHF/LA overload) – In chronic MR, the intensity of the murmur does correlate with the severity. • Exertion Dyspnea: ( exercise intolerance) • Heart Failure: May coincide with increased hemodynamic burden e.g., pregnancy, infection or atrial fibrillation The Natural History of MR • Compensatory phase: 10-15 years • Patients with asymptomatic severe MR have a 5%/year mortality rate • Once the patient’s EF becomes <60% and/or becomes symptomatic, mortality rises sharply • Mortality: From progressive dyspnea and heart failure Chronic Mitral Regurgitation Diagnosis • ECG: May show, LA enlargement, atrial fibrillation and LV hypertrophy with severe MR • CXR: LA enlargement, central pulmonary artery enlargement. • ECHO: Estimation of LA, LV size and function. Valve structure assessment – TEE if transthoracic echo is inconclusive √ Management of MR • Medications Vasodilator such as hydralazine Rate control for atrial fibrillation with blockers, CCB, digoxin Anticoagulation in atrial fibrillation and flutter Diuretics for fluid overload Management of MR • • Serial Echocardiography: – Mild: 2-3 years – Moderate: 1-2 years – Severe: 6-12 months IE prophylaxis: Patients with prosthetic valves or a Hx of IE for dental procedures. Management Strategy for Patients With Chronic Severe Mitral Regurgitation Bonow, R. O. et al. J Am Coll Cardiol 2008;52:e1-e142 Mitral Valve Prolapse Types • Women 20 to 50 years • Low BP, orthostatic hypotension, palpitations, chest pain • Mid systolic click, maybe mid systolic murmur • Echo: - thickened, redundant leaflets - leaflet excursion (prolapse) into LA in systole - redundant chordae tendinae, trivial or mild MR • Little progression of MR, Abx prophylaxis Mitral Valve Prolapse Types • Men 40 to 70 years • Myxomatous and thickened MV • Significant leaflelt prolapse • Significant MR, progressive MR • Complications: Chordal rupture, Afib • Endocarditis prophylaxis • Surgery for MR often required Classic or non-classic combined MVP equal in male and females. More complications in MEN Transthoracic echocardiographic image in parasternal long-axis view, showing posterior mitral leaflet bowing backward and prolapsing into left atrium during systole. LV=left ventricle. LA=left atrium. PML=posterior mitral valve leaflet. Aortic Regurgitation Aortic Regurgitation Overview • Definition: Leakage of blood into LV during diastole due to ineffective coaptation of the aortic cusps Etiology of Acute AR • Endocarditis • Aortic Dissection • Physical Findings: – Wide pulse pressure – Diastolic murmur – Florid pulmonary edema Treatment of Acute AR • True Surgical Emergency • Positive inotrope: (eg, dopamine, dobutamine) • Vasodilators: (eg, nitroprusside) • Avoid beta-blockers • Do not even consider a balloon pump Etiology of Chronic AR • Aortic leaflet disease Bicuspid aortic valve Rheumatic Infective endocarditis • Aortic root disease Aortic aneurysm/dissection Marfan’s syndrome Connective tissue disorders Syphilis HTN Annulo-aortic ectasia Pathophysiology of AR • Combined pressure AND volume overload • Compensatory Mechanisms: LV dilation, LVH. Progressive dilation leads to heart failure Pathophysiology of aortic regurgitation Aortic regurgitation LV volume stroke volume LV mass systolic BP LV dysfunction diastolic BP myocardial ischaemia LV failure Natural History of AR • Asymptomatic until 4th or 5th decade • Rate of Progression: 4-6% per year • Progressive Symptoms include: - Dyspnea: exertional, orthopnea, and paroxsymal nocturnal dyspnea - Nocturnal angina: due to slowing of heart rate and reduction of diastolic blood pressure - Palpitations: due to increased force of contraction Physical Exam findings of AR • Wide pulse pressure: most sensitive • Hyperdynamic and displaced apical impulse • Auscultation– Diastolic blowing murmur at the left sternal border – Austin flint murmur (apex): Regurgitant jet impinges on anterior MVL causing it to vibrate – Systolic ejection murmur: due to increased flow across the aortic valve 水冲脉 Duroziez征 股动脉枪击音 毛细血管搏动 点头征 The Evaluation of AR • CXR: enlarged cardiac silhouette and aortic root enlargement • ECHO: Evaluation of the AV and aortic root with measurements of LV dimensions and function (cornerstone for decision making and follow up evaluation) • Aortography: Used to confirm the severity of disease Example of a Jet of Aortic Regurgitation, as Shown by Color-Flow Imaging Enriquez-Sarano, M. et al. N Engl J Med 2004;351:1539-1546 Management of AR • • • • • General: IE prophylaxis in dental procedures with a prosthetic AV or history of endocarditis. Medical: Vasodilators (ACEI’s), dihydropyridine calcium channel blocker improve stroke volume and reduce regurgitation only if pt symptomatic or HTN. Serial Echocardiograms: to monitor progression. Surgical Treatment: Definitive Tx Percutaneous aortic valve implantation Management Strategy for Patients With Chronic Severe Aortic Regurgitation Bonow, R. O. et al. J Am Coll Cardiol 2008;52:e1-e142 THANK YOU