* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Antipsychotics
Prescription costs wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Drug interaction wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Toxicodynamics wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Chlorpromazine wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Antipsychotic wikipedia , lookup
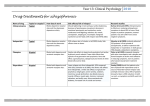
Psychotropics in Psychiatric Patient - Psychotic disorders: Pharmacology and Clinical Applications of Antipsychotics Pongsatorn Meesawatsom B. Pharm., M.Sc. (Pharmacology) Faculty of Pharmacy Srinakarinwirote University Characteristics of schizophrenia Prevalence 0.5–1.0% of population Onset Positive features in late adolescence or early adulthood Aspects of cognitive deficits detectable earlier in life Comorbidity Depression: ∼30–50% Substance abuse: ∼50% Suicide: ∼5–10% Schizophrenia: A Disease with Various Aspects Positive Symptoms Delusions Hallucinations Disorganized speech Catatonia Cognitive Deficits Attention Memory Executive functions (e.g., abstraction) Social/Occupational Dysfunction Work Interpersonal relationships Self-care Negative Symptoms Affective flattening Alogia Avolition Anhedonia Social withdrawal Mood Symptoms Depression Anxiety Aggression Hostility Hopelessness Suicidality Inter-relationship between disease factors and drug-induced adverse factors in the burden of schizophrenia Other effects •Anticholinergic •Prolactin elevation •QTc prolongation Adverse effect of antipsychotic drugs Risk of hyperglycemia/ diabetes Sedation Extrapyramidal symptoms Weight gain Drug-induced factors Tardive dyskinesia Dysphoria Disease factors Suicidality Positive symptoms Cognitive symptoms Negative symptoms Depression/Anxiety Diverse symptoms of schizophrenia Int Clin Psychopharmacol 2005, 20:183–198. Treatment Goal of Schizophrenia Stabilization Phase Treatment Acute Phase Treatment Rapid symptom control Initiation of therapeutically effective dose No need for initial dose titration for tolerability Patient relationship Insight on medication Minimal drug-drug interaction Proven efficacy and safety Maintenance Phase Treatment Relapse/recurrence prevention Adherence Functional recovery Increased tolerance to occasional missed doses Proven relapse prevention effect Improved PSP Factors affecting antipsychotic response Receptor pharmacology (binding capacity) Pharmacokinetics Patient variables Pharmacogenetics (CYP450) Comorbid condition/ polypharmacy The Dopamine hypothesis of psychosis Overactivity of dopamine neurons in the mesolimbic dopamine pathway may mediate the positive symptoms Dopamine hypocactivity in mesocortical dopamine pathway may mediate the negative and cognitive symptoms Dorsolateral prefrontal cortex – negative, cognitive symptoms Ventromedial prefrontal cortex – negative, affective symptoms Brain dopaminergic tracts 2 3 1 4 5 CTZ 6 Lateral hypothalamus Simplify Neurocircuitry of Dopamine in Schizophrenia Mesolimbic pathway Hyperdopaminergia DA D2 Mesocortical pathway Hypodopaminergia DA Limbic Positive symptoms D1 PFCx Negative symptoms Cognitive symptoms Affective symptoms Antipsychotic Drugs: Development Timeline Minimal efficacy with regard to positive symptoms in 20-30% of patients Much weaker effect on negative symptoms than positive symptoms Significant parkinsonian symptoms and anticholinergic effects (poor compliance and potentially disabling) Tardive dyskinesia in a minimum of 20% of patients who receive chronic neuroleptic treatment. At least as effective as typical neuroleptics with regard to positive symptoms More effective than typical agents with regard to negative symptoms Much lower incidence of parkinsonian symptoms and anticholinergic effects than typical agents TD does occur but at much lower incidence Elevated risk of metabolic side effects Therapeutic effects from D2 receptor blockade Amelioration of the positive signs, symptoms of psychosis, manic symptoms, aggressive behaviors Antiemetic effect Modified J Clin Psychiatry 1999;60(suppl 10):5–14. Adverse effects from D2 receptor blockade Extrapyramidal symptom (EPS) Acute; akathisia, acute dystonia, parkinsonism Late; tardive dyskinesia Endocrine effects: prolactin elevation Weight gain due to increase feeding Modified J Clin Psychiatry 1999;60(suppl 10):5–14. Binding affinities of chlorpromazine and haloperidol for various receptor J Psychiatr Pract 2005;11:258–61. Higher potency Higher EPS Lower anticholinergic effect Haloperidol Fluphenazine Trifluoperazine Thioxanthine Perphenazine Pimozide Lower potency Low EPS Higher anticholinergic effect Chlorpromazine Thioridazine Mesoridazine Rational explanations for SDA therapeutic effects Therapeutic effects D2-receptor blockade in the mesolimbic pathway to reduce positive symptoms Enhanced dopamine release and 5-HT2A receptor blockade in the mesocortical pathway to reduce negative symptoms Side-effect profile 5-HT2A antagonism in the nigrostriatal pathway reduces EPS and tardive dyskinesia 5-HT2A antagonism in the tuberoinfundibular pathway reduces hyperprolactinemia Role of 5-HT in Nigrostriatal Dopaminergic Synapse Raphe Sunstantia nigra pars compacta Nigrostriatal tract 5-HT 5-HT2A DA D1 D2 Caudate/putamen Normal function Role of 5-HT in Nigrostriatal Dopaminergic Synapse Raphe Sunstantia nigra pars compacta Nigrostriatal tract 5-HT 5-HT2A DA Haloperidol D1 D2 Caudate/putamen EPS Role of 5-HT in Nigrostriatal Dopaminergic Synapse Raphe Sunstantia nigra pars compacta Nigrostriatal tract 5-HT 5-HT2A DA D1 SDA D2 Caudate/putamen Less EPS Receptor affinities of selected atypical antipsychotics Receptor D2 5-HT1A 5-HT2A 5-HT2C 1 2 H1 M1 HAL CLOZ OLAN 0.7 126 11 2600 875 >7100 45 16 4 1500 16 23 6 360 440 >1500 7 8 6 1.9 RIS 4 210 0.5 25 19 0.7 230 3 7 20 1.9 >10,000 QUET 160 >830 295 1500 ZIP 5 3 0.4 1 ARI 0.45 4.4 3.4 15 7 10 57 87 – – 11 47 61 120 >1,000 >10,000 All values are reported as Ki (nM). Modified from Clin Ther 2004;26:649-66 (partial) (partial) Effects of blockade of neuroreceptors Receptors Effects of blockade D2 Anipsychotic, antimanic, antiaggressive, EPS/akathisia, tardive dyskinesia, increase prolactin, weight gain 5-HT1A Anxiolytic, antidepressant, anti-EPS/akathisia 5-HT2A Anti-EPS/akathisia, possible antipsychotics, improve REM sleep 5-HT2C Possible increased appetite/weight Modified from J Clin Psychiatry 2008;69[suppl4]:26-36. Effects of blockade of neuroreceptors Receptors 1 Effects of blockade Postural hypotension, dizziness, syncope, nasal congestion 2 Antidepressive effect, increase alertness, increase blood pressure H1 Anxiolytic, sedation, weight gain, potentiate CNS depressant drug Modified from J Clin Psychiatry 2008;69[suppl4]:26-36. Effects of blockade of neuroreceptors Receptors Effects of blockade M1 Memory dysfunction, delirium, confusion, sedation, (central) REM sleep disturbance , anti-EPS M2, M3 Blurred vision, attack or exacerbation of narrow-angle (peripheral) glaucoma, dry mouth, sinus tachycardia, constipation urinary retention, interfere pancreatic insulin release Modified from J Clin Psychiatry 2008;69[suppl4]:26-36. Impact of receptor binding affinity on clinical responses of antipsychotics Receptor affinities of selected atypical antipsychotics: Potential risk Receptor HAL CLOZ OLAN RIS QUET ZIP 0.7 126 11 4 160 5 0.45 (partial) 5-HT1A 2600 875 >7100 210 >830 3 4.4 (partial) 5-HT2A 45 16 4 0.5 295 0.4 3.4 5-HT2C 1500 16 23 25 1500 1 15 1 6 7 19 0.7 7 10 57 2 360 8 230 3 87 – – H1 440 6 7 20 11 47 61 M1 >1500 1.9 1.9 >10,000 120 >1,000 >10,000 D2 ARI All values are reported as Ki (nM). EPS risk and hyperprolactinemia Orthostatic hypotension Sedation, weight gain Anticholinergics Modified from Clin Ther 2004;26:649-66 Receptor affinities of selected atypical antipsychotics: Potential Benefit Receptor HAL CLOZ OLAN RIS QUET ZIP 0.7 126 11 4 160 5 0.45 (partial) 5-HT1A 2600 875 >7100 210 >830 3 4.4 (partial) 5-HT2A 45 16 4 0.5 295 0.4 3.4 5-HT2C 1500 16 23 25 1500 1 15 1 6 7 19 0.7 7 10 57 2 360 8 230 3 87 – – H1 440 6 7 20 11 47 61 M1 >1500 1.9 1.9 >10,000 120 >1,000 >10,000 D2 ARI All values are reported as Ki (nM). PD psychosis BPSD, autism Sedative action Alleviate EPS risk Modified from Clin Ther 2004;26:649-66 Sleep quality improvement Aripiprazole Activity at Cloned Human D2 Receptors Dopamine Maximum DA Response (%)* 100 100 nM Dopamine + Aripiprazole Full Receptor Activity 50 Aripiprazole Partial Receptor Activity 100 nM Dopamine + Haloperidol (Modulated) 0 No Receptor Activity 10-10 10-9 10-8 10-7 10-6 Drug Concentration 10-5 (Blocked) Haloperidol *Receptor activity measured as inhibition of forskolin-induced cAMP accumulation in CHO cells transfected with human D2L DNA. Adapted from Burris et al. J Pharmacol Exp Ther. 2002;302:381. Paliperidone vs Risperidone Paliperidone is active metabolite of risperidone via metabolism by CYP2D6. High affinity for D2, 5-HT2A, 1 and 2 receptors Very low affinity for M1 as same as as risperidone Expert Opin Drug Saf. 2007 ;6(6):651-62. Pharmacokinetics differences of risperidone and paliperidone Risperidone Tmax Paliperidone 1-2 hr (risperidone) 1-2 Hr (IR form) 3 hr (paliperidone in CYP2D6 EM) 24 hr (ER form) 17 hr (paliperidone in CYP2D6 PM) T1/2 3 hr 23 hr (IR and ER form) Elimination CYP2D6 to paliperidone (major) pathway CYP3A4 (minor) CYP3A4 to (minor) inactive metabolite and >80% found in urine and 60%unchanged Adverse Effect Profile of Antipsychotics Shift in Risk Perception of Antipsychotics Past Areas of Concern Current Medical Realities Diabetes Weight Gain Weight Gain Sedation Tardive Dyskinesia Insulin Resistance CHD Prolactin Hyperlipidemia Prolactin TD Hyperlipidemia Insulin Resistance Sedation Coronary Heart Disease D2 Blocking-related Side Effects Late onset Acute onset Spectrum of EPS Acute dystonia Relationship between clinical effectiveness, EPS and D2 receptor occupancy 80% Threshold for EPS Threshold for antipsychotic efficacy Medication used to treat EPS Am J Health-Sys Pharm 1997;54:2461-77. Association of medication, target dose, and likelihood of treatment-emergent EPS J Psychiatric Pract 2007;13:13–24. Tardive dyskinesia (TD) TD is a latent extrapyramidal effect generally not occurring for months or years, occur in 20% patient treated with antipsychotic. It is characterized by abnormal movements that can occur in any part of the body, including faces, tongue, shoulders, hips, extremities, fingers, and toes Prominent Feature of TD Lingual-facial hyperkinesias Neck and trunk movements Chewing movements Spasmodic torticollis Smacking and licking of the lips Retrocollis Sucking movements Axial hyperkinesia (hip-rocking) Tongue movements within the oral cavity Tongue protrusion Tongue tremor with mouth open Myokemic movements (wormlike movement on the surface of the tongue) Blinking Grotesque grimaces and spastic facial distortions Torsion movements of the trunk Choreoathetoid movements of the extremities Neuroleptic malignant syndrome NMS is an uncommon but serious and potentially fatal complication of therapy It is a syndrome of EPS, hyperthermia, altered consciousness, and autonomic changes (tachycardia, unstable BP, incontinence) Management Discontinuation of the antipsychotic agents Supportive therapy Bromocriptine may be benificial The onset is sudden and recovery may take 5-10 days after discontinuation of the agent Simplified Pathophysiology of Neuroleptic Malignant Syndrome (NMS) Am J Psychiatry 2007;164:870-876. Spectrum-based concept of NMS J Am Acad Child Adolesc Psychiatry 1992;31:1161–4. Proposed Treatment Algorithm for NMS Spectrum-Related Symptoms Am J Psychiatry 2007;164:870-876. Hyperprolactinemia: possible signs and symptoms Osteoporosis J Clin Psychopharmacol 2007;27:639–661. Mean Plasma Prolactin Level Changes Over 24 Hours in 18 Patients After Taking Clozapine, Olanzapine, or Risperidone and in Five of the Same Patients After Not Taking the Drugs Am J Psychiatry 2002; 159:133–135 Effects of Antipsychotics on Prolactin Levels J Clin Psychopharmacol 2007;27:639–661. Sedation Receptor blocking properties that affect arousal and sleep stages Blocking of H1 sedation Blocking of M1 sedation, REM sleep interference Blocking of 1, 2, 5-HT2A promote cholinergic pedunculopontine (PPT) and laterodorsal tegmental nuclei (LDT) firing REM sleep improvement Receptor affinities of selected atypical antipsychotics Receptor D1 D2 D3 D4 5-HT1A 5-HT2A 5-HT2C 1 2 H1 M1 HAL CLOZ 210 85 0.7 126 2 473 3 35 2600 875 45 16 1500 16 6 360 440 >1500 RIS OLAN 460 31 4 11 10 49 9 27 210 >7100 0.5 4 25 23 7 0.7 8 3 6 20 1.9 >10,000 19 230 7 1.9 QUET 455 160 340 1600 >830 295 1500 ZIP 525 5 7 32 3 0.4 1 ARI 265 0.45 0.8 44 4.4 3.4 15 7 10 57 87 – – 11 47 61 120 >1,000 >10,000 All values are reported as Ki (nM). Clin Ther 2004;26:649-66 (partial) (partial) SGAs and sedation J Clin Psychiatry 2008;69 Suppl 1:18-31. Obesity and metabolic syndromes Clinical issues of weight gain and antipsychotics Not everyone gains weight Difficult to predict who will have weight gain Multifactorial etiology Not dose related ADR. Start in first few weeks Reach plateau between 3 months to 1 year Mean weight gain during treatment with antipsychotic drugs. CNS Drugs 2005; 19 (Suppl. 1): 1–93. Mechanisms of antipsychotic-induced weight gain and metabolic abnormalities Interfere feeding behavior by blocking many neuroreceptor Feeding center Lateral hypothalamus (DA D2) Ventromedial hypothalamus (5-HT 5-HT2A, 5-HT2C) Satiety center Paraventricular nuclei (NE 1, , Histamine H1) Interfere pancreatic insulin release Pancreas (ACh M3 ) Atropine Olanzapine Ziprasidone Risperidone Diabetes 2005; 54:1552–1558. Clozapine Haloperidol Receptor affinities of selected atypical antipsychotics Receptor D1 D2 D3 D4 5-HT1A 5-HT2A 5-HT2C 1 2 H1 M1 HAL CLOZ 210 85 0.7 126 2 473 3 35 2600 875 45 16 1500 16 6 360 440 >1500 RIS OLAN 460 31 4 11 10 49 9 27 210 >7100 0.5 4 25 23 7 0.7 8 3 6 20 1.9 >10,000 19 230 7 1.9 QUET 455 160 340 1600 >830 295 1500 ZIP 525 5 7 32 3 0.4 1 ARI 265 0.45 0.8 44 4.4 3.4 15 7 10 57 87 – – 11 47 61 120 >1,000 >10,000 All values are reported as Ki (nM). Clin Ther 2004;26:649-66 (partial) (partial) Olanzapine-Associated Weight Gain Plateaus After First 39 Weeks of Treatment LOCF; Median = 2.5 Years Mean Weight Change (kg) up to 3 years 8 6 4 2 0 -2 -4 OLZ (N=573) -6 HAL (N=103) -8 0 20 40 60 80 100 Patients Observed for 39 Weeks or More; Week Double-blind and open-label olanzapine. 120 140 160 Kinon BJ, et al. J Clin Psychiatry 2001;62:92-100 Weight gain by olanzapine is not dose dependent (5-20 mg dose range). Why Less weight gain in quetiapine, ziprasidone and aripiprazole? Quetiapine Norquetiapine inhibit norepinephrine reuptake transporter Aripiprazole Low affinity H1, 5-HT2C Partial D2 agonist Ziprasidone Moderate affinity for 1 Low affinity H1 Full 5-HT1A agonist Inhibit 5-HT/NA reuptake transporter SGAs and metabolic abnormalities Clin Psy 2007;68(Suppl 7):27-33. Monitoring protocol for patients on SDAs Baseline 4 weeks 8 weeks 12 weeks Personal/ family history Weight (BMI) Waist circumference () () Blood pressure () () Fasting plasma glucose () () Fasting lipid profile () Quarterly Annually Every 5 years () () () () () () () () () () () () Diabetes Care 2004; 27(2): 596-601. Other Adverse effects QTC interval prolongation Thioridazine, ziprasidone Agranulocytosis Clozapine Epileptogenic Clozapine Retinitis pigmentosa Thioridazine > 800 mg/day Incidence of categorical increases in QTc (Bazett correction) There is a consensus that a QTc interval of >500ms, or an absolute in-crease of 60ms compared with drug-free baseline, puts a patient at significant risk of torsade depointes, ventricular fibrillation and sudden death Clozapine safety issues Clozapine is one of the atypical agents that is EPS/TD free, as same as quetiapine However, clozapine is still reserved as last-line therapy because of its increased incidence of agranulocytosis, myocarditis/cardiomyopathy, and convulsion and the need for frequent monitoring Clozapine safety issues Seizure risk 1-2% and increase to 3-5% if dose is greater than 600 mg/day. Agranulocytosis 1% in general 95% cases in first 6 m, peak in 4-18 week CBC weekly Management of clozapine-induced agranulocytosis US New patients: weekly blood counts UK New patients: weekly blood counts Twice weekly monitoring: WBC Weekly monitoring: WBC 3000- 3000-3500 and ANC >1500 3500 and/or ANC1500-2000 Temporary discontinuation: WBC 2000-3000 and/or ANC 10001500 Permanent discontinuation: WBC <2000 and/or ANC <1000 > 6 months: monitor once every two weeks Discontinue: WBC <3000 and/or ANC ≤1500 Weeks 19-52: at least every 2 weeks > 52 weeks: monitor at least monthly thereafter Contribution of CYP450 in atypical antipsychotic drug metabolism Drug CYP450 1A2 Aripiprazole 2C9/2C19 2D6 3A4 Clozapine Olanzapine //- Paliperidone Quetiapine Risperidone Ziprasidone (1/3 with aldehyde oxidase) Enzyme CYP1A2 Substrate Clozapine, olanzapine CYP2C19 Inhibitor Inducer Fluvoxamine, ciprofloxacin Carbamazepine, smoking Fluoxetine, fluvoxamine Carbamazepine, phenytoin CYP2D6 Aripiprazole, clozapine, olanzapine, risperidone, conventional antipsychotics Bupropion, fluoxetine, paroxetine, duloxetine CYP3A4 Aripiprazole, clozapine,, quetiapine, ziprasidone Azole antifungal Carbamazepine, Most of macrolide except phenytoin, azitromycin rifampin, ARVs; indinavir, nelfinavir, phenobarbita ritonavir l Dose-response curve for seizure risk with clozapine Dose-response curve for extrapyramidal adverse effects with risperidone J Psychiatric Pract 2005;11:116-122. Acute treatment of psychotic patients Injectable, conventional agents are typically used such as haloperidol 5-10 mg IM or zuclopenthixol acetate 50150mg It may be given every hour until Acute symptoms are controlled Side effects occur Patient falls asleep Once control has been obtained, the patient can be converted to oral therapy Selection of antipsychotic agents Based on the patient’s history and safety profile of the available agents Newly diagnosed patients, the APA suggest initiating therapy with atypical agent (SGAs) because of these agents’improve safety profile Monitoring of first episode Less disturbed sleep patterns and decreased anger and anxiety should be observed within the first day or two of treatment, with gradual improvement in other symptoms in the first week and near-maximal effects in six to eight weeks Lack of improvement in the first one to four weeks should prompt an increase in the dose, followed by a change to another drug, usually clozapine or another secondgeneration drug after an additional four to six weeks, if the response remains inadequate N Eng J Med 2003;349:1738-49. Monitoring of early adverse effects It appears within days to weeks of starting the antipsychotic dose It maybe transient and time limited (it will be disappear after the first month of treatment) J Clin Psy 2007;68(Suppl 7):34-43. Initial dose and titration schedule for a firstepisode J Clin Psy 2007;68(Suppl 7):3443. Strategies for managing side effects in stable patients J Clin Psy 2007;68(Suppl 7):34-43. Medical Issues in Schizophrenia Factor Prevalence in Schizophrenia Prevalence in General Population Smoking 75% 25% Obesity 50% 33% 13-14% 7% HIV 3% 0.3% Hepatitis C 20% 1.8% Diabetes Mellitus Other: -inactivity, poor nutrition -substance use Meyer JM and Nasrallah H eds. Medical Illness and Schizophrenia. APPI 2003 Regenold WT, et al. Increased prevalence of type 2 diabetes mellitus among psychiatric inpatients with bipolar I affective and schizoaffective disorders independent of psychotropic drug use. Journal of Affective Disorders. 2002 Jun;70(1):19-26 Medical conditions that may influence antipsychotic treatment dicisions Antipsychotics switching Avoid if possible Consider in Not responing patient with adequate trial Not able to tolerate Non-compliance (switch to depot preparation) Significant long term risk with current medication Obesity, TD, persistent cognitive deficit, CVS problems, DDI Patient/family member request Switching techniques for antipsychotics CNS Drugs 2005; 19 (1): 27-42 Dopaminergic considerations Cross switching of 2 high potency D2 antagonist may increase EPS risk. J Clin Psy 2007;68(Suppl 7):109. Dopaminergic considerations Prolong exposure of high potency D2 antagonist results in D2 supersensitivity Switching D2 antagonist from higher potency to lower potency or D2 partial agonist May lead to switch-emergent dopamine psychosis. Improvement in prolactin-related side effects such as galactorrhea, amenorrhea and sexual dysfunction and EPS Muscarinic considerations There is a potential that patient who have been maintained on anticholinergic antipsychotics to develop cholinergic supersensitivity. Nausea, vomiting and insomnia may occur when anticholinergic drugs is withdrawn or switched to less potent anticholinergic drugs. Muscarinic considerations If patient is being changed because of EPS in which an anticholinergic agents was initiated, the patient can remain on the anticholinergic agent until the cross taper and titrated is completed Exception in the case of clozapine being added as the new therapy, the anticholinergic drugs should be discontinued when the cross taper and titration begins Estimated side effects after switching J Clin Psy 2008;69(Suppl 1):4-17. Conclusions Antipsychotics are not uniform drug class which different in their pharmacological profile, efficacy and ADRs. Adherence of treatment should be enhanced by various strategies e.g. Counseling Awareness of DDI ADR monitoring and management