* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Survey
Document related concepts
Cellular differentiation wikipedia , lookup
List of types of proteins wikipedia , lookup
G protein–coupled receptor wikipedia , lookup
Signal transduction wikipedia , lookup
Hedgehog signaling pathway wikipedia , lookup
Mitogen-activated protein kinase wikipedia , lookup
Transcript
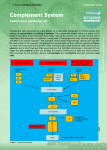
Aims • Describe the activation of the complement cascade via: – Classical pathway – Alternative pathway • Explain how activation of the complement cascade can impact other immunologic processes. • Describe clinical implications of complement deficiencies. • Readings: Abbas & Lichtman, Chapter 8 The Complement Activation Pathways • There are three activation pathways – Classical - C1, C4, C2, C3 – Alternate - properdin pathway – Mannose binding lectin or Lectin – uses MBL to initiate the pathway • All three activation pathways result in the formation of C3 & C5 convertases • They converge at a single terminal pathway Classical Pathway EC RBC antibody bacteria Classical Pathway • C1 complex – C1q has the antibody binding sites – C1r and C1s are serine proteases C1-Inhibitor is released upon binding to Ab and this activates C1r & C1s. Roitt’s Essential Immunology 2-2 C1s C1r C1q C1 C1’ C4a C4b C1’ C4b C1’ C2a C2b C4b C1’ C3 C4b2b C3 Convertase b a C1’ Explosive amplification C4b2b C3a C3b C1’ C5 a b C4b2b3b C5 Convertase C1’ C5a C5b C4b2b3b C1’ C4b2b3b C5b Terminal Pathway Na+ and H2O K+ 6 C4b2b3b 999 7 C5b 8 9 9 9 9 9 Membrane Attack Complex Activators of the Alternative Complement Pathway • Anything that hydrolyzes C3 – leukocyte proteases – plasmin – bacteria or bacteral products (LPS, bacterial cell wall components) – aggregated IgA – cobra venom factor – Cellophane – Water “Ticking over” Alternative Pathway EC RBC C3 bacteria Alternative Pathway EC C3a RBC C3b bacteria Alternative Pathway EC RBC C3b bacteria Alternative Pathway Factor D Factor B a b C3b bacterium Alternative Pathway Ba Bb C3b bacterium Alternative Pathway Properdin C3a C3b C3bBb bacterium C3 Convertase Alternative Pathway Roitt’s Essential Immunology 2-3 Alternative Pathway C3 binding and cleavage is repeated over and over (explosive amplification) Properdin C3a C3b C3bBb bacterium Alternative Pathway Properdin C3bnBb C5 Convertase bacterium Alternative Pathway C5a C5b C3bnBb C5 Convertase bacterium Terminal Pathway Na+ and H2O K+ 6 C3bnBb 999 7 C5b 8 9 9 9 9 9 Membrane Attack Complex Terminal Pathway • Formation of the MAC is identical in classical and alternative pathway once C5 convertase is formed. Abbas & Lichtman’s Basic Immunology 8-6 Lectin Pathway EC RBC MBL bacteria Mannose Binding Lectin (MBL) binds terminal mannose residues of proteins and polysaccharides found on bacteria. Only real difference from the classical pathway is that MBL is substituted for C1 complex during initiation. MBL Terminal Mannose residues Complement Pathway Regulation • C3b by itself has a short half-life (ms) • C3b inactivator (Factor H, DAF, and Factor I) – Break apart stable structures and enzymatically cleave C3b • C1 Inhibitor – Regulates classical pathway by dissociating C1r and C1s from C1q – Can also regulate Lectin pathway by dissociating components of MBL C1’ 999 9 9 7 C4b2b3b 6 C5b 8 999 Complement Pathway Regulation • C4 binding protein – Breaks apart C4b2b (classical C3 convertase) • Anaphylatoxin inactivator or serum carboxypeptidase B – Removes terminal arginine residue from C3a,C4a, and C5a. • Vitronectin (S protein) – Serum protein which can bind C567 preventing complete MAC formation C1’ 999 9 9 7 C4b2b3b 6 C5b 8 999 Cells with Complement Receptors Receptor Specificity Functions Cell types CR1 C3b, C4b stimulates phagocytosis removal of IC by RBCs RBCs, Mf, PMN, B cells CR2 C3b, EBV B cell receptor complex Epstein-Barr virus receptor B cells CR3 C3b stimulates phagocytosis Mf, PMNs CR4 C3b stimulates phagocytosis Mf, PMNs C1q C1q binds IC to phagocytes B cells, Mf, platelets endothelial cells Complement Deficiencies • Deficiency of early cascade members (C1, C4, C2, and C3) – Deficiency in opsonization • Poor phagocytosis resulting in increased infection with encapsulated bacteria. • Poor clearance of IC associated with autoimmune diseases. Complement Deficiencies Type I Hereditary angioedema – Stress and trauma provoked vasodilatation and edema usually of the skin, extremities, or GI mucosa. – Can be fatal if it involve larynx resulting in asphyxiation. – Deficiency of C1INH • spontaneous generation of bradykinin • spontaneous activation of C1 C4a • production of C2a C2a kinin Complement Deficiencies • Deficiency of late cascade members (C5, C6, C7, C8 and C9) – Deficiency in the formation of MAC – C5, C6, C7 or C8 deficiency results in difficulty killing gram negative bacteria (Neisseria meningitidis) Summary • Complement is a group of serum proteins – activated in an orderly fashion from inactive forms. This leads to “spin-off” peptides that have biological activity. • Three main activation pathways and one terminal pathway that leads to the formation of the MAC. • Complement activation is highly regulated. • Possession of complement component receptors lends cells certain biological activities through interaction with complement. • Deficiencies in complement components exist. Next Lecture • Antigen capture and presentation • Exogenous and Endogenous antigens. • Readings: Abbas & Lichtman, Chapter 3 Objectives 1. Describe the similarities and differences between the 3 complement cascade activation pathways. 1. Classical 2. Alternative 3. Lectin (Mannose Binding Lectin) 2. Describe complement regulation and deficiencies.