* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Introduction to Anti-Fungals
Discovery and development of integrase inhibitors wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Drug discovery wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of tubulin inhibitors wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Psychopharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
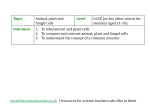
Introduction to Anti-Fungals Selective toxicity = the ability to harm the parasite/virus while minimally affecting your patient 1. Example mechanism: fungi have cell walls and people have cell membranes, so target components of cell walls Classification of anti fungal drugs 1. Polyenes (e.g. amphotericin B) 2. Flucytosine 3. Azoles 4. Echinocandins 5. Topical drugs for mucocutaneous infections (see handout) 1) Ergosterol is a good opportunity to express selective toxicity 2) Drugs that attack the mitotic spindles keep the fungi/viral infections from reproducing Agents for systemic fungal infections ○ Amphotericin B ○ Azoles (Triazoles are now favorites) ○ Flucytosine ○ Echinocandins Oral Mucocutaneous Agent ○ Griseofulvin ○ Terbinafine Topical Mucocutaneous Agents ○ Nystatin ○ Topical Azoles ○ Topical Allylamines 1. Amphotericin B o Mode of Action: - Binds ergosterol and forms leaky pores (channels) on cell membranes o Antifungal Activity: - Candida spp, Cryptococcus neoformans, Blastomyces dermatitis, Histoplasma capsulatum, Sporothrix schenkii, Coccidioides immitis, Paracoccidioides braziliensis, Aspergillus spp, Penicillium marneffei and Mucormyces 2. Flucytosine o Mechanism of action: - Flucytosine undergoes several steps of metabolism within the fungal cells to the active metabolites 5-fluorodeoxyuridine monophosphate (inhibits DNA synthesis) and fluorouridine triphosphate, an inhibitor of RNA synthesis o Clinical uses: - Cryptococcus neoformans, some Candida species and dermatiaceous molds that cause chromoblastomycosis o Adverse Effects: - Intestinal flora converts flucytosine to its metabolite fluorouracil (an anti neoplastic drug) bone marrow toxicity, anemia, leukopenia and thrombocytopenia Systemic Antifungal Drugs 1. Azoles o Classification of azoles: 1) Imidazoles - Ketoconazole, miconazole and clotrimazole (mic and clo- are now used only as topical agents) 2) Triazoles - Itraconazole, fluconazole and voriconazole o Mechanism of action: - azoles inhibit fungal cytochrome p450 enzymes and reduce ergosterol synthesis. triazoles are more selective for fungal p450 than imidazoles Fluconazole: - highly water soluble and good body fluid distribution (e.g. CSF) - Unlike ketoconazole and itraconazole, fluconazole has high bioavailability and has the least effects of all azoles on cytochrome P450 enzymes - It is the agent most used in treatment of mucocutaneous candidiasis. Voriconazole: - new, good absorption, high bioavailability and less plasma protein binding than itraconazole. Oral and i.v. formulations are available - Undergoes hepatic metabolism, less human P450 enzyme induction. 2. Echinocandins o Mechanism of action: destroys fungal cell wall by inhibiting -glycan synthesis o Clinical uses: 1) Caspofungin: o disseminated and mucocutaneous candida infections, empiric antifungal therapy during febrile neutropenia. o Recommended for invasive aspergillosis only as salvage therapy in patients not responding to amphotericin B 2) Micafungin: o is used only for mucocutaneous candidiasis and prophylaxis of candida infection in bone marrow transplant patients 3) Anidulafungin: o esophageal candidiasis, invasive candidiasis septicemia Drugs for Mucocutaneous Infection 1. Griseofulvin ○ Used only for systemic treatment of dermatophytosis ○ Griseofulvin binds to microtubules and disrupts mitosis. It binds to keratin in the skin and protects from new fungal infections ○ Requires 2-6 weeks for the drug to take effect with skin treatment and months for nail treatment 2. Terbinafine o Available in oral formulations o Used for treating dermatophytes esp. onychomycosis o Interferes with ergosterol biosynthesis (like azoles), no action on P450, inhibits fungal squalene epoxidase accumulation of sterol squalene which is toxic to fungi