* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download biotransformation
Metabolomics wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Biochemistry wikipedia , lookup
Metalloprotein wikipedia , lookup
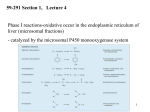
Clinical neurochemistry wikipedia , lookup
Drug design wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Biosynthesis wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacometabolomics wikipedia , lookup
Enzyme inhibitor wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Biotransformation Prepared by Prof .Abdulkader.H.El Daibani 1 Biotransformation Biotransformation (metabolism) of drugs: As most drugs are lipid soluble and be reabsorbed, biotransformation is essential for termination of action and elimination of drugs. 2 Biotransformation Drug metabolism lead to: 1) Increase polarity of drugs by converting lipid soluble drugs into water soluble drugs and therefore enhance excretion. 2) Inactivation of drugs: a) most drugs form inactive metabolites. b) With some drugs both the parent drug and the metabolite are active. e.g. Diazepam Herion → → oxazepam Morphine 3 Biotransformation c) Other drugs, the parent drug is inactive (prodrug) and the metabolite is active and formed by hydrolysis of an ester or amide bond e.g. L-dopa → → Talampicillin → enalapril enalaprilate dopamine ampicillin Cyclophosphamide → 4-ketocyclophosphamide 4 Biotransformation Loss of activity or formation of active metabolites occurs mainly in phase I reaction where a functional group is introduced or exposed. if not rapidly excreted in urine, the metabolites of phase I undergo conjugation in phase II reactions to form highly polar conjugates which are generally inactive and rapidly excreted renally. 5 Biotransformation Sites of drug metabolism: The liver is the major organ of drug metabolism, although other sites (lungs, kidneys, plasma, small intestine. Placenta, skin and brain) may contribute. Cytochrome P450 monooxygenase or mixed function oxidase (M.F.O) system is the major catalyst of drug biotransformation reaction and located in smooth endoplasmic reticulum (SER) of liver and other tissues. 6 Biotransformation Enzymes presented in S.E.R are called Microsomal enzyme. Non-microsomal enzymes are located in mitochondria cytosole phase I enzyme are located in S.E.R. while phase II enzyme are located in the cytosol. Most drugs are metabolized by phase I (oxidation) followed by phase II (conjugation) with glucouronic acid in some cell. e.g. PI PII paracetamol ( p) → Oxi P-OH → P-OH-Gu Conj. 7 Biotransformation In human 12 cytochrome P450 gene families have been identified. The cyto.P450 1, P4502, P4503,(CYP1, CYP2,CYP3). Encode the enzyme involved in the majority of drug transformation. CYP3A4,CYP2D6 are involved in the metabolism of all drugs. as a result of low substrate specificity among cyt.P450 proteins, two or more enzymes may catalyze a given metabolic reaction. 8 Biotransformation Biochemical pathways of drug biotransformation 1)phase I (Non synthetic) reactions : loss of activity or formation of active metabolites occur in phase I ,enzyme of phase I located in S.E.R. a) Oxidation: Most important phase I reactions and involve (M.O.F) system. Aliphatic oxidation: tolbutamide,Ibuprofen. Aromatic oxidation: propranolol, phenytoin S oxidation: cimetidine, chloropromazine(CPZ) N-Oxidation: paracetamol,dapsone. N-dealkylation: morphine,imipramine. O-dealkylation: codeine,indomethacin. Oxidation deamination : diazepam,amphetamine. 9 Biotransformation Cytochrome P450 independent oxidation Amine oxidases (M.AO) sympathomimetic (adrenaline, Noradrenaline) Dehydrogenase-ethanol. Oxidative stress: is a harmful consequence of drug oxidation leading to toxicity or carcinogenicity due to formation of highly reactive intermediates(FR) (free radicals) capable of damaging specific cellular components, also some diseases e.g. parkinsonism may be due to oxidative stress. 10 Biotransformation b)Reduction: Microsomal and non microsomal. Nitroreduction Chloramphenicol, clorazepate . c) hydrolysis: ester-succinylcholine, aspirin, procaine by non specific estrase in liver and other tissue. Amide –Lidocaine, Indomethacin by specific estrase in liver. Peptide-insulin, vasopressin by protease and peptidases in plasma, erythrocyte and other tissue. 11 Biotransformation II) phase II (conjugation) reactions: Also called synthetic reaction because drug or metabolite binds with polar endogenous substance to form water soluble conjugate which is readily eliminated by kidney or in bile>300 in M.W. The drug must possess a chemically active group (mainlyOH introduced-phase I) to which the conjugation substance is attached. The most imp. conjugation reactions are: a) Glucuronidation. b) Sulphation. c) Acetylation. d) Methylation. e) Conjugation with glutathione. f) Conjugation with amino acids. 12 Biotransformation a) Glucuronidation Most common phase II reaction. Catalyzed by glucuronyl transferase in S.E.R. in liver, kidney and other tissues in presence of uridie diphosphate glucuronate (DP-G) as glucuronate donor to form glucaronides which are: 1) Generally inactive But morphine glucuronide is more active than morphine as analgesic. 2) rapidly excreted by kidney and bile by an anion transport mechanism. 3) May be hydrolyzed by β-glucuronidase of intestinal bacterial flora to produce the parent drug which is reabsorbed from S.I (E.H circulation). 13 Biotransformation Examples: Bilirubin, morphine, stilbesterol and chlormphenicol is C.I. in neonates because it may cause grey baby syndrome due to deficiency of glucuronyl transferase in neonates. Most biotransformation reaction are oxidation followed by glucuronidation. oxi. Paracetamol Glu. → para-OH → para-O-Glu phaseI phase II 14 Biotransformation b) Sulphation In presence of 3-phosphadenosin, 5-phosphosulphate, steroids, heparin and α methyl dopa. c) Acetylation catalyzed by N-acetyl transferase in presence of acetyl CoA as an acetyl group donnar limited to drug with primary-NH2. e.g. Isonaizid , sulphonamides, hydralazine. People who are genetically deficient in N-acetyl transferase are called slow acetylators and they may exhibit adverse effects from these drugs e. INH → Peripheral neuropathy slow acetylator Hyralazine and procainamide → slow acetylator S.L.E ( Systemic lupus erythrmatosus) 15 Biotransformation d) Methylation Addition of methyl group via methionine in presence of COMT e.g. metabolism of adrenaline and histamine. e) Conjugation with glutathione Binds with unstable potentially toxic intermediate metabolites e.g. epoxide, paracetamol metabolite to form non harmful compounds. f) Conjugation with amino acids (Glycine and glutamine) e.g. conjugation of aromatic carboxylic acids such as salicylic acid, benzoic acid and nicotinic acid with glycine . 16 Biotransformation Factors affecting biotransformation 1) Enzyme induction and enzyme inhibition. 2) Genetic polymorphism (oxidation,conjugation)genetic differences in the metabolism of drugs e.g. Isoniazid (INH) slow acetylation and fast acetylation. 3) Environmental pollutants –smoking, insecticides e.g D.D.T. (enzyme induction). 4) Pathological factors: liver disease, heart failure and shock (↓ hepatic blood flow). 5) Age: drug metabolism is reduced in extremes of age. 17 Biotransformation 1)enzyme induction and enzyme inhibition:some drugs stimulate (induction ) or inhibit microsomal enzymes in liver. a) Enzyme induction: causes increased activity of microsomal enzyme. Involves de novo (synthesis of new protein). 18 Biotransformation Characteristics of enzyme induction 1) reversible process. 2) Takes one week to appear and 2-3 weeks to disappear after stopping drug. 3) ↑ weight and size of liver due to hypertrophy of hepatocytes. Some drugs increase metabolism of other drugs and their own metabolism (Autoinduction) e.g. Carbamazepine. Inducing agents are specific for a given P450 family e.g. polycyclic aromatic hydrocarbons, cigeratte smoking and barbequed meat →↑CYP1A family. Glucocorticoids and anticonvulsants →↑CYP3A4 family . Acetone and chronic alcohol →↑ CYP2E1 family. Many inducers of cyt. P450 induce enzyme involved in phase II reaction e.g. Glucuronyl transferase and glutathione transferase . 19 Biotransformation Characteristics of inducing agent 1) lipid soluble. 2) Is a substrate for the enzyme it induces. 3) Has long t 1/2. 1) Clinically importance of enzyme inductions may occur e.g. failure of oral contraceptive or loss of anticoagulant, effect of warfarin following Rifampin. 2) Pharmacokinetic tolerance due to antiinduction with antiepileptic drug e.g. carbamazepine and others. 20 Biotransformation 3) useful in therapy- phenobarbitone induces bilirubin conjugation so used in treatment of Hyperbilirubinemia. 4) Disease may result ( Itarogenic Effect) antiepilptics ↑ metabolism and elimination of vit.D → leads to vit. D deficiency→ osteomalasia in adults or rickits in children. 21 Biotransformation B) Enzyme Inhibition Reduction in enzyme activity after exposure to some drugs e.g. cimetidine and ketoconazol inhibit oxidation of drugs by forming tight complex with heam-iron of cyp P450. Erythromycin inhibit CYP3A and its metabolites to form a complex with heam of iron of CYP 450. Other enzyme inhibitors include INH, sodium valproate, metronidazole and ciprofloxacin. Enzyme inhibition tend to be more selective than enzyme induction. 22 Biotransformation Enzyme inhibitor Cimetidine Chloramphenicol Erythromycin ↓metabolism of clinical effect warfarin bleeding tolbutamide hypoglycemia terfenadineor astrmizole arrthmias 23