* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Digestive System Chapter 16
Liver support systems wikipedia , lookup
Fecal incontinence wikipedia , lookup
Intestine transplantation wikipedia , lookup
Gastric bypass surgery wikipedia , lookup
Cholangiocarcinoma wikipedia , lookup
Wilson's disease wikipedia , lookup
Glycogen storage disease type I wikipedia , lookup
Hepatic encephalopathy wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Liver transplantation wikipedia , lookup
Liver cancer wikipedia , lookup
Surgical management of fecal incontinence wikipedia , lookup
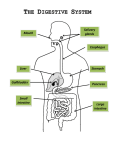
The Digestive System Chapter 16 Function of the Digestive System To break down food into a “usable” (absorbable) form To supply our cells with the nutrients (carbohydrates, proteins, fats, vitamins, minerals, water) they need for energy, growth & repair Organs of the Digestive System Gastrointestinal tract (GIT) – continuous passageway which contains the food from the time it enters the body, until it leaves; organs include: mouth (oral cavity), pharynx, esophagus, stomach, small intestine, large intestine, rectum, anus Accessory organs - participate in digestive processes; organs include: teeth, tongue, salivary glands, liver, gall bladder, pancreas Processes of Digestion 1. Ingestion 2. Movement along GIT Voluntary – e.g. swallowing Involuntary – e.g. peristalsis 3. Secretion – release of water, enzymes, acids, buffers, mucous, etc. into GIT for physical (mechanical) & chemical digestive processes Processes of Digestion 4. Digestion Mechanical processing – physical breakdown of food; e.g. mastication, emulsification, mixing waves, segmentation Chemical digestion – chemical breakdown of food; disassembling of organic molecules into their component parts; requires enzymes carbohydrates (polysaccharides) disaccharides monosaccharides proteins amino acids lipids (triglycerides) fatty acids Processes of Digestion 5. Absorption – movement of nutrients from GIT into blood capillaries (monosaccharides, amino acids, H2O, vitamins, minerals) or lymphatic capillaries (fatty acids) 6. Excretion (Defecation) – removal of waste products from GIT Histology of the GIT 4 layers of tissue surround the lumen of the GIT epithelium – stratified squamous or simple Mucosa columnar lamina propria – loose CT muscularis mucosa – smooth muscle Submucosa CT with BV’s, nerves & lymphatics Muscularis externa Skeletal muscle at beginning & end of GIT, smooth muscle (inner circular; outer longitudinal layer) from lower esophagus to rectum Serosa (a.k.a. visceral peritoneum) Peritoneum & Mesenteries The abdominal cavity is lined with parietal peritoneum & many of the organs within are covered with visceral peritoneum Folds of peritoneum called “mesenteries” attach some organs to others greater omentum lesser omentum mesentery proper Mouth (oral cavity) Regions include the vestibule & oral cavity proper Roof comprised of hard & soft palate; floor primarily comprised of tongue Mucosa of stratified squamous epithelium (nonkeratinized) Tongue – intrinsic & extrinsic muscles papillae filiform fungiform circumvallate Mouth (oral cavity) Salivary glands – secrete saliva – made of H2O, salts & “salivary amylase” Parotid gland Sublingual gland Submandibular gland Teeth – involved in “mastication” Pharynx Common passageway for air & food oropharynx & laryngopharynx lined with stratified squamous epithelium (nasopharynx lined with PSCC) uvula & epiglottis protect airway when swallowing (“deglutition”) nasopharynx uvula oropharynx epiglottis laryngopharynx Esophagus muscular tube extending from pharynx, posterior to trachea, down thoracic cavity, through “esophageal hiatus” of diaphragm, to lower esophageal (a.k.a. cardiac) sphincter at junction of stomach functions in “deglutition” through action of peristalsis mucosa is stratified squamous epithelium variations in muscularis externa – begins as skeletal muscle at upper 1/3, mixed skeletal & smooth muscle in middle, smooth muscle by lower 1/3 Stomach - Gross Anatomy Lower esophageal (cardiac) sphincter Pyloric sphincter Stomach - Histology Rugae – folds of mucosa & submucosa to allow for expansion of stomach Mucosa of simple columnar epithelium with mucous cells Gastric pit leading to gastric glands Stomach – Histology (cont) - Secrete mucus to protect epithelial cells from enzymes & acid - Secrete HCl (for protein digestion) (Peptic) - Secrete pepsinogen which gets converted to “pepsin” when mixed with HCl; for protein digestion Stomach Modifications in stomach include 3 layers of smooth muscle in muscularis externa – outer longitudinal, middle circular, innermost oblique layer Functions of stomach include: temporary storage of food mechanical breakdown of food to “chyme” through powerful mixing waves start of chemical digestion of proteins – pepsin proteins HCl polypeptides Small Intestine - Anatomy - connects stomach to large intestine; 15-20’ long; 1” diameter; held together in abdominal cavity by “mesentery proper” - site for completion of chemical digestion & absorption of nutrients - comprised of three regions: Duodenum – 10” in length; receives chyme from stomach, secretions from liver, gallbladder & pancreas Jejunum – 8’ long; most digestion & absorption occurs here Ileum – 12’ long; connects to cecum of large intestine at iliocecal valve (sphincter) Small Intestine Modifications in mucosa & submucosa of intestinal wall designed to increase functional surface area: Plicae circulares (circular folds) – large transverse ridges; most abundant in jejunum Villi – small finger-like projections of mucosal folds across surface of intestine Plicae circulares Small Intestine Villi Villi lined with “absorptive cells” - mucosal epithelium of simple columnar epithelium with microvilli “brush border” . These cells also produce enzymes (disaccharidases & peptidases) for final digestion of carbs and proteins Submucosa of each villus contains a capillary network & a “lacteal” (lymphatic capillary) for absorption of nutrients Pancreas Stomach Tail Body Head Duodenum Pancreatic duct Retroperitoneal elongated organ, deep to stomach, from duodenum to spleen Both endocrine (pancreatic islets of Langerhans – secretes insulin & glucagon) & exocrine gland (pancreatic acini – secrete pancreatic juice aka pancreatin) Pancreas Pancreatic juice – mixture of enzymes & buffers (sodium bicarbonate) secreted by acinar cells into pancreatic duct & released into duodenum pancreatic amylase Starch (polysaccharide) lipase Lipids (triglycerides) maltose (disaccharide) fatty acids + monoglycerol proteases (trypsin, chymotrypsin, carboxypeptidase) Proteins & polypeptides nucleases – digest RNA & DNA small tripeptides & dipeptides sodium bicarbonate – neutralizes acidic chyme because enzymes in small intestine need an alkaline pH Liver - Anatomy Largest organ within the body Comprised of 4 lobes: Large right & left lobes divided by falciform ligament; small caudate & quadrate lobes Lobes of liver functionally divided into microscopic lobules Liver - Histology Lobules comprised of rows of Hepatocytes arranged radially around a central vein Hepatocytes surround blood sinusoids (capillary structures) which are partially lined with phagocytic Kupffer (aka stellate reticuloendothelial) cells hepatocytes central vein sinusoids Liver Hepatocytes produce bile, which gets secreted into bile canaliculi of lobule Bile canaliculi merge to form bile ducts which eventually merge to create the right & left hepatic ducts Liver & gall bladder Right & left hepatic ducts unite to form common hepatic duct which merges with cystic duct of gall bladder to form common bile duct which enters the duodenum Right hepatic duct Gall bladder – hollow muscular sac under right lobe of liver; stores & concentrates bile Bile released into duodenum functions in emulsification of lipids, absorption of fats (due to presence of bile salts), & excretion of bilirubin Left hepatic duct Liver - Functions The liver has over 200 functions including: Bile production & excretion Metabolic regulation – storage of glycogen, fatty acids, fat-soluble vitamins & minerals interconversion of nutrients (“gluconeogenesis”) detoxification & removal of drugs, toxins & hormones hematological regulation – phagocytosis of worn-out RBCs, bacteria & other pathogens synthesis of plasma proteins Blood Supply to Liver In order for the liver to perform all of its functions, it receives blood through 2 vessels: Hepatic artery - delivers oxygenated blood into sinusoids of liver Hepatic Portal vein – delivers de-oxygenated, nutrient-rich blood from digestive organs to sinusoids of liver Liver uses O2 & nutrients within blood of sinusoids & then blood drains into central veins of lobule & eventually into IVC Large Intestine Begins at the ilium & ends at the anus; 5’ long; 3” in diameter Transverse colon 3 regions: cecum - blind pouch; has appendix attached colon – ascending, (hepatic flexure), transverse, (splenic flexure), descending, sigmoid rectum – last 1” known as “anal canal” Hepatic (rt. Colic) flexure Splenic (lt. colic) flexure Ascending colon Descending colon ileum Ileocecal sphincter Rectum Anal canal Cecum Sigmoid colon Vermiform appendix Rectum Anal canal Internal anal sphincter Rectum External anal sphincter Anus Large Intestine main functions – H2O re-absorption; absorption of some vitamins & minerals; formation & temporary storage of fecal material no chemical (enzymatic) digestion but some bacterial Simple columnar epithelium in mucosa, except at anal canal (strat. Squam.) No plicae circularis or villi Modifications in muscularis externa & serosa : haustra taeniae coli longitudinal muscle layer forms bands called “taeniae coli” which create puckers known as “haustra” serosa forms “epiploic appendages” epiploic appendages Overview of digestion & absorption