* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Organism Classification
Survey
Document related concepts
Transcript
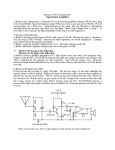
Organism Classification Hyphae Aspergillus species, pseudallescheria boydii Dermatophytes (Trichophyton species, Microsporum species), Phialophora species, Fusarium species. Dimorphic Fungi Blastomyces, coccidioides, Histoplasma, Sporothrix. Grow as a mold in nature (27c) but quickly convert to parasitic yeast form after infecting the host (37c). Yeast Candida spesies, Cryptococcus neoformans Clinical classification of mycoses Classification Superficial versicolor Site Infected Stratum corneum Example Tinea & hair Cutaneous epidermis & nails Dermatophytosis Subcutaneous Dermis & Sporothrichosis subcutaneous tissue Systemic Disease of 1 Candidiasis internal organs Cryptococcosis Antifungics Drugs Classification: Antifongic Agents Polyene Flucytosine Azoles Nystatin Amphotericin B Imidazoles Allylamines Triazoles Terbinafine Ketoconazole Fluconazole Miconazole Itraconazole Clotrimazole Ravuconazole Econazole Posaconazole Isoconazole Voriconazole Griseofulvine Naftifine Pneumocandins Caspofungin Antifungal Agents 1- inhibitors of the fungal cell mb ( polyenes, azoles, allylamines) 2- inhibitors of DNA (flucytosine) 3- inhibitors of cell wall biosynthesis (caspofungin) Adapted from Ghannoum MA and RiceLB Clin Micro Rev. 1999;12:501-517. Mechanism of action of azoles Azoles antifungals exert their effects primarily by inhibiting the fungal cytochrome P450 3A enzyme lanosterol 14-α-demethylase, preventing the conversion of lanosterol to ergosterol. This in turn leads to depletion of ergosterol (a regulator of fungal cell membrane fluidity and asymmetry) and accumulation of sterol precursors. As a result of ergosterol depletion, the integrity and function of the fungal cell membrane is disrupted, eventually leading to cell lysis Mechanism of action of Amphotericin Amp B acts principally by binding to ergosterol in the fungal cell menbrane, effectively creating pores in the cell mb, leading to depolarisation of the mb and cell leakage. Amp B binds>>> to ergosterol than to cholesterol Toxic effects Mechanism of action of 5Flucytosine = fluorinated cytosine analogue Acts by inhibiting nucleic acid synthesis It is actively transported into cells, where it is metabolically transformed by deamination to toxic metabolite 5-Fu. 5Fu convert to 5-fluoridine triP=> antimetabolite => disrupts Prot synthesis. monoP => -- thymidylate synthase=>disrupts DNA synthesis. Resistance in monotherapie+++ Diffuse LCR 60-80% Mechanism of action of allylamines Inhibition of sterol biosynthesis by interfering with squalene epoxidase (critical enzymes in the biosynthesis of ergosterol). faulty cell mb with altered permeability Mechanism of action of Griseofulvin Inhibits growth by inhibiting fungal cell mitosis caused by polymerization of cell microtubules It has activity only against dermatophyte fungi Mechanism of action of caspofungin Interfering with 1,3 ß glucan, preventing synthesis of essential cell wall polysaccharides protect the cell from osmotic and structural stresses Cilofungin 1= but was dropped bcs of the toxicity of Hydrophobic vehicle. 1- Clotrimazole 1= imidazoles inadequate for the ttt of systemic infection, bcs it induce its own metabolism rapidly (oral, or IV) It use now largely as topical therapy (vulvovaginal candidiasis). [Canestan] 2- Miconazole poorly soluble in water, therefore administer in castor oil vehicle for IV admi. This vehicle is responsible for many adverse effects: Phlebitis, pruritis, N, V, anemia, thrombocytosis and hyperlipidemia (high dose), cardiorespiratory arrest (rapid infusion). Ttt of inf. Caused by pseudallescheria boydii Topical use (vulvovaginal candediasis, and superficial skin inf). 3- Ketoconazole is poorly soluble in aqueous fluids (acidic PH<3). Absorption is impaired in pt w elevated gastric PH SE: GI discomfort >50% inhibition of adrenal steroid synthesis (gynecomastia, libido, azoospermia, secondary to testosterone synthesis following high daily dosage >600mgd or during prolonged admi of lower dosages. 4- Itraconazole (vehicle= cyclodextrin) have greater specifity against fungal versus mammalian cyt P450. same SE of Ketoconazole. vehicle is not absorbed following oral adm, Use of IV formulation is limited to 2w, bcs of potential nephrotoxicity secondary to accumulation of vehicle. 5- Fluconazole is markedly differentpharmacologic featurs: small molecular weight Complete absorption of low protein binding drug water solubility Well tolerated, does not inhibit testicular or adrenal steroidogenesis, reversible alopecia occurs after several months of ttt with high doses. 6- Voriconazole, Ravuconazole, Posaconazole New Triazoles have activity against aspergillose and Fluconazole- resistant strains of candida Krusei, albicans, glabrata. Posaconazole is the only drugs that acts against zygomycetes. It has a long side chains that appear to stabilize binding to mutated cyp51a1. 7- Amp B: dose and duration should be individulized. Pt stable, no evidence of deep-seated inf =>0.3mg/Kg/d at least 14d Pt unstable, have deep..( organ involvement) =>0.5-0.6mg/Kg/d for at least 14d Pt developp septic shock =>1mg/Kg/d Max doses 2-4g Lean body mass Initial T1/2=24-48h; terminal T1/2= 15days => practice of every other day, (0.5mg/kg/d or 1mg/kg qod) Based on the potential for reduce nephrotoxicity Faster infusion rates (< 4-6h) r associated w : *Earlier onset of infusion-related reaction ( fever, chills, headache, vomiting..) *Cardiac arrythmias (high serum [Amp] can precipitate severe cardiac adverse events most often in pt who r anuric or have previous cardiac disease, therefore we should do ECG.) The dose- related side effects is renal damage, that manifests by: -azotemia -HypoK+ -HypoMgnesimia Amp B related renal toxicity is reversible within 2w after therapy has been discontinued. Adm of NS 250ml bfr AmpB can reduce nephrotoxicity Should not mix w NS bcs Na causes Ampb to precipitate into Iv admixture. Anemia is associated w decrease renal production of erythropoietine; it is resolve after discontinuation of AmpB; it need not to be treated. No need dose adjustment w chronic reanl or hepatic failure (5-10% is eliminated in urine and bile, it is cleared by reticuloendothelial system). 8- Cancidas is metabolised and excreted 35% in feces, and 41% in urine. No adjustment is necessary for pt w renal insufficiency. Monitor liver fct test( surtout if used w cyclosporin where it increased by 2-3 fold) May cause histamine release (rash, facial swelling) Slow infusion 1h Lipid form of Amp B: is indicated for treatment of invasive fungal infections in pt who r refractory to or intolerant of conventional amp B. They r less toxic, more potent. Abelcet, Ambisome Antifungal CNS penetration IV amp B have a limited penetration into CSF bcs of high bound to lipid([ ampB] 2-4% of the serum conc) Intraventricular or intrathecal adm (0.25-0.5mg diluted w 5ml glucose5% Flucytosine might be alternative to ampB (74% of serum conc) Fluconazole (60% of serum conc) at dose 400mg/d Relapse is high when fluc. is stopped In pregnancy Azoles are teratogenic (factor c) Griseofulvin and flucytosin are teratogenic (factorc) Amp B ( factor b) has been the mainly drug used in pregnancy for the treatment of systemic mycoses. Terbinafine (factor b), ( ther have been no reports of the use of terbinafine in pregnancy.