* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Depression
Mental health professional wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Substance use disorder wikipedia , lookup
Mental status examination wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Mental disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Abnormal psychology wikipedia , lookup
Emergency psychiatry wikipedia , lookup
History of psychiatry wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
History of mental disorders wikipedia , lookup
Child psychopathology wikipedia , lookup
Causes of mental disorders wikipedia , lookup
Postpartum depression wikipedia , lookup
Major depressive disorder wikipedia , lookup
Biology of depression wikipedia , lookup
Behavioral theories of depression wikipedia , lookup
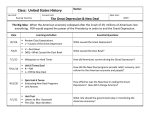
Depression Purdue University Calumet Counseling Center Gyte 05 219 989 2366 Counseling Center Webpage Who does it impact? The National Institute for Mental Health estimates that in the U.S., 16 million adults had at least one major depressive episode in 2012. That is 6.9% of the population According to the World Health Organization (WHO), 350 million people worldwide suffer from depression. Depression is the leading cause of disability. What are the symptoms? Depressed mood (feeling sad or empty) most of the day, nearly every day Loss of pleasure in activities once enjoyed Significant weight loss or weight gain (change of more than 5% body weight in a month) Insomnia (trouble sleeping) or hypersomnia (sleeping too much) Symptoms Psychomotor agitation (physical and emotional responses sped up) or retardation (physical and emotional responses slowed down) Fatigue or loss of energy Feeling worthless or excessive/inappropriate guilt Diminished ability to think or concentrate, or indecisiveness Recurrent thoughts of death, suicidal ideation, suicide attempts, or having a plan for suicide. Emotional Symptoms extreme irritability over minor things anxiety and restlessness anger management issues loss of interest in favorite activities fixation on the past or on things that have gone wrong thoughts of death or suicide Physical Symptoms insomnia or sleeping too much debilitating fatigue increased or decreased appetite weight gain or weight loss difficulty concentrating or making decisions unexplained aches and pains Symptoms In children, depression may cause clinginess and refusal to go to school. Teens may be excessively negative and begin avoiding friends and activities. Depression may be difficult to spot in older adults. Unexplained memory loss, sleep problems, or withdrawal may be signs of depression. Others may notice depression if you: -Consistently making negative statements about themselves -Withdrawing from social involvement -Increasing in irritability or angry outbursts -Losing interest in sexual activity -Begin complaining of frequent headaches, stomachaches, or muscle pain Who does it affect? Over 50% of university students report feeling depressed at some point since their freshman year of college 15% of college students meet the criteria for clinical depression Women are twice as likely to experience depression as men (though this may be related to gender differences in the way sadness is expressed) Causes and Risk Factors There is no single cause of depression. Brain chemistry, hormones, and genetics may all play a role. Other risk factors for depression include: low self-esteem anxiety disorder, borderline personality disorder, post-traumatic stress disorder (PTSD) physical or sexual abuse Causes and Risk Factors chronic diseases like diabetes, multiple sclerosis, or cancer alcohol or drug abuse certain prescription medications family history of depression Related Symptoms Anxiety Substance abuse Common Myths Depression is not a real medical problem. -Extensive research has indicated genuine biological and genetic factors that contribute to the development of depression, not just psychological factors. Depression can be changed by “positive thinking” if a person is strong enough. -Depression is not something people can “snap out of” with positive thinking, as research shows that it can change brain structure and alter thoughts and perceptions. Common Myths cont. Depression will go away on its own. -Without treatment, depression can last for months, years, or worse: it can result in suicide, the 3rd leading cause of death for Americans between 18-24. Depression only results from traumatic events, such as the death of a loved one. - Sometimes, painful events in life can bring about a depressive episode, but for many people it occurs when everything in life seems to be going smoothly. How can you know? If you, or someone you know has symptoms of depression, take it seriously. Make an appointment with a doctor if symptoms last more than a few weeks. It’s important to report all symptoms. A physical examination and blood tests can rule out health problems that can contribute to depression. Depression Screening website: Completely anonymous and confidential Does not provide a clinical diagnosis, but can give you some idea of whether you (or someone you care about) should seek professional help What makes depression worse? Ignoring the problem, denying the problem, or waiting for it to go away Alcohol Drugs Social isolation from friends and family Poor diet Poor sleeping habits/schedule Treatment Depression help Treatment is treatable with professional can include antidepressant medication and psychological counseling. Complications Prolonged or chronic depression can have a devastating impact on your emotional and physical health. Untreated, it may even put your life at risk. Depression can lead to: alcohol or drug abuse headaches and other chronic aches and pains phobias, panic disorders, anxiety attacks trouble with school or work family and relationship problems social isolation overweight or obesity due to eating disorders, raising the risk of heart disease and type 2 diabetes self-mutilation attempted suicide or suicide What can you do? Seek professional help (counseling center, mental health center) Many places offer free to low-cost therapeutic services Seek support groups (community, online, friends, family) Talk about it (with family, friends, community) Accept that the problem exists Stay active Limit alcohol consumption Increase social activity Eat a balanced diet, and don’t skip meals Seek mindfulness classes (can be found free online) Help is Available: Seek professional help. Contact PUC Counseling Center at 219 989 2366 or come to the office at Gyte 05 Contact PUC Student Health Service Center at 219 989 1235 or come to the office at Gyte Annex 34 References American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: Author. Fava M, Cassano P. Mood disorders: Major depressive disorder and dysthymic disorder. In: Stern TA, Rosenbaum JF, Fava M, Biederman J, Rauch SL, eds. Massachusette General Hospital Comprehensive Clinical Psychiatry. 1st ed. Philadelphia, Pa: Mosby Elsevier; 2008:chap 29. Pietrangelo, A. (2015). Depression and Mental Health by the numbers: Facts, statistics, and you. Healthline.com Kessler, R. C., McGonagle, K. A., Zhao, S., Nelson, C. B., Hughes, M., Eshleman, S., Wittchen, H.U., & Kendler, K.S. (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry, 51, 8-19 References (continued) Furr, Susan R.; Westefeld, John S.; McConnell, Gaye N.; Jenkins, J. Marshall (2001). Professional Psychology: Research and Practice, 32, 97-100. National Institute of Mental Health (NIMH) Nolen-Hoeksema, S., Larson, J., & Grayson, C. (1999). Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology, 77, 1061-1072