* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Dendritic cells in Leishmania infection
Survey
Document related concepts
Infection control wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
DNA vaccination wikipedia , lookup
Sarcocystis wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adaptive immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Transcript
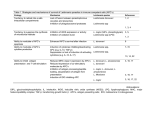
Microbes and Infection 6 (2004) 1402–1409 www.elsevier.com/locate/micinf Review Dendritic cells in Leishmania infection Olga Brandonisio a,*, Rosa Spinelli b, Maria Pepe b a Department of Internal Medicine, Immunology and Infectious Diseases, University of Bari Medical School, Bari, Italy b Department of Human Anatomy and Histology, University of Bari Medical School, Bari, Italy Available online 04 November 2004 Abstract Dendritic cells (DCs) are key elements of the immune system, which function as sentinel in the periphery and alert T lymphocytes about the type of invading antigen and address their polarisation, in order to mount an efficacious immune response. Leishmania spp. are parasitic protozoa which may cause severe disease in humans and domestic animals. In this work, the main studies concerning the role of DCs in Leishmania infection are reviewed, in both the murine and human models. In particular, the importance of the genetic status of the hosts and of the different Leishmania species in modulating DC-mediated immune response is examined. In addition, different approaches of DC-based vaccination against experimental leishmaniasis, which could have important future applications, are summarised. © 2004 Elsevier SAS. All rights reserved. Keywords: Leishmania; Leishmaniasis; Dendritic cells; Vaccine 1. Introduction expression and chemokine production, enabling DC migration and recruitment of other cell types (see in Ref. [2,3]). Dendritic cells (DCs) are a family of professional antigenpresenting cells, which sit in an immature state, capable of antigen uptake and processing, in all peripheral non-lymphoid tissues and therefore function as sentinel of the immune system. After contact with microorganisms or substances associated with infection or inflammation, DCs undergo a process of maturation and migrate to the T-cell areas of lymphoid organs. There they present antigens to naive T cells and modulate their responses [1]. The maturation process consists of (1) increased expression of major histocompatibility complex (MHC) and costimulatory or adhesion molecules such as CD40, CD80, CD86 and CD54; (2) down-regulation of antigen-capture and phagocytic capacity; (3) enhanced cytokine secretion; (4) different patterns of chemokine receptor DCs take up antigens via different groups of receptor families, such as Fc receptors for antigen–antibody complexes, C-type lectin receptors (CLRs) for glycoproteins [4] and pattern-recognition receptors (PRRs) such as Toll-like receptors (TLRs), which enable DCs to recognise a wide range of microbial stimuli [5]. Abbreviations: BMD, bone marrow-derived; CLR, C-type lectin receptors; DCs, dendritic cells; DC-SIGN, DC-specific ICAM-3-grabbing nonintegrin; LCs, Langerhans cells; LPG, lipophosphoglycan; MHC, major histocompatibility complex; MyD, myeloid differentiation; ODN, oligodeoxynucleotides; SLA, soluble leishmanial antigen; TLR, Toll-like receptor. * Corresponding author. Present address: Microbiologia e Immunologia, Policlinico, Piazza G. Cesare, I-70124, Bari, Italy. Tel.: +39-08-05478491; fax: +39-08-0547-8537. E-mail address: [email protected] (O. Brandonisio). 1286-4579/$ - see front matter © 2004 Elsevier SAS. All rights reserved. doi:10.1016/j.micinf.2004.10.004 The information is passed from DCs to T cells via a complex structure, named immunological synapse, which is a specialised molecular organisation that occurs at the contact region between DCs and T cells. It is essentially composed of the T-cell receptor and the MHC molecule, which present the antigenic peptide, but also includes costimulatory and adhesion molecules (mainly CD40–CD40L and CD28– CD80) and cytokine–cytokine receptors [6]. In addition, DCs are essentially flexible and can promote T helper (Th)1, Th2 or regulatory T-cell phenotypes, instructed by the priming signals from microbial and tissue-derived factors. Activated DCs can produce IL-12p70, which regulates Th1 proliferation, interferon (IFN)-c production and parasiticidal ability of activated macrophages; this is a critical process for the containment of infections caused by intracellular pathogens, even including Leishmania infection. However, it is a specific, tightly regulated mechanism requiring the signal mediated by CD40L, in order to protect the host against the O. Brandonisio et al. / Microbes and Infection 6 (2004) 1402–1409 potential harmful Th1-mediated immunopathological reactions. The secretion by DCs of anti-inflammatory cytokines, like IL-10, can also prevent the induction of an exaggerated immune response [6]. Human and mouse DCs can be divided into several subtypes on the basis of surface antigen differences. In humans, they include CD11c+ myeloid DCs (DC1) circulating in the blood, CD11c– plasmocytoid DCs (DC2), which are also found in lymphoid organs, and Langherans’ cells (LCs) in the skin. In mouse, high surface expression of the b2 integrin p150/95 (CD1c) is a characteristic of mature DCs. On the basis of the expression of CD8, CD4, CD205 and CD11b surface markers, several murine DC subtypes can be characterised [7]. Human and mouse myeloid and plasmocytoid DC subsets show partly different functions. However, even if different DC subsets may have different functions in terms of Th1/Th2 induction, cytokine production, and antigen recognition and presentation, these functions rather than being intrinsic, are often related to different stimuli and the cytokine milieu [3]. In addition, immature DCs are considered keepers of peripheral T-cell tolerance to self. Leishmania is a parasitic protozoan, which causes severe diseases in humans and dogs. Its life cycle includes an infective flagellated promastigote stage transmitted by phlebotomine sandfly vectors and an aflagellated amastigote stage in vertebrate hosts. Control measures for leishmaniasis include evaluation of new diagnostic tests [8], screening of new compounds for chemotherapy [9] and development of an affordable and effective vaccine for humans and dogs. For the latter purpose, the precise knowledge of the protective immune response against the parasite, including the role of DCs in the course of the infection, plays a fundamental role. 2. Leishmania–DC interactions: studies in mice 2.1. A silent phase in the skin Moll et al. [10] first demonstrated that murine LCs can ingest Leishmania major and migrate in lymph nodes, where DCs harbour persistent parasites and enable the maintenance of T-cell memory. However, a recent paper indicates that although parasites can be detected in mouse lymph nodes a few hours after infection, none of the DC emigrants from the skin harbours parasites. The authors conclude that DCs could not be the vehicle that ferries the parasites from the skin to the lymph nodes [11]. Interestingly, after L. major infection of C57BL resistant mice with low parasite dose into a dermal site, there was a prolonged silent phase of parasite amplification in the skin, lasting 4–5 weeks, before the onset of lesions and immunity [12]. The establishment of the infection can be favoured through different evasion mechanisms, like the inhibition of DC maturation (see below) or induction of regulatory T cells. In fact, during infection by L. major in mice, CD4+ CD25+ regulatory T cells accumulate in the dermis, where they 1403 suppress, in part by IL-10 production, the ability of effector T cells to eliminate the parasite [13]. 2.2. IL-12 production An impairment of IL-12 production was demonstrated in bone marrow-derived (BMD) Leishmania-infected macrophages and was selectively observed in infected cells [14]. In contrast, DCs are the main source of IL-12 in early Leishmania infection. In fact, murine C57BL/6 skin-derived DCs were recognised as the main source of IL-12p40 immediately after dermotropic L. major infection [15,16], whereas IL12p70 release by DCs required IFN-c and prolonged (72 h) incubation [15] or addition of CD40L [17]. After viscerotropic Leishmania donovani infection in BALB/c mice, splenic DCs that are localised in the periarteriolar lymphoid sheath are the critical source of early IL-12p40 production [18,19]. The effect of Leishmania infection on IL-12 induction and DC maturation may vary according to DC subtype and to Leishmania species. In fact, infection in vitro of murine BMD DCs with L. mexicana promastigotes failed not only to induce IL-12 release, but also to activate immature DCs. The importance of additional stimuli is underlined in this work, since the addition of IFN-c plus LPS restored DC maturation and IL-12 production in infected cells [20]. Murine splenic DC subsets can vary in their ability to produce IL-12 and carry out phagocytosis of L. major amastigotes in mice. In fact, CD4+ CD8– DCs were the most permissive cells, followed by CD4– CD8– DCs; CD4– CD8+ cells were the least permissive but the best IL-12 producer in response to infection [21]. Moreover, it was found that resting murine and human myeloid cells, including DCs, contain preformed, membrane-associated IL-12p70 stores, which are released within minutes after in vitro or in vivo contact with L. donovani [22]. 2.3. The role of genetic susceptibility/resistance DC responses can also vary according to the genetic susceptibility or resistance of mice, on the basis of studies performed mainly in the murine model of L. major infection. Skin-DCs from L. major-infected C57BL/6 resistant mice or BALB/c susceptible mice both exhibit up-regulation of surface markers (MHC class I and II antigens, CD40, CD54, and CD86) and release IL-12p70, thus suggesting that genetic susceptibility to L. major is not dependent on DC inability to respond to the parasite [23]. However, an increased expression of IL-4R was observed on LCs infected with L. major from susceptible but not resistant mice [24], and the expression of the costimulatory molecule CD80 was down-regulated on LCs from susceptible but not resistant mice [25]. Moreover, in lymph node DCs from susceptible, but not resistant mice in vivo infected with L. major, a decreased CD40 activity was observed, which correlated with underproduction of IL-12p40 and IL-12p40 mRNA expression [26]. 1404 O. Brandonisio et al. / Microbes and Infection 6 (2004) 1402–1409 In addition, in a model of L. amazonensis infection, it was shown that in both BALB/c and C3H/HeJ (resistant) mice, amastigotes enter and activate BMD DCs, but in the former, infection fails to induce CD40-dependent IL-12 release and rather potentiates IL-4 production; transfer of infected BALB/c DCs into syngeneic resistant recipients induces release of IL-4 and IL-10 by primed Th cells [27]. Susceptible and resistant mice infected with L. major were also analysed for amastigote load and cell surface phenotype of lymph node DCs [28]. Cells expressing the DC specific marker CD11c were the most frequently infected cells in draining lymph nodes of all mice tested. CD11c+infected cells from C57BL/6 mice displayed a weak parasitic load, a typical dendritic morphology and frequently expressed CD11b or F4/80 myeloid differentiation (MyD) markers. In contrast, some CD11c+-infected cells from BALB/c mice were multinucleated giant cells, which presented a dramatic accumulation of parasites without differentiation markers at their surface. However, data from a recent paper argue against a relevant genetic difference in the DCs initiating the anti-parasite Th cell response in C57BL/6 and BALB/c mice, but rather underline the importance of DC turnover during the infection. In fact, in both strains there were two different waves of antigen-containing DCs in vivo in experimental L. major infection. In the first wave, DCs presented leishmanial antigens, produced IL-12 but were not infected, whereas DCs of the second wave were able to ingest the parasites [29]. 2.4. TLR involvement: studies in null mice After the demonstration that TLR2 is essential for the pro-inflammatory activity of the protozoan parasite Trypanosoma cruzi (the causative agent of Chagas’ disease) and that the glycosylphosphatidylinositol (GPI) anchor of this parasite activates TLR2 [30], studies have been undertaken to evaluate a possible involvement of TLRs in Leishmania infection. Firstly, studies were performed on a murine macrophage cell line transfected with a dominant-negative version of the MyD88, which is a protein adaptor involved in TLR-signalling pathways and production of inflammatory cytokines [5]. Transfection inhibited activation of the IL-1a promoter, which is selectively activated by L. major infection. Furthermore, stimulation of IL-1a RNA expression by L. major was inhibited in peritoneal macrophages from MyD88–/–, compared to MyD88+/+ mice, thus indicating that the parasite stimulates IL-1a promoter activity and mRNA expression in macrophages through MyD88- and TLR-dependent pathways [31]. Similar results showing that MyD88-dependent pathways are essential for the development of the protective IL-12mediated Th1 response against L. major were obtained by Muraille et al. [32] and de Veer et al. [33]. Following inoculation of L. major, MyD88(–/–) C57BL/6 mice presented large footpad lesions containing numerous infected cells. In response to soluble leishmanial antigens (SLAs), cells from lesion-draining lymph nodes showed a typical Th2 profile, similarly to infected BALB/c mice. Moreover, IL-12p40 plasma levels collapsed in infected MyD88(–/–) mice compared with infected wild-type C57BL/6 mice. Importantly, administration of exogenous IL-12 rescues L. major-infected MyD88(–/–) mice, demonstrating that the susceptibility of these mice is a direct consequence of IL-12 deficiency [32]. Furthermore, among leishmanial major surface glycoconjugated molecules, a role for promastigote lipophosphoglycan (LPG) in TLR2 activation was demonstrated [33]. In fact, LPG, but not LPG without the lipid portion nor glycoinositolphospholipids (GIPLs) or proteophosphoglycan, activates IL-12p40 and tumour necrosis factor (TNF)-a synthesis in macrophages from wild-type but not from MyD88-null mice, thus indicating that LPG signals through a TLR pathway. In this work, human kidney 293T cells were also transfected with seven different human TLR expression constructs and evaluated for NFkB and IL-8 promoter activation after addition of LPG. LPG stimulated both IL-8 and a synthetic NFkB-luciferase reporter only in cells transfected with TLR2 [33]. As regards DCs, recent data on mice suggest that MyD88dependent receptors are implicated in their maturation in response to Leishmania infection. In fact, L. donovaniinduced DC maturation in terms of up-regulated expression of MHC II and costimulatory receptors (CD40, CD80/B7.1 and CD86) was partially abolished in MyD88deficient mice [34]. Interestingly, in this work the use of a green fluorescent protein-expressing parasite showed that DCs undergoing maturation in vivo display no parasite internalisation, thus indicating that Leishmania-induced maturation results from direct recognition of Leishmania by DCs, and not from DC infection [34]. 3. Leishmania–DC interactions: studies in humans The importance of CD40–CD40L interaction for IL12p70 production, which is also investigated for immunotherapy of infections, is underlined in a study on human myeloid-derived human DCs [35]. The IL-12p70 production by L. major-harbouring myeloid-derived human DCs showed a CD40/CD40L-dependent process. In fact, DCs which have ingested metacyclic promastigotes of L. major up-regulated HLA-DR, CD86 and CD40 surface molecules, thus suggesting a process of maturation. However, these cells were unable to produce IL-12p70, IL-1b, IL-6, IL-10 or TNF-a, while the addition of CD40 ligand trimer 8–10 h after infection resulted in a marked IL-12p70 production. IL12 production by DCs in vitro required opsonisation of parasites with 5% normal human serum, mimicking the in vivo infection. Interestingly, flow cytometry analysis by an antiIL12 and anti-LPG mAbs showed that IL-12 was colocalised to LPG+ (i.e. Leishmania-infected) DCs. In addition, when autologous primed T cells were co-cultured with these infected cells, they were able to proliferate and produce IFN-c [35]. O. Brandonisio et al. / Microbes and Infection 6 (2004) 1402–1409 The effect of infection on DCs may vary according to Leishmania species in the human model also. In fact, monocyte-derived DCs, infected with metacyclic promastigotes (i.e. parasites at infectious stage) and then stimulated with CD40L, showed a different ability to secrete IL-12p70, according to the Leishmania species employed for the infection. In fact, L. major, which is responsible for self-healing cutaneous leishmaniasis, induced IL-12p70 release, differently from L. tropica, which may cause persistent cutaneous lesions and from the viscerotropic species L. donovani [36]. These opposite effects may be related to the difference in leishmanial surface molecules LPG and GIPLs, which show a great diversity between the various species. The response to different Leishmania species of monocyte-derived DCs and macrophages from blood donors was also investigated in a study assessing gene expression profiles by microarray analysis [37]. Human DCs and macrophages shared a vast majority of genes expressed at baseline, but each cell type responded very distinctly to infection with diverse pathogens. In particular, after infection with metacyclic promastigotes of L. major or L. donovani, a small number of genes, notably IFN-c-induced genes, were differentially regulated by the two species in macrophages and DCs [37]. As regards TLRs, studies in humans were performed on natural killer (NK) cells, which can also express these receptors. Interestingly, purified L. major LPG up-regulates both mRNA and the membrane expression of TLR-2 in human NK cells, and enhances IFN-c and TNF-a production and nuclear translocation of NFkB. The activation effect was more intense with LPG purified from infectious metacyclic promastigotes than from non-infectious procyclic parasites. Since the difference between the molecules derived from these two stages lies exclusively in the number of phosphosaccharide repeat domains and in the composition of glycan side chains that branch off these domains, TLR-2 could distinguish between phosphorylated glycan repeats on LPG molecules [38]. 4. Evasion of Leishmania parasites from DC presentation 4.1. Inhibition of DC migration The inhibition of DC migration could represent a stratagem for the pathogens to escape the host immune system. Products secreted by L. major promastigotes inhibit the motility of murine splenic DCs in vitro [39], and L. major LPG inhibits migration of murine LCs [40]. The chemokine– chemokine receptor pathway may be involved in this inhibition. In fact, DCs can be selectively recruited due to their expression of different chemokine receptors: chemokines that arise under inflammatory conditions and act on CCR1, CCR2, CCR5 and CCR6 attract immature DCs to the affected sites. After antigen uptake, during maturation, 1405 chemokine receptor expression changes: CCR1, CCR2 and CCR5 are down-regulated and replaced by CCR7 and CXCR4, thus enabling DCs to migrate in the draining lymph nodes in response to corresponding chemokines [41]. Absence of CCR2 shifts the L. major-resistant phenotype to a susceptible state dominated by Th2 cytokines [42]. Furthermore, Leishmania infection can differently modulate chemokine receptor expression on host cells [43]. Interestingly, after chronic infection with L. donovani in mice, there was IL-10-mediated inhibition of CCR7 expression and inhibition of DC migration from the marginal zone to the T-cell areas of the spleen, which may contribute to the development of visceral leishmaniasis [44]. 4.2. Inhibition of DC maturation Results from different investigations suggest that Leishmania parasites tend to delay DC maturation to favour the establishment of the infection before the onset of the acquired immune response. As described above, after L. major infection in C57BL resistant mice with low parasite dose into a dermal site, there was a prolonged silent phase of parasite amplification in the skin, before the onset of lesions and immunity, suggesting an impairment of DC activation [10]. In mouse BMD DCs in vitro infected with L. mexicana, an impairment of maturation and IL-12 secretion was selectively induced by uptake of parasites, whereas infected cells retained the capacity of full activation after addition of LPS plus IFN-c [20] and retained the capacity of exogenous antigen presentation [45]. In addition, metacyclic promastigotes of L. amazonensis phagocytosed by murine DCs did not induce DC maturation, which was instead elicited if parasites were previously opsonised with specific antibodies [46]. In lymph node of mice, CD11c+ L. major-infected DCs express low MHC II levels and no detectable CD86 expression, thus suggesting that they might constitute a reservoir of parasites [28]. In addition, L. donovani inhibits expression of the lipid and glycolipid antigen-presenting molecules CD1 on human BMD DCs, thus impairing CD1-mediated presentation of lipid antigens and activation of T cells [47]. CD1 molecules may be involved in the protective immune response against Leishmania species, which harbour abundant glycolipid antigens. 4.3. Inhibition of IL-12p70 production by DCs As mentioned above, studies in human myeloid DCs have demonstrated the inhibitory effect of infection with L. tropica and L. donovani, but not L. major, on IL-12p70 production after addition of CD40L [36]. 4.4. Induction of IL-10 Finally, DCs could be indirectly modulated by Leishmania infection through the induction of IL-10, which can 1406 O. Brandonisio et al. / Microbes and Infection 6 (2004) 1402–1409 Table 1 Escape of Leishmania from DC presentation DC subtype LCs Splenic DCs Splenic DCs BM-derived DCs BM-derived DCs Lymph node DCs BM-derived DCs Monocyte-derived DCs Function inhibited Migration Migration Migration and CCR7 expression Activation markers expression IL-12 secretion Activation markers expression MHC II and CD86 expression Expression of CD1 molecules IL-12p70 production Host BALB/c mice BALB/c mice C578L/6 mice CBA mice Parasite L. major L. major L. donovani L. mexicana Reference [40] [39] [44] [20] BALB/c mice BALB/c and C57BL/6 mice Humans Humans L. L. L. L. [46] [28] [47] [36] render DCs tolerogenic through the up-regulation of the inhibitory receptor leukocyte immunoglobulin-like receptor (LIR)-2, resulting in T-cell hyporesponsiveness in vitro [48]. The main escape mechanisms of Leishmania parasites from DC-mediated immune-responses are listed in Table 1. 5. Targeting Leishmania–DC interaction DC-specific ICAM-3-grabbing nonintegrin (DC-SIGN) is CLR which is expressed almost exclusively on differentiated blood myeloid and tissue monocyte-derived DCs. It is being extensively studied not only as pathogen-binding receptor, but also as mediator of DC-T-cell interactions and as an escape mechanism for intracellular pathogens, which can target DC-SIGN to shift the protective Th1 towards Th2 cell balance [49]. Interestingly, DC-SIGN was indicated as a major ligand for the amastigote stage of L. pifanoi [50] and for LPG of L. mexicana [51]. In addition, it was recently demonstrated that DC-SIGN is a receptor for promastigote and amastigote infective stages from both visceral (L. infantum) and New World cutaneous (L. pifanoi) Leishmania species, but not for L. major metacyclic promastigotes, an Old World species causing cutaneous leishmaniasis. However, in this work, Leishmania binding to DC-SIGN was independent from LPG [52]. Since binding of DC-SIGN by distinct Leishmania species and strains can favour parasite survival and persistence, it was suggested that this receptor might be a therapeutic target for both visceral and cutaneous leishmaniasis [52]. 6. DC-based vaccination and immunotherapy Several studies suggest the potential of tumour Ag-pulsed DCs or DCs engineered to secrete cytokines such as IL-12 or IL-18 to induce anti-tumour immunity [53,54]. Moreover, DC-based immunotherapy or vaccination is also emerging as a tool to combat infectious diseases, since DCs can be longlived, thus ensuring the maintenance of an efficient presentation and stimulation for T cells in draining lymph nodes [2,6,55]. The first studies demonstrating that LCs can be used as a natural adjuvant to induce a protective immune response amazonensis major donovani tropica, L. donovani against leishmaniasis were performed in a murine model of L. major infection. A single i.v. application of LCs, pulsed with promastigote lysate in vitro, induced protection in susceptible BALB/c mice against subsequent challenge with L. major parasites. Development of resistance was paralleled by a reduced parasite burden and a shift of the cytokine expression towards a Th1-like pattern [56]. In a murine BALB/c model of L. donovani infection, DCs engineered to secrete IL-12 and pulsed ex vivo with soluble L. donovani antigens were potent vaccine [57]. Not only antigen-pulsed, but also Leishmania-infected DCs were used for vaccination: in another work L. majorinfected syngeneic DCs protected BALB/c susceptible mice against L. major challenge [23]. Moreover, LCs loaded with a mixture of the recombinant leishmanial antigens LACK, KMP-11, gp63 and PSA or with the single antigen LeIF mediated significant protection against challenge with L. major parasites, upon adoptive transfer into naïve susceptible mice [58]. In this work, the protection was found to be dependent on IL-12, since in Ag-pulsed LCs from IL-12-deficient mice, the capacity of DCs to mediate protection was completely abrogated. Another approach to vaccination is to deliver the antigen to endogenous DCs with the aid of molecules, which bind surface receptors on DCs and deliver an activating signal. The importance of CD40L in DC activation and IL-12 production after Leishmania infection is underlined above. Interestingly, a robust induction of IL-12 production by DCs was obtained by using murine L929 transfected cells expressing CD40L and the Leishmania antigen gp63 [17]. Vaccination with these co-transfected cells provided a significant degree of protection against challenge with virulent L. major and L. amazonensis in genetically susceptible mice. Oligodeoxynucleotides (ODNs) which contain immunostimulatory CG motifs (CpG ODN) and activate DCs by promoting Th1 responses were also investigated as adjuvant for vaccination against leishmaniasis in susceptible BALB/c mice. Mice receiving SLA plus CpG ODN showed a highly significant reduction in swelling compared to SLAvaccinated mice and enhanced survival compared to unvaccinated mice. The modulation of the response to SLA by CpG ODNs was maintained even when mice were infected 6 months after vaccination [59]. CpG ODNs were also able to reduce the pathogenicity of a live L. major promastigote vaccine, without reducing its efficacy [60]. O. Brandonisio et al. / Microbes and Infection 6 (2004) 1402–1409 1407 Table 2 DC-based vaccines against experimental Leishmania infection Vaccine LCs pulsed with L. major lysate DCs engineered to secrete IL-12 and pulsed with soluble L. donovani antigens L. major-infected skin-derived DCs Skin-derived DCs pulsed with LeIF antigen or LACK + KMP-11 + gp63 antigens L. major Ag-pulsed, CpG ODN-activated BM-derived-DCs The mechanism by which CpG ODNs mediate the adjuvant effect in vivo was investigated in BALB/c mice. Vaccination with leishmanial LACK antigen and CpG ODNs led to the presence of CD11c+ DCs in the draining lymph nodes, which were potent producers of IL-12p70 and IFN-c, and were capable of vaccinating naïve BALB/c mice against L. major infection [61]. However, in another work, IL12 expression by the immunising DCs was not required for induction of host resistance in mice vaccinated with a single dose of L. major Ag-pulsed BMD DCs, stimulated by prior in vitro exposure to CpG ODN [62]. DCs pulsed with soluble L. donovani antigen were also employed for immunotherapy of murine visceral leishmaniasis together with the conventional chemotherapy with sodium antimony gluconate. This combined treatment potentiates the antileishmanial effect of antimony and results in complete clearance of parasites from both the liver and the spleen [63]. Finally, targeting DCs with antigen-containing liposomes was highly effective in inducing anti-tumour immunity [64] and could be exploited for immunotherapy of leishmaniasis, in which liposomal amphotericin B is the first-line treatment in industrialised countries [65]. [1] [2] [3] [4] [5] [6] [7] [8] [9] [10] [11] [12] 7. Conclusions [13] Possible applications of this type of vaccine include not only human cutaneous and visceral leishmaniasis in hyperendemic countries, but also canine leishmaniasis in areas, including Mediterranean countries and Latin America, where the dog is the main domestic reservoir of the parasite. In these areas, vaccination of dogs may be an important measure for control of the human disease. Route i.v. i.v. i.d. i.v. i.v. Challenge L. major L. donovani L. major L. major L. major Reference [56] [57] [23] [58] [62] References The main investigations concerning DC-based vaccination against experimental leishmaniasis are summarised in Table 2. The possibility of DC-based vaccination against leishmaniasis is exciting, even if further studies are needed. These studies may have practical applications for vaccination purposes after an exact standardisation concerning parasite antigen for an appropriate DC instruction, route of antigen delivery, stage of DC maturation and usefulness of exogenous activating factors like CD40L or cytokines (see also in Ref. [55]). Experimental model BALB/c mice BALB/c mice BALB/c BALB/c BALB/c C57BL76 [14] [15] [16] [17] [18] C. Reis e Sousa, Activation of dendritic cells: translating innate into adaptive immunity, Curr. Opin. Immunol 16 (2004) 21–25. H. Moll, Dendritic cells and host resistance to infection, Cell. Microbiol 5 (2003) 493–500. M. Sundquist, A. Rydstrom, M.J. Wick, Immunity to Salmonella from a dendritic point of view, Cell, Microbiol 6 (2004) 1–11. T.B. Geijtenbeek, S.J. Van Vliet, A. Engering, B.A. T’Hart, Y. Van Kooyk, Self- and nonself-recognition by C-type lectins on dendritic cells, Annu. Rev. Immunol 22 (2004) 33–54. K. Takeda, S. Akira, TLR signaling pathways, Semin. Immunol 16 (2004) 3–9. J. Colino, C.M. Snapper, Dendritic cells, new tools for vaccination, Microbes Infect 5 (2003) 311–319. K. Shortman, Y.J. Liu, Mouse and human dendritic cell subtypes, Nat. Rev. Immunol 2 (2002) 151–161. D. Otranto, P. Paradies, M. Sasanelli, R. Spinelli, O. Brandonisio, Rapid immunochromatographic test for serodiagnosis of canine leishmaniasis, J. Clin. Microbiol 42 (2004) 2769–2770. L. Fumarola, R. Spinelli, O. Brandonisio, In vitro assays for evaluation of drug activity against Leishmania spp, Res. Microbiol 155 (2004) 224–230. H. Moll, S. Flohé, M. Rollinghoff, Dendritic cells in Leishmania major-immune mice harbor persistent parasites and mediate an antigen-specific T-cell immune response, Eur. J. Immunol. 25 (1995) 693–699. T. Baldwin, S. Henri, J. Curtis, M. O’Keeffe, D. Vremec, K. Shortman, E. Handman, Dendritic cell populations in Leishmania majorinfected skin and draining lymph nodes, Infect. Immun 72 (2004) 1991–2001. Y. Belkaid, S. Mendez, R. Lira, N. Kadambi, G. Milon, D. Sacks, A natural model of Leishmania major infection reveals a prolonged “silent” phase of parasite amplification in the skin before the onset of lesion formation and immunity, J. Immunol. 165 (2000) 969–977. Y. Belkaid, The role of CD4(+)CD25(+) regulatory T cells in Leishmania infection, Expert Opin. Biol. Ther 3 (2003) 875–885. Y. Belkaid, B. Butcher, D.L. Sacks, Analysis of cytokine production by inflammatory mouse macrophages at the single-cell level: selective impairment of IL-12 induction in Leishmania-infected cells, Eur. J. Immunol. 28 (1998) 1389–1400. E. Von Stebut, Y. Belkaid, T. Jakob, D.L. Sacks, M.C. Udey, Uptake of Leishmania major amastigotes results in activation and interleukin 12 release from murine skin-derived dendritic cells: implications for the initiation of anti-Leishmania immunity, J. Exp. Med. 188 (1998) 1547–1552. P. Konecny, A.J. Stagg, H. Jebbari, N. English, R.N. Davidson, S.C. Knight, Murine dendritic cells internalize Leishmania major promastigotes, produce IL-12p40 and stimulate primary T-cell proliferation in vitro, Eur. J. Immunol. 29 (1999) 1803–1811. G. Chen, P.A. Darrah, D.M. Mosser, Vaccination against the intracellular pathogens Leishmania major and L. amazonensis by directing CD40 ligand to macrophages, Infect. Immun 69 (2001) 3255–3263. P.M. Gorak, C.R. Engwerda, P.M. Kaye, Dendritic cells, but not macrophages, produce IL-12 immediately following Leishmania donovani infection, Eur. J. Immunol. 28 (1998) 687–695. 1408 O. Brandonisio et al. / Microbes and Infection 6 (2004) 1402–1409 [19] C.R. Engwerda, P.M. Kaye, Organ-specific immune responses associated with infectious disease, Immunol. Today 21 (2000) 73–78. [20] C.L. Bennett, A. Misslitz, L. Colledge, T. Aebischer, C.C. Blackburn, Silent infection of bone marrow-derived dendritic cells by Leishmania mexicana amastigotes, Eur. J. Immunol 31 (2001) 876–883. [21] S. Henri, J. Curtis, H. Hochrein, D. Vremec, K. Shortman, E. Handman, Hierarchy of susceptibility of dendritic cell subsets to infection by Leishmania major: inverse relationship to interleukin-12 production, Infect. Immun 70 (2002) 3874–3880. [22] M. Quinones, S.K. Ahuja, P.C. Melby, L. Pate, R.L. Reddick, S.S. Ahuja, Preformed membrane-associated stores of interleukin (IL)-12 are a previously unrecognized source of bioactive IL-12 that is mobilized within minutes of contact with an intracellular parasite, J. Exp. Med. 192 (2000) 507–516. [23] E. Von Stebut, Y. Belkaid, B.V. Nguyen, M. Cushing, D.L. Sacks, M.C. Udey, Leishmania major-infected murine langerhans cell-like dendritic cells from susceptible mice release IL-12 after infection and vaccinate against experimental cutaneous leishmaniasis, Eur. J. Immunol. 30 (2000) 3498–3506. [24] H. Moll, A. Scharner, E. Kampgen, Increased interleukin 4 (IL-4) receptor expression and IL-4-induced decrease in IL-12 production by langerhans cells infected with Leishmania major, Infect. Immun 70 (2002) 1627–1630. [25] M.L. Mbow, G.K. DeKrey, R.G. Titus, Leishmania major induces differential expression of costimulatory molecules on mouse epidermal cells, Eur. J. Immunol 31 (2001) 1400–1409. [26] F.P. Heinzel, R.M. Rerko, A.M. Hujer, Underproduction of interleukin-12 in susceptible mice during progressive leishmaniasis is due to decreased CD40 activity, Cell. Immunol. 184 (1998) 129–142. [27] H. Qi, V. Popov, L. Soong, Leishmania amazonensis-dendritic cell interactions in vitro and the priming of parasite-specific CD4(+) T cells in vivo, J. Immunol 167 (2001) 4534–4542. [28] E. Muraille, C. De Trez, B. Pajak, F.A. Torrentera, P. De Baetselier, O. Leo, Y. Carlier, Amastigote load and cell surface phenotype of infected cells from lesions and lymph nodes of susceptible and resistant mice infected with Leishmania major, Infect. Immun 71 (2003) 2704–2715. [29] A.C. Misslitz, K. Bonhagen, D. Harbecke, C. Lippuner, T. Kamradt, T. Aebischer, Two waves of antigen-containing dendritic cells in vivo in experimental Leishmania major infection, Eur. J. Immunol 34 (2004) 715–725. [30] M.A. Campos, I.C. Almeida, O. Takeuchi, S. Akira, E.P. Valente, D.O. Procopio, L.R. Travassos, J.A. Smith, D.T. Golenbock, R.T. Gazzinelli, Activation of Toll-like receptor-2 by glycosylphosphatidylinositol anchors from a protozoan parasite, J. Immunol 167 (2001) 416–423. [31] T.R. Hawn, A. Ozinsky, D.M. Underhill, F.S. Buckner, S. Akira, A. Aderem, Leishmania major activates IL-1 alpha expression in macrophages through a MyD88-dependent pathway, Microbes Infect 4 (2002) 763–771. [32] E. Muraille, C. De Trez, M. Brait, P. De Baetselier, O. Leo, Y. Carlier, Genetically resistant mice lacking MyD88-adapter protein display a high susceptibility to Leishmania major infection associated with a polarized Th2 response, J. Immunol 170 (2003) 4237–4241. [33] M.J. De Veer, J.M. Curtis, T.M. Baldwin, J.A. Di Donato, A. Sexton, M.J. McConville, E. Handman, L. Schofield, MyD88 is essential for clearance of Leishmania major: possible role for lipophosphoglycan and Toll-like receptor-2 signaling, Eur. J. Immunol 33 (2003) 2822– 2831. [34] C. De Trez, M. Brait, O. Leo, T. Aebischer, F.A. Torrentera, Y. Carlier, E. Muraille, MyD88-dependent in vivo maturation of splenic dendritic cells induced by Leishmania donovani and other Leishmania species, Infect. Immun 72 (2004) 824–832. [35] M.A. Marovich, M.A. McDowell, E.K. Thomas, T.B. Nutman, IL-12p70 production by Leishmania major-harboring human dendritic cells is a CD40/CD40 ligand-dependent process, J. Immunol. 164 (2000) 5858–5865. [36] M.A. McDowell, M. Marovich, R. Lira, M. Braun, D. Sacks, Leishmania priming of human dendritic cells for CD40 ligand-induced interleukin-12p70 secretion is strain and species dependent, Infect. Immun 70 (2002) 3994–4001. [37] D. Chaussabel, R.T. Semnani, M.A. McDowell, D. Sacks, A. Sher, T.B. Nutman, Unique gene expression profiles of human macrophages and dendritic cells to phylogenetically distinct parasites, Blood 102 (2003) 672–681. [38] I. Becker, N. Salaiza, M. Aguirre, J. Delgado, N. Carrillo-Carrasco, L.G. Kobeh, A. Ruiz, R. Cervantes, A.P. Torres, N. Cabrera, A. Gonzalez, C. Maldonado, A. Isibasi, Leishmania lipophosphoglycan (LPG) activates NK cells through toll-like receptor-2, Mol. Biochem. Parasitol 130 (2003) 65–74. [39] H. Jebbari, A.J. Stagg, R.N. Davidson, S.C. Knight, Leishmania major promastigotes inhibit dendritic cell motility in vitro, Infect. Immun 70 (2002) 1023–1026. [40] A. Ponte-Sucre, D. Heise, H. Moll, Leishmania major lipophosphoglycan modulates the phenotype and inhibits migration of murine langerhans cells, Immunology 104 (2001) 462–467. [41] A.P. Vicari, B. Vanbervliet, C. Massacrier, C. Chiodoni, C. Vaure, S. Ait-Yahia, C. Dercamp, F. Matsos, O. Reynard, C. Taverne, P. Merle, M.P. Colombo, A. O’Garra, G. Trinchieri, C. Caux, In vivo manipulation of dendritic cell migration and activation to elicit antitumour immunity, Novartis Found. Symp 256 (2004) 241–269. [42] N. Sato, S.K. Ahuja, M. Quinones, V. Kostecki, R.L. Reddick, P.C. Melby, et al., CC chemokine receptor (CCR)2 is required for langerhans cell migration and localization of T helper cell type 1 (Th1)-inducing dendritic cells. Absence of CCR2 shifts the Leishmania major-resistant phenotype to a susceptible state dominated by Th2 cytokines, b cell outgrowth, and sustained neutrophilic inflammation, J. Exp. Med. 192 (2000) 205–218. [43] M.A. Panaro, R. Spinelli, S. Lisi, M. Sisto, A. Acquafredda, L. Fumarola, V. Mitolo, O. Brandonisio, Reduced expression of the chemokine receptor CCR1 in human macrophages and U-937 cells in vitro infected with Leishmania infantum, Clin. Exp. Med 3 (2004) 225– 230. [44] M. Ato, S. Stager, C.R. Engwerda, P.M. Kaye, Defective CCR7 expression on dendritic cells contributes to the development of visceral leishmaniasis, Nat. Immunol 3 (2002) 1185–1191. [45] C.L. Bennett, L. Colledge, H.E. Richards, P.A. Reay, C.C. Blackburn, T. Aebischer, Uncompromised generation of a specific H-2DMdependent peptide-MHC class II complex from exogenous antigen in Leishmania mexicana-infected dendritic cells, Eur. J. Immunol 33 (2003) 3504–3513. [46] E. Prina, S.Z. Abdi, M. Lebastard, E. Perret, N. Winter, J.C. Antoine, Dendritic cells as host cells for the promastigote and amastigote stages of Leishmania amazonensis: the role of opsonins in parasite uptake and dendritic cell maturation, J. Cell Sci 117 (Pt 2) (2004) 315–325. [47] J.L. Amprey, G.F. Spath, S.A. Porcelli, Inhibition of CD1 expression in human dendritic cells during intracellular infection with Leishmania donovani, Infect. Immun 72 (2004) 589–592. [48] B.G. Beinhauer, J.M. McBride, P. Graf, E. Pursch, M. Bongers, M. Rogy, U. Korthauer, J.E. de Vries, G. Aversa, T. Jung, Interleukin 10 regulates cell surface and soluble LIR-2 (CD85d) expression on dendritic cells resulting in T-cell hyporesponsiveness in vitro, Eur. J. Immunol 34 (2004) 74–80. [49] Y. Van Kooyk, T.B. Geijtenbeek, DC-SIGN: escape mechanism for pathogens, Nat. Rev. Immunol 3 (2003) 697–709. [50] M. Colmenares, A. Puig-Kroger, O.M. Pello, A.L. Corbi, L. Rivas, Dendritic cell (DC)-specific intercellular adhesion molecule 3 (ICAM-3)-grabbing nonintegrin (DC-SIGN, CD209), a C-type surface lectin in human DCs, is a receptor for Leishmania amastigotes, J. Biol. Chem 277 (2002) 36766–36769. [51] B.J. Appelmelk, I. Van Die, S.J. Van Vliet, C.M. VandenbrouckeGrauls, T.B. Geijtenbeek, Y. Van Kooyk, Cutting edge: carbohydrate profiling identifies new pathogens that interact with dendritic cellspecific ICAM-3-grabbing nonintegrin on dendritic cells, J. Immunol 170 (2003) 1635–1639. O. Brandonisio et al. / Microbes and Infection 6 (2004) 1402–1409 [52] M. Colmenares, A.L. Corbi, S.J. Turco, L. Rivas, The dendritic cell receptor DC-SIGN discriminates among species and life cycle forms of Leishmania, J. Immunol 172 (2004) 1186–1190. [53] T. Tatsumi, J. Huang, W.E. Gooding, A. Gambotto, P.D. Robbins, N.L. Vujanovic, S.M. Alber, S.C. Watkins, H. Okada, W.J. Storkus, Intratumoral delivery of dendritic cells engineered to secrete both interleukin (IL)-12 and IL-18 effectively treats local and distant disease in association with broadly reactive Tc1-type immunity, Cancer Res 63 (2003) 6378–6386. [54] C.G. Figdor, I.J. De Vries, W.J. Lesterhuis, C.J. Melief, Dendritic cell immunotherapy: mapping the way, Nat. Med 10 (2004) 475–480. [55] H. Moll, Dendritic cells as a tool to combat infectious diseases, Immunol. Lett 85 (2003) 153–157. [56] S.B. Flohé, C. Bauer, S. Flohé, H. Moll, Antigen-pulsed epidermal langerhans cells protect susceptible mice from infection with the intracellular parasite Leishmania major, Eur. J. Immunol. 28 (1998) 3800–3811. [57] S.S. Ahuja, R.L. Reddick, N. Sato, E. Montalbo, V. Kostecki, W. Zhao, et al., Dendritic cell (DC)-based anti-infective strategies: DCs engineered to secrete IL-12 are a potent vaccine in a murine model of an intracellular infection, J. Immunol. 163 (1999) 3890–3897. [58] C. Berberich, J.R. Ramirez-Pineda, C. Hambrecht, G. Alber, Y.A. Skeiky, H. Moll, Dendritic cell (DC)-based protection against an intracellular pathogen is dependent upon DC-derived IL-12 and can be induced by molecularly defined antigens, J. Immunol 170 (2003) 3171–3179. [59] K.J. Stacey, J.M. Blackwell, Immunostimulatory DNA as an adjuvant in vaccination against Leishmania major, Infect. Immun. 67 (1999) 3719–3726. 1409 [60] S. Mendez, K. Tabbara,Y. Belkaid, S. Bertholet, D. Verthelyi, D. Klinman, R.A. Seder, D.L. Sacks, Coinjection with CpG-containing immunostimulatory oligodeoxynucleotides reduces the pathogenicity of a live vaccine against cutaneous leishmaniasis but maintains its potency and durability, Infect. Immun 71 (2003) 5121–5129. [61] J.A. Shah, P.A. Darrah, D.R. Ambrozak, T.N. Turon, S. Mendez, J. Kirman, C.Y. Wu, N. Glaichenhaus, R.A. Seder, Dendritic cells are responsible for the capacity of CpG oligodeoxynucleotides to act as an adjuvant for protective vaccine immunity against Leishmania major in mice, J. Exp. Med 198 (2003) 281–291. [62] J.R. Ramirez-Pineda, A. Frohlich, C. Berberich, H. Moll, Dendritic cells (DC) activated by CpG DNA ex vivo are potent inducers of host resistance to an intracellular pathogen that is independent of IL-12 derived from the immunizing DC, J. Immunol 172 (2004) 6281–6289. [63] M. Ghosh, C. Pal, M. Ray, S. Maitra, L. Mandal, S. Bandyopadhyay, Dendritic cell-based immunotherapy combined with antimony-based chemotherapy cures established murine visceral leishmaniasis, J. Immunol 170 (2003) 5625–5629. [64] C.L. Van Broekhoven, C.R. Parish, C. Demangel, W.J. Britton, J.G. Altin, Targeting dendritic cells with antigen-containing liposomes: a highly effective procedure for induction of antitumor immunity and for tumor immunotherapy, Cancer Res 64 (2004) 4357– 4365. [65] A. Cascio, L. Di Martino, P. Occorsio, R. Giacchino, S. Catania, A.R. Gigliotti, C. Aiassa, C. Iaria, S. Giordano, C. Colomba, V.F. Polara, L. Titone, L. Gradoni, M. Gramiccia, S. Antinori, A 6 day course of liposomal amphotericin B in the treatment of infantile visceral leishmaniasis: the Italian experience, J. Antimicrob. Chemother 54 (2004) 217–220.