* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hypersensitivity Reactions and Methods of Detection
Rheumatic fever wikipedia , lookup
Innate immune system wikipedia , lookup
Immunocontraception wikipedia , lookup
Immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Anti-nuclear antibody wikipedia , lookup
Duffy antigen system wikipedia , lookup
DNA vaccination wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Autoimmunity wikipedia , lookup
Adaptive immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Food allergy wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Molecular mimicry wikipedia , lookup
Monoclonal antibody wikipedia , lookup
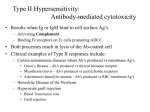
Polyclonal B cell response wikipedia , lookup
1 Hypersensitivity Reactions and Methods of Detection David Marc, B.Sc.a, & Kelly Olson Ph.Da. a NeuroScience, Inc., 373 280th St., Osceola, WI 54020, United States [email protected] ABSTRACT Hypersensitivity reactions are classified into four groups (Type I, II, III, and IV), each characterized by specific biological actions. Research has focused on understanding each hypersensitvity to ensure appropriate therapeutic recommendations are made. This overview will present the defining characteristics of each hypersensitivity and examine the diagnostic methods used to determine the existence of a specific type. Type I hypersensitivities can be determined by provacation testing, immediate-type skin testing, or radioallergosorbent tests (RASTs); Type II hypersensitivities can be determined by measuring the level of IgG antibodies to specific host proteins; Type III hypersensitivities may be detected with serum IgG antibody testing to specific antigens; Type IV hypersensitivities are determined by delayed skin testing or memory lymphocyte immunostimulation assay (MELISA®). Persistent antigen exposure may contribute to chronic conditions such as autoimmune diseases, irritable bowel syndrome, asthma, or even psychiatric illnesses. Through the effective detection of potential hypersensitivities, a patient’s quality of life can be improved through consequent antigen avoidance. crystallizable (Fc) receptors, to induce degranulation (Yamasaki & INTRODUCTION A hypersensitivity reaction refers to a state of altered Saito, 2005). Mast cell degranulation can lead to the release of reactivity in which the body mounts an amplified immune response inflammatory mediators including histamine, proteoglycans, serine to a substance. proteases, and leukotrienes (Yamasaki & Saito, 2005). In 1963, Gell and Coombs classified The hypersensitivity reactions into four different groups (Types I, II, immediate release of these inflammatory mediators can produce III, and IV) which depended upon the severity and latency of a hives, redness, and angioedema (swelling of the lips, eyelids, reaction (Gell & Coombs, 1963). Clinically, it is difficult to throat, or tongue) in what is referred to as an anaphylactic reaction distinguish between the four types of hypersensitivities as they do (Noone & Osguthorpe, 2003). In some cases, the anaphylactic not necessarily occur in isolation from each other. Biologically, reaction can be severe enough to block airways or cause heart Types I, II, and III hypersensitivities are mediated by antibodies, arrhythmias (Noone & Osguthorpe, 2003). whereas, Type IV is mediated by T cells and macrophages Type II hypersensitivities, also known as cytotoxic Hypersensitivities can only manifest hypersensitivities, are rare reactions that are typically caused by following a second or subsequent contact with a particular antigen. IgG and IgM antibodies (Brostoff et al., 1991). A Type II response Recently, extensive research has been conducted to determine may occur when the target antigen is part of the surface of a optimum treatments and to define the specific mechanisms that specific host cell or tissue (Figure 1B). Type II hypersensitivities mediate each type of hypersensitivity. This overview will define can be associated with autoimmune diseases, drug reactions, and the different types of hypersensitivities and examine different transplantations (Brostoff et al., 1991). Biochemically, Type II methods to detect hypersensitivity responses. reactions occur when IgG and IgM antibodies bind to host cells (Brostoff et al., 1991). and tissues to form complexes that activate the complement TYPES OF HYPERSENSITIVITY Typically, hypersensitivities are classified into four different types. Type I hypersensitivity is an immediate immune reaction to an antigen (Sicherer & Leung, 2009). Mast cells and basophils play an integral role in Type I hypersensitivity reactions. Following exposure to an antigen, mast cells and basophils go through a process called degranulation, where they release substances that induce inflammation (Figure 1A). Specifically, antigens interact with IgE molecules that are bound to high affinity receptors on the surface of mast cells, called fragment ©NeuroScience, Inc. December, 2009 pathway which, in turn, eliminates the host cells (Brostoff et al., 1991; Kornbrust et al., 1989). During Type II hypersensitivities, mediators of acute inflammation, such as B cells, antibodies, and cytokines are generated to induce cell lysis and death. For example, a Type II reaction may occur when a drug binds to host cells, such as red blood cells, causing them to be recognized as foreign pathogens. This will induce B cell proliferation and antibody production as well as activate the complement system which will ultimately trigger cell death (Kornbrust et al., 1989). A Type II reaction may take several hours to a full day to develop. 2 Type III hypersensitivities are also mediated by IgG and IgM antibodies (Table 1). Unlike a Type II response, Type III hypersensitivity is associated with responses to soluble antigens Figure 1. A. B. Type I Hypersensitivity Type II Hypersensitivity that are not combined with host tissues but with antibodies in the IgG Antibody IgE Antibody blood which can then lead to inflammatory responses (Brostoff et Antigen al., 1991). As the number of antigen-antibody complexes increase, Mast Cell Fc Receptor T Cell they can deposit in joints and various tissues such as kidneys, skin, and eyes leading to an inflammatory response wherever they Complement precipitate (Ellsworth et al., 2008). Research has suggested that Histamine and other mediators Type III reactions may contribute to certain systemic diseases such as systemic lupus erythematosus (SLE), serum sickness, and C. Type III Hypersensitivity Host Cell D. Antigen Type IV Hypersensitivity farmer lung (Coico & Sunshine, 2009). A Type III reaction can Antigen Presenting Cell IgG Antibody take hours, days, or even weeks to develop. Type IV hypersensitivities are referred to as delayedtype hypersensitivities because a reaction can typically take 12 or more hours to develop (Brostoff et al., 1991). Type IV responses Antigen Antigen Immune Complexes Deposited in Tissue Systemic Inflammation are dependent on T cell interactions, which recruit other cells to the site of exposure (Brostoff et al., 1991). Upon an initial antigen exposure, naive T cells differentiate into memory T cells which are Tissue Destruction Host Tissue Activation Cytokine Secretion T Cell Proliferation specific to that antigen. The memory T cells remain dormant until a subsequent exposure of the antigen elicits a faster and stronger Type I hypersensitivity reactions are traditionally immune response than the first encounter. Upon future encounters recognized through provocation testing or immediate-type skin with the given antigen, memory T cells immediately proliferate testing (Table 1). Provocation testing involves a masked topical and differentiate into effector cells to quickly eliminate the antigen. challenge of certain antigens followed by observation of the Contact dermatitis is commonly caused by a Type IV reaction in patient’s dermal responses (Smith, 1992). Clinically, the which lymphocyte production can produce local inflammation, provocation testing can pose a danger since some antigens may such as a rash, which characterizes this skin condition (Nosbaum et result in a severe anaphylactic reaction (Smith, 1992). Skin testing al., 2009). is an alternative method which may include skin pricks or patches of to determine hypersensitivity. Both the prick test and scratch test hypersensitivity in which granulomas, a ball-like collection of Recent literature proposes a fifth type involves pricking the skin with a needle or pin containing a small macrophages and epitheloid cells, are formed to encapsulate and amount of the antigen. A patch test is conducted by applying a isolate a pathogen (Rajan, 2003; Tercelj et al., 2008). Granulomas patch that contains known antigens to the skin (Williams et al., are formed in response to antigens that escape the early phases of 1992). If there is a visual reddening or swelling at the prick or an immune response and are often times related to a delayed-type patch site, the patient is considered allergic to that antigen hypersensitivity (Tercelj et al., 2008). (Williams et al., 1992). Type I hypersensitivity reactions can also Although hypersensitivity reactions appear to be be determined via radioallergosorbent tests (RASTs), which detect deleterious, they do serve the purpose to protect the human body the amount of IgE antibodies that react with suspected or known through the isolation and elimination of specific antigens. Still, allergens (Primeau & Adkinson, Jr., 2001; Williams et al., 1992). identification of hypersensitivity reactions can be beneficial for If a RAST indicates a high level of IgE to a specific antigen, the helping patients to avoid reactive antigens and to limit deleterious person is said to be allergic to that antigen (Primeau & Adkinson, actions, which will decrease the risk of developing chronic Jr., 2001). diseases (Rajan, 2003). include leuokocyte histamine release assays, surface markers for Other methods to detect a Type I hypersensitivity basophil activation, and leukotriene release tests (for review see METHODS TO IDENTIFY HYPERSENSITIVITY Primeau & Adkinson, Jr., 2001). Various methods exist to determine the existence and Type II hypersensitivity reactions are mediated by IgM types of hypersensitivity. A summary of methods to detect Type I, and IgG antibody responses to host tissues (Table 1). For instance, II, III, and IV is provided. Goodpasture syndrome is an autoimmune disease characterized by ©NeuroScience, Inc. December, 2009 3 inflammation of the glomeruli in the kidneys and hemorrhaging of lymphocyte transformation test, called memory lymphocyte the lungs (Salama et al., 2001). The measurement of IgG immuno-stimulation assay (MELISA®), is available for healthcare antibodies to glomerular basement membrane (anti-GBM) is used practitioners and can assist in the detection of Type IV to diagnose Goodpasture syndrome (Salama et al., 2001). In hypersensitivities, as previously described (Valentine-Thon et al., addition, anti-neutrophil cytoplasmic IgG antibodies (ANCAs) are 2006; Stejskal et al., 1996). In summary, a standard number of used to detect various autoimmune disorders that may be lymphocytes, with the exclusion of monocytes, are isolated from associated with Type II hypersensitivities (Radice & Sinico, 2005). whole blood specimens for cell culture. Most common Type II reactions occur in transplant and blood cultured for 5 days then transferred to new plates containing transfusion patients where the reaction is determined by a tissue known antigens, which are then pulsed for 4 hours with methyl-3H- biopsy or by monitoring a patient’s signs and symptoms. thymidine to quantify cell proliferation. A negative control is also The lymphocytes are Although limited data exists about methods for the obtained via lymphocytes from the same patient, which is not detection of Type III hypersensitivity reactions, some suggest added to antigens. After culture, the lymphocytes are harvested serum IgG antibody testing can be utilized (Table 1; Shamberger, onto filter paper and dried. The radioactivity present on the filter 2008; Stapel et al., 2008). Research on food sensitivities suggests paper is measured in a liquid scintillation counter. A stimulation that the use of enzyme-linked immunosorbent assays (ELISA) can index (SI) is calculated by dividing the counts per minute (cpm) in be effectively used to detect IgG antibodies to specific dietary the test well to the average cpm in the negative control wells proteins (Shamberger, 2008). Specifically, an increased titer of (Valentine-Thon et al., 2007; Valentine-Thon & Schiwara, 2003; IgG antibodies to a specific dietary protein would be indicative of Stejskal et al., 1996). A positive reaction, indicating Type IV a Type III hypersensitivity to that protein (Scott et al., 1990). hypersensitivity, is defined as a SI greater than 3 and an equivocal Cessation from eating the reactive food would therefore be reaction is a SI between 2 and 3. A SI less than 2 is considered recommended. However, further research is warranted to verify negative. Clinically, MELISA® has been proven to be an serum IgG antibody testing as a method to detect Type III hypersensitivities. effective tool for the determination of sensitivities to various In recent years, methods have been developed and refined to detect Type IV hypersensitivities (Table 1). metals (Valentine-Thon & Schiwara, 2003) and to bacterial antigens such as Borrelia burgdorferi (Valentine-Thon et al., Historically, the role of T cells in hypersensitivity reactions has 2007). been neglected; however, recent research has clarified and intelligently choose to remove or avoid various cleaning analyzed the role of T cells in hypersensitivity, which has provided chemicals, drugs, foods, dental amalgams, jewelry, or cosmetics a better understanding of delayed-type reactions (Primeau & that contain the hypersensitive antigens (Valentine-Thon et al., Adkinson, Jr., 2001). Two primary methods exist to verify a Type 2006; Pichler & Tilch, 2004a). Also, appropriate decisions or IV hypersensitivity in patients: 1) delayed skin testing and 2) alternative methods of treatment can be developed for patients that lymphocyte transformation tests (Primeau & Adkinson, Jr., 2001). may have hypersensitivities to antigens found in bacteria or Ultimately, patients who possess hypersensitivities can Delayed skin testing is similar to an immediate-type prostheses (Valentine-Thon et al., 2007; Stejskal et al., 2006; skin test however the reaction is typically read after 24 or 72 hours Hallab et al., 2005). MELISA® testing may prove to be an rather than 15 minutes after application of the antigens (Li, 2002). invaluable tool for the determination of contributing factors to Still, skin testing can pose the risk of developing adverse systemic persistent conditions so appropriate treatment may be achieved. reactions and appropriate training and care must therefore be practiced to ensure the safety of patients (Reid et al., 1993). In addition, research has shown that skin testing may be unreliable for some antigens, such as food allergens (Sampson & Albergo, 1984). Due to the limitations of skin testing (Rietschel, 1996), alternative Table 1. Type I II methods are currently being tested for the detection of Type IV hypersensitivities including such methods as lymphocyte III The lymphocyte transformation test is an in vitro assay IV transformation tests (Pichler & Tilch, 2004b). that measures the proliferation of T cells following an antigen challenge (Warrington & Tse, 1979). An enhanced version of the ©NeuroScience, Inc. December, 2009 Description An immediate reaction that can result in an anaphylactic reaction Cytotoxic reaction mediated by IgM and IgG antibody responses to host tissue IgG and IgM antibodies form immune complexes with antigens in the blood Delayed reaction that is mediated by memory T cells Method of Detection Provocation test, Skin test, IgE RAST IgG serum test IgG serum test Skin test, MELISA® 4 Radice, A. & Sinico, R. A. (2005). Antineutrophil cytoplasmic antibodies (ANCA). Autoimmunity, 38, 93103. COMPARING HYPERSENSITIVITY TO TOXICITY Hypersensitivity and toxicity appear to be two related events, yet they are two distinct responses that can occur in isolation of each other. Hypersensitivity reactions can transpire after acute contact with an antigen, whereas toxicity is a harmful reaction that may occur with exposure to excessive amounts of a substance (Hallab et al., 2005). To explain further, hypersensitivity can occur without a toxic reaction because a hypersensitive response is not dose-dependent and can take place Rajan, T. V. (2003). The Gell-Coombs classification of hypersensitivity reactions: a re-interpretation. Trends Immunol., 24, 376-379. Reid, M. J., Lockey, R. F., Turkeltaub, P. C., & Platts-Mills, T. A. (1993). Survey of fatalities from skin testing and immunotherapy 1985-1989. J.Allergy Clin.Immunol., 92, 6-15. Rietschel, R. L. (1996). Reproducibility of patch-test results. Lancet, 347, 1202. Roy-Byrne, P. P., Davidson, K. W., Kessler, R. C., Asmundson, G. J., Goodwin, R. D., Kubzansky, L. et al. (2008). Anxiety disorders and comorbid medical illness. Gen.Hosp.Psychiatry, 30, 208225. Salama, A. D., Levy, J. B., Lightstone, L., & Pusey, C. D. (2001). Goodpasture's disease. Lancet, 358, 917920. Sampson, H. A. & Albergo, R. (1984). Comparison of results of skin tests, RAST, and double-blind, placebo-controlled food challenges in children with atopic dermatitis. J.Allergy Clin.Immunol., 74, 26-33. with very low levels of an antigen (Stejskal & Stejskal, 1999). Scott, H., Fausa, O., Ek, J., Valnes, K., Blystad, L., & Brandtzaeg, P. (1990). Measurements of serum IgA and IgG activities to dietary antigens. A prospective study of the diagnostic usefulness in adult coeliac disease. Scand.J.Gastroenterol., 25, 287-292. Therefore, if a patient presents with a hypersensitivity reaction, Shamberger, R. (2008). Types of Food Allergy Testing. Townsend Letter, January, 71-72. even small amounts of the antigen may result in health problems Sicherer, S. H. & Leung, D. Y. (2009). Advances in allergic skin disease, anaphylaxis, and hypersensitivity reactions to foods, drugs, and insects in 2008. J.Allergy Clin.Immunol., 123, 319-327. emphasizing the importance of antigen avoidance. Smith, T. F. (1992). Allergy testing in clinical practice. Ann.Allergy, 68, 293-301. Spiller, R. C. (2004). Irritable bowel syndrome. Br.Med.Bull., 72, 15-29. Stapel, S. O., Asero, R., Ballmer-Weber, B. K., Knol, E. F., Strobel, S., Vieths, S. et al. (2008). Testing for IgG4 against foods is not recommended as a diagnostic tool: EAACI Task Force Report. Allergy, 63, 793-796. CONCLUSION Hypersensitivity reactions are common yet they aren’t often considered in treatment regimens. Untreated hypersensitivities can contribute to a myriad of conditions including autoimmune diseases (Valenta et al., 2009), irritable bowel syndrome (Spiller, 2004), asthma (Fernandez-Nieto et al., 2006), and psychiatric illnesses (Roy-Byrne et al., 2008). By Stejskal, J. & Stejskal, V. D. (1999). The role of metals in autoimmunity and the link to neuroendocrinology. Neuro.Endocrinol.Lett., 20, 351-364. Stejskal, V., Hudecek, R., Stejskal, J., & Sterzl, I. (2006). Diagnosis and treatment of metal-induced sideeffects. Neuro.Endocrinol.Lett., 27 Suppl 1, 7-16. Stejskal, V. D., Forsbeck, M., Cederbrant, K. E., & Asteman, O. (1996). Mercury-specific lymphocytes: an indication of mercury allergy in man. J.Clin.Immunol., 16, 31-40. Tercelj, M., Salobir, B., & Rylander, R. (2008). Microbial antigen treatment in sarcoidosis--a new paradigm? Med.Hypotheses, 70, 831-834. Valenta, R., Mittermann, I., Werfel, T., Garn, H., & Renz, H. (2009). Linking allergy to autoimmune disease. Trends Immunol., 30, 109-116. utilizing appropriate techniques to determine the existence of Valentine-Thon, E., Ilsemann, K., & Sandkamp, M. (2007). A novel lymphocyte transformation test (LTTMELISA) for Lyme borreliosis. Diagn.Microbiol.Infect.Dis., 57, 27-34. hypersensitivity reactions, patients can become better aware of Valentine-Thon, E., Muller, K., Guzzi, G., Kreisel, S., Ohnsorge, P., & Sandkamp, M. (2006). LTTMELISA is clinically relevant for detecting and monitoring metal sensitivity. Neuro.Endocrinol.Lett., 27 Suppl 1, 17-24. which antigens to avoid. Ultimately, by minimizing exposure to potential antigens patients may decrease the likelihood of Valentine-Thon, E. & Schiwara, H. W. (2003). Validity of MELISA for metal sensitivity testing. Neuro.Endocrinol.Lett., 24, 57-64. developing chronic diseases and therefore increase their quality of Warrington, R. J. & Tse, K. S. (1979). Lymphocyte transformation studies in drug hypersensitivity. Can.Med.Assoc.J., 120, 1089-1094. life. Williams, P. B., Dolen, W. K., Koepke, J. W., & Selner, J. C. (1992). Comparison of skin testing and three in vitro assays for specific IgE in the clinical evaluation of immediate hypersensitivity. Ann.Allergy, 68, 35-45. REFERENCES Yamasaki, S. & Saito, T. (2005). Regulation of mast cell activation through FcepsilonRI. Chem.Immunol.Allergy, 87, 22-31. Brostoff, J., Scadding, G. K., Male, D., & Roitt, I. M. (1991). Introduction to Immune Responses. In J.Brostoff, G. K. Scadding, D. Male, & I. M. Roitt (Eds.), Clinical Immunology ( New York: Gower Medical Publishing. Coico, R. & Sunshine, G. (2009). Hypersensitivity: Types II and III. In R.Coico & G. Sunshine (Eds.), Immunology: A short course (6th ed., pp. 237-245). New Jersey: John Wiley & Sons. Ellsworth, J. L., Maurer, M., Harder, B., Hamacher, N., Lantry, M., Lewis, K. B. et al. (2008). Targeting immune complex-mediated hypersensitivity with recombinant soluble human FcgammaRIA (CD64A). J.Immunol., 180, 580-589. Fernandez-Nieto, M., Quirce, S., Carnes, J., & Sastre, J. (2006). Occupational asthma due to chromium and nickel salts. Int.Arch.Occup.Environ.Health, 79, 483-486. Gell, P. G. H. & Coombs, R. R. A. (1963). The classification of allergic reactions underlying disease. In R.R.A.Coombs & P. G. H. Gell (Eds.), Clinical Aspects of Immunology ( Blackwell Science. Hallab, N. J., Anderson, S., Stafford, T., Glant, T., & Jacobs, J. J. (2005). Lymphocyte responses in patients with total hip arthroplasty. J.Orthop.Res., 23, 384-391. Kornbrust, D., Eydelloth, R., & Garratty, G. (1989). Investigations of the potential for five beta-lactam antibiotics to elicit type II hypersensitivity reactions in rats and monkeys. Fundam.Appl.Toxicol., 12, 558-566. Li, J. T. (2002). Allergy testing. Am.Fam.Physician, 66, 621-624. Noone, M. C. & Osguthorpe, J. D. (2003). Anaphylaxis. Otolaryngol.Clin.North Am., 36, 1009-20, ix. Nosbaum, A., Vocanson, M., Rozieres, A., Hennino, A., & Nicolas, J. F. (2009). Allergic and irritant contact dermatitis. Eur.J.Dermatol., 19, 325-332. Pichler, W. J. & Tilch, J. (2004a). The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy, 59, 809-820. Pichler, W. J. & Tilch, J. (2004b). The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy, 59, 809-820. Primeau, M. N. & Adkinson, N. F., Jr. (2001). Recent advances in the diagnosis of drug allergy. Curr.Opin.Allergy Clin.Immunol., 1, 337-341. 091230-GEN-Z1109 ©NeuroScience, Inc. December, 2009