* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Antifungals
Compounding wikipedia , lookup
List of comic book drugs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
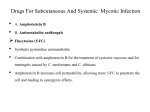
ANTIFUNGALS When to think fungus? Diabetes Immunosuppresed Acidosis Neutropenic Already on broad spectrum antibiotics. Travel to location with an endemic fungal pathogen. Disturbances in the GI mucosa either by inflammation or mechanical. Burns Trauma Neonatal Fungal Cell Structure and Targets Fungal Cell Structure and Targets Several antifungals such as polyenes, azoles, and allylamines take advantage of the difference in sterol content CLASSES OF ANTIFUNGALS Azoles Echinocandins Polyenes Fungal Death Immune Modulation and Other Fungal Treatments Antimetabolites and Other Allylamines POLYENES Natamycin Rimocidin Filipin Nystatin Amphotericin B Candicin MECHANISM OF ACTION FOR POLYENES Polyenes act by binding to ergosterol in the fungal cell membrane. This forms pores that increase the permeability to protiens and monovalent and divalent cations depolarizing the membrane. MECHANISM OF ACTION FOR POLYENES AMPHOTERICIN B Produced by Streptomyces nodosus First available in the US in 1959 ANITFUNGAL SPECTRUM FOR AMPHOTERICIN B Drug of Choice for: Invasive Fungal Infections Cryptococcal meningitis (in combo with 5-FC) Blastomycosis (followed by itraconazole) Fungal Endocarditis (plus 5-FC) Endophthalmitis Severe disseminated coccidioidomycosis Severe Histoplasmosis +/- steroids Mucormycosis/Zygomycosis Penicilliosis (followed by itraconazole) ANITFUNGAL SPECTRUM FOR AMPHOTERICIN B Active against almost all fungi except: Apergillus terreus Scedosporium apiospermum, prolificans Trichosporon spp. Candida lusitaniae Antiprotozoan Activity Viseral Leishamniasis Primary Amoebic Meningoencephalitis Toxicities of Amphotericin Fever, Rigor, Hypotension, Nausea, Vomiting Usually subsides with repeated infusions. Alleviated with narcotics, usually meperidine. Premedication with Tylenol, diphenhydramine, hydrocortisone, or heparin has little influence on rigors/fever. Anorexia, Wasting Nephrotoxicity Electrolyte Imbalances and Acidosis (RTA) Hepatotoxicity Anemia and blood dyscrasias Hypokalemia, hypocalcemia, hypomagnesemia, low bicarb Leukopenia, thrombopenia, anemia (decreases erythropoietin) Cardiac arrhythmias Drug Interactions of Amphotericin Flucytosine increases toxicity and vice versa. Diuretics or Cisplatin increase renal toxicity and risk of hypokalemia. Corticosteroids increase risk of hypokalemia. In general combination with nephrotoxic drugs increases the risk of serious renal damage. Deferent preparations for Amphotericin B Amphotericin B Deoxycholate Oral Preparations Bladder Irrigations Cholesteryl sulfate complex (Colloidal Dispersion) Lipid complex (Abelcet) Ampho B complexed with 2 lipid bilayer ribbons. Larger volume distribution and clearance from the blood. Achieves higher tissue concentrations in liver, spleen, lung. Less renal toxicity. Deferent preparations for Amphotericin B Liposomal formulation (AmBisome Vesicular bilayer liposome with ampho B intercalated within the membrane Same advantages as the lipid complex. Acute infusion-related reactions common (20-40%) 86% Occur in the 1st 5 minutes with chest pain, dyspnea, hypoxia, severe abdominal, flank, or leg pain. Responds to holding the infusion and diphenhydramine (1mg/kg). To use Amphotericin B Would prefer to use lipid formulations in most all situations to limit renal toxicity. Has to be infused slowly and with pre/post hydration. May pre-medication with Tylenol and an antihistamine but more important to infuse slowly. Given most patients with invasive fungal disease are immunosupressed would not pre-medicate with steroids. Must follow electrolytes and renal function. May continue to use with mild elevations in renal function and may spread out the dosing interval to maintain renal function. Nystatin Drug of Choice Thrush Formulations Swish and Swallow Troches No IV formulation and is not absorbed. Toxicity Virtually no adverse effects. Back to Menu AZOLES Imidazoles Miconazole* Ketoconazole Clotrimazole Econazole* Bifonazole Butoconazole Fenticonazole Isoconazole Oxiconazole* Sertaconazole* Sulconazole Tioconazole Triazoles * Used solely as topical formulations. Fluconazole Itraconazole Isavuconazole Ravuconazole Posaconazole Voriconazole Terconazole Thiazoles Abafungin MECHANISM OF ACTION FOR AZOLES Azoles inhibit the fungal cytochrome P-450 3-A dependent enzyme 14-alpha demethylase which is needed to synthesize ergosterol. This leads to depletion of ergosterol in the cell membrane and accumulation of toxic intermediate sterols leading to increased membrane permeability and inhibition of fungal cell growth. MECHANISM OF ACTION FOR AZOLES Toxicities of Azoles Also inhibit mammalian cytochrome P450dependent enzymes causing multiple drug interactions. Itraconazole inhibits CYP 3A4 the most. Class C in pregnancy with only fluconazole considered safe with breast feeding. Itraconazole Drug of choice for: Bone involvement by Coccidioidiomycosis. Bastomycosis after primary treatment with amphotericin. Chromoblastomycosis Mild-mod Histoplasmosis Sporotrichosis Pharmacology 99% protein-bond and does not penetrate the CSF. Recommended taking with food and acidic drinks. May need to check drug levels given multiple drug interactions. Itraconazole Drug Interactions Contraindicated with cisapride, dofetilide, ergot alkaloids, lovastatin, midazolam, pomozide, quinidine, simvastatin, triazolam. Decreased absorption with antacids, PPI, H2 blockers, or achlorhydria. Increases adverse effects with trazadone. Do not use with CrCl <30 ml/min Inhibits P450 3A4 metabolism and has multiple more interations. Toxicities Negative inotrope (may cause heart failure) Hepatotoxicity Nausea, Vomiting, and Diarrhea are the most common side effects. Ketoconazole Drug of choice: Tinea versicolor (instructed to sweat after taking) Pharmacology Does not cross into the CSF. Gastric acid required for absorption. Avoid Antacids, H2 blockers, PPI, buffered didanosine Achlorhydria (need to drink with HCl acid) Coca Cola increased absorption by 65% Ketoconazole Drug Interactions Do not use with cisapride, midazolam, pimozide, trazolam. Levels reduced by isoniazid, rifampin, efavirenz. Avoid >200mg/day with ritonavir. Inhibits P450 3A4 and has many drug interactions. Need to reduce trazodone dose. Toxicities Hepatotoxicity High doses (>800mg/day) may case adrenal deficiency. Fluconazole Drug of choice for: Spectrum of coverage: Vaginal candidiasis Candidemia (unless C. glabrada or C. krusei) Thrush (non-AIDS) Candidal Peritonitis Mild to Mod Coccidioidomycosis, CNS Cocci Non-meningeal Cryptococcosis (non-AIDS) Candida Cryptococcus Coccidioidiomycosis Does not cover: Aspergillus C. glabrada, C. tropicalis Scedosporium Zygomycetes Dematiaceous molds Fluconazole Pharmacology Excellent bioavailability with CNS penetration. Drug Interactions Reduce dose by 50% with CrCl 11-50ml/50 Many drug interactions due to P-450 Increases levels of cyclosporine, phenytoin, theophylline and INR on warfarin. May increase levels of statins Toxicity Side effects uncommon, mild nausea Hepatotoxicity May cause alopecia at high doses for long periods. Voriconazole Drug of choice for: Invasive pulmonary aspergillosis Scedosporium apiospermum infection Fusarium infection Spectrum of coverage: Aspergillus to include A. terreus Candida to include C. krusei Fusarium and some molds Dimorphic Fungi except Sporothrix Does not cover: Zygomcetes Scedosporium prolificans Voriconazole Drug Interactions Substrate and inhibitor of CYP2C9, 2C19, 3A4. Check levels with treatment failures. Ritonivir decreases voriconazole levels. Will need dose adjustment for cyclosporine, omeprazole, phenytoin, tacrolimus. Avoid using sirolimus. Avoid rifampin, rifabutin, and sirolimus. Inhibits metabolism of benzodiazpines, CCB, statins, and methadone. Increases level of estrogen and progestin with oral contraceptives Reduce maintenance dose by 50% with Child-Pugh class A/B. Voriconazole Toxicities Type IV anaphylactoid reactions. Rare severe skin reaction and photosensitivity. Rare hepatotoxicity. Transient visual disturbances common. Advise against night driving and strong sunlight. Vehicle in IV form may accumulate in renal impairment and would use oral form with CrCl <50mL/min. Posaconazole Drug of choice: 2nd line for Mucormycosis/Zygomycosis Salvage therapy. Broadest range of antifungal coverage. Aspergillosis Zygomycosis Fusarosis Ssscedosporium Phaeohyphomycosis Dimorphic fungi (Histo, Blasto, Cocci) Refractor Candidiasis Refractory Cryptococcosis Refractory Chromoblastomycosis Dermatiaceous molds Posaconazole Drug Interactions Must take with fatty meals for absorption. Metabolized by glucuronidation. CYP 34A inhibitor Contraindicated with ergot alkaloids and other CYP 3A4 substrates which increase QT interval such as cisapride, pimozide, halofantrine, and quinidine. Reduce dose with vinca alkaloids, CCB, and statins. Reduce cyclosporine dose by 25% and tacrolimus dose by 66%. May need to reduce benzodiazepines Levels reduced by rifabutin, phenytoin, and cimetidine. Toxicities Toxicities similar to other azoles. Hepatotoxicity Clotrimazole Formulations Vaginal Creams Oral Troches Dermal Creams Back to Menu ECHINOCANDINS Anidulafungin Caspofungin Micafungin MECHANISM OF ACTION FOR ECHINOCANDINS Glucan Synthesis Inhibitors Inhibits the enzyme 1,3-beta glucan synthase resulting in the depletion of glucan polymer in the fungal cell wall. The weakened cell wall is unable to withstand osmotic stress. MECHANISM OF ACTION FOR ECHINOCANDINS Echinocandin B Spectrum of Coverage for Echinoocandins Spectrum of coverage: Cidal against Candida and Aspergillus sp. Including ampho B and triazole resistant strains. Does not cover: Dimorphic fungi Zygomycetes Anidulafungin Drug of choice for: Candidemia and candidal systemic infecitons. Candida Esophagitis Bloodstream infections with C. glabrata or C. krusei. Anidulafungin Pharmacology No CSF penetration. Not excreted in the urine. No dose adjustment in renal or hepatic insufficiency. Side effects: Slow infusion rate to prevent histamine reactions. Diluent contains dehydrated alcohol. Overall remarkably non-toxic, like other echinocandins. Caspofungin Drug of choice for: Candidemia and candidal systemic infecitons. Bloodstream infections with C. glabrata or C. krusei. Pharmacology No drug in CSF or Urine Metabolized in the liver. Toxicity Also remarkable non-toxic. Puritis at infusion site or N/V/F/C/diarrhea/headache rarely report during it infusion. Caspofungin Drug Interactions: Must increase the daily dose to 70mg when using concurrently with rifampin. May need to increase the dose with other enzyme inducers such as carbamazepine, dexamethasone, efavirenz, nevirapine, phenytoin. Multiple interactions with immunosuppressants. Cyclosporine will increase caspofungin levels Caspofungin with decrease tacrolimus levels May need to adjust dose with liver dysfunction. Reduce daily dose to 35mg QD with ChildPugh score 7-9. Micafungin Drug of choice for: Candidemia and candidal systemic infecitons. Candidal Esophagitis Bloodstream infections with C. glabrata or C. krusei. Pharmacology No antagonism seen when used with other antifungals. No dose adjustment need with severe renal impairment or moderate hepatic impairment. No CSF or Urine penetration. Micafungin Drug Interactions Increases levels of sirolimus and nifedipine. Not dialysed. Toxicities Histamine-medicated reactions possible with rapid infusions. Again well tolerated like all echinocandins. Back to Menu ALLYLAMINES Terbinafine – Lamisil Amorolfine Naftifine – Naftin Butenafine – Lotrimin Ultra MECHANISM OF ACTION FOR ALLYLAMINES Works similar to azoles by inhibiting synthesis of ergosterol but at an earlier step in the pathway. Inhibits squalene epoxidase. Terbinafine Drug of choice: Onychomycosis Toxicity Hepatotoxicity (monitor LFT’s) Neutropenia May exacerbate lupus. Do not use with liver disease or CrCl <50 mL/min. Inhibits CYP 2D6. Multiple drug interaction. Rifampin with increase its clearance. Back to Menu ANTIMETABOLITES AND OTHER Benzoic acid Ciclopirox – (ciclopirox olamine) Unsaturated fatty acid derived from natural castor oil; fungistatic as well as anti-bacterial and anti-viral Flucytosine or 5-fluorocytosine Topical used against Tinea versicolour, Tinea corporis/cruris, Seborrheic dermatitis Tolnaftate – Tinactin, Desenex, Aftate, or other names Undecylenic acid Has antifugal properties but must be combined with a keratolytic agent such as in Whitfield's Ointment Antimetabolite Griseofulvin Binds to polymerized microtubules and inhibits fungal mitosis Flucytosine Drug of Choice: Drug Interactions: Cryptococcal meningitis (plus amphotericin B) Reduce in renal dysfunction Toxicity Myelosuppression Nausea Must use in combination therapy to prevent resistance from rapidly developing. Loss of cytosine permease to cross membrane. Altered enzyme for 5FC conversion. Griseofulvin Drug of choice Tinea capitis Drug Interactions Do not use in liver failure or porphyria. Decreases INR with warfarin. Reduced oral contraceptive efficacy. Toxicity Photosensitivity Lupus like syndrome / exacerbation of Lupus Septra Drug of Choice: Paracoccidioidomycosis Back to Menu NOVEL ANTIFUNGALS AND IMMUNE MODULATION Gamma Interferon Cryptococcosis Coccidioidomycosis New azole compounds to with broader spectrums of activity and less resistance. Isavuconazole Vibunazole Surgery Aspergilloma (Fungus Ball) Chromoblastomycosis (if small and few) Lobomycosis Phaeohyphomycosis (black molds) Plus itraconazole Back to Menu