* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Increased carrier prevalence of deficient CYP2C9, CYP2C19 and
Biology and consumer behaviour wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Hardy–Weinberg principle wikipedia , lookup
Human genetic variation wikipedia , lookup
Gene therapy wikipedia , lookup
Genetic drift wikipedia , lookup
Population genetics wikipedia , lookup
History of genetic engineering wikipedia , lookup
Genomic imprinting wikipedia , lookup
Epigenetics of human development wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Public health genomics wikipedia , lookup
Genome (book) wikipedia , lookup
Gene expression profiling wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Dominance (genetics) wikipedia , lookup
Designer baby wikipedia , lookup
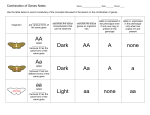
PERSONALIZED MEDICINE IN ACTION Increased carrier prevalence of deficient CYP2C9, CYP2C19 and CYP2D6 alleles in depressed patients referred to a tertiary psychiatric hospital Objective: This study compared the types and carrier prevalences of clinically significant DNA polymorphisms in the cytochrome P450 (CYP450) genes CYP2C9, CYP2C19 and CYP2D6 in major depressive disorder patients with a control group of nonpsychiatrically ill, medical outpatients. Method: We conducted a case–control study using 73 psychiatric outpatients diagnosed with depression and referred to a tertiary center, The Institute of Living (Hartford, CT, USA), for treatment resistance or intolerable side-effects to psychotropic drugs. The controls were 120 cardiovascular patients from Hartford Hospital being treated for dyslipidemia but otherwise healthy and not psychiatrically ill. DNA typing to detect polymorphisms in the genes CYP2C9, CYP2C19 and CYP2D6 was accomplished with the Tag-It™ mutation detection assay and the Luminex xMAP® system. Results: The percentage of individuals in psychiatric versus control groups with two wild-type alleles for CYP2C9, CYP2C19 and CYP2D6 genes, were 50 versus 74% (p < 0.001), 71 versus 73% (not statistically significant) and 36 versus 43% (trend, p < 0.2), respectively. Within the psychiatric population, 57% of individuals were carriers of non-wild-type alleles for 2–3 genes, compared with 36% in the control population (p < 0.0001). The balance, 43% in the psychiatric population and 64% in the control, were carriers of non-wild-type alleles for none or one gene. Conclusions: These findings reveal that clinically relevant CYP2C9 polymorphisms occur more frequently in depressed psychiatric patients than in nonpsychiatric controls. The same trend was found for polymorphisms in the CYP2D6 gene. We found a significant cumulative metabolic deficiency in the psychiatric population for combinations of the CYP2C9, CYP2C19 and CYP2D6 genes. The significant enrichment of CYP2C9-deficient alleles in the psychiatric population validates a previously reported association of this gene with the risk for depression disorders. The high prevalence of carriers with deficient and null alleles suggests that CYP450 DNA typing may play a role in the management of psychiatric patients at tertiary care institutions. KEYWORDS: alleles, CYP2D6, CYP2C9, CYP2C19, drug metabolism, patient safety, pharmacogenetics, psychotropic drug safety Major depressive disorder (MDD) is currently the leading cause of disability in North America as well as other countries and, according to the WHO, may become the second leading cause of disability worldwide (after heart disease) by the year 2020 [1] . Over the years, the elusive and highly variable nature of psychiatric disorders has led to drug therapy treatment that largely relies on empiricism to ascertain individual patient differences. This empirical approach has resulted in a high rate of refractory and adverse responses to drug therapies, rendering treatment of MDD one of the most significant challenges in psychiatry. Both published literature studies and clinical experience reveal great variability in an individual’s response to psychotropic drug treatment with regards to drug metabolism, side effects and efficacy [2–4] . This variability is in part attributable to genetic differences that result in slowed or accelerated oxidation of many psychotropic drugs metabolized by the cytochrome P450 (CYP450) isoenzyme system in the liver [5–7] . In particular, clinically relevant variants have been identified for the isoenzymes coded by the CYP2C9, CYP2C19 and CYP2D6 genes. While the pharmacogenetic significance of CYP2C9-deficient alleles is not as prominent in psychiatry as that of CYP2D6 and CYP2C19, it is known that the gene represents a minor metabolic pathway for some antidepressants [5] . Therefore, polymorphisms in CYP2C9 may be important in psychiatric patients deficient for other CYP450 enzymatic activities [8] . Some of the potential consequences of polymorphic drug metabolism are extended pharmacological effect, adverse drug reactions (ADRs), lack of prodrug activation, drug toxicity, increased or decreased effective dose, metabolism by alternative deleterious pathways and exacerbated drug– drug interactions [9,10] . CYP450 isoenzymes are also involved in the metabolism of endogenous substrates, including neurotransmitter amines, and have been implicated in the pathophysiology 10.2217/17410541.5.6.579 © 2008 Future Medicine Ltd Personalized Medicine (2008) 5(6), 579–587 Gualberto Ruaño1†, David Villagra1, Umme Salma Rahim2, Andreas Windemuth1, Mohan Kocherla1, Bruce Bower1, Bonnie L Szarek2 & John W Goethe 2 † Author for correspondence: Genomas, Inc., 67 Jefferson Street, Hartford, CT 06107 USA; Tel.: +1 860 545 3773; Fax: +1 860 545 4575; [email protected] 2 Institute of Living, Hartford Hospital, Hartford CT, USA 1 ISSN 1741-0541 579 PERSONALIZED MEDICINE IN ACTION Ruaño, Villagra, Rahim et al. of mood disorders. CYP2D6 activity has been associated to personality traits and CYP2C9 to MDD [11,12] . The CYP2D6 gene product metabolizes several antipsychotics (e.g., aripiprazole and risperidone) and antidepressants (e.g., duloxetine, paroxetine and venlafaxine) [9] . CYP2D6 is highly polymorphic. More than 60 alleles and more than 130 genetic variations have been described for this gene, located on chromosome 22q13 [9,101] . Clinically, the most significant phenotype is the null metabolizer, which has no CYP2D6 activity because it has two nonfunctional CYP2D6 alleles or is missing the gene altogether. The prevalence of null metabolizers is approximately 7% in Caucasians and 1–3% in other races [2,9,13] . Gene duplications of CYP2D6 that may lead to an ultra-rapid metabolizer (UM) phenotype are also clinically significant. A recent worldwide study suggested that up to 40% in some North African and more than 20% in Australian populations are CYP2D6 UMs [14] . In a 2006 US survey, the prevalence of CYP2D6 UMs was 1–2% in Caucasians and African–Americans [2] . CYP2C9 is located on chromosome 10q24, and its gene product is involved in the metabolism of several important psychoactive substances (e.g., fluoxetine, phenytoin, sertraline and tetrahydrocannabinol) [11,15] . It has been reported that CYP2C9 activity is modulated by endogenous substrates such as adrenaline and serotonin [16] . CYP2C19 is also located on chromosome 10q24, but in linkage equilibrium with CYP2C9. Its gene product is involved in the metabolism of various antidepressants (e.g., citalopram and escitalopram). For some psychotropics, a cumulative deficit in drug metabolism resulting from multigene polymorphisms in CYP2D6, CYP2C9 and CYP2C19 may be clinically significant. For example, gene products for CYP2C19 and CYP2D6 provide joint drug-metabolism pathways for various tricyclic antidepressants (e.g., amitriptyline and imipramine) [6] . Given that CYP2D6, CYP2C9 and CYP2C19 genes are not linked physically or genetically, their polymorphisms would be expected to segregate independently in populations. Pharmacogenetics is a discipline that attempts to correlate specific gene variations with responses to particular drugs. Such DNA-guided pharmacotherapy would be potentially cost effective and could spare patients from unwanted side effects by matching each with the most suitable, individualized drug and dosing regimen at initiation of pharmacotherapy. There have been strategies personalizing dosing for psychiatric drugs according to algorithms derived from studies of 580 Personalized Medicine (2008) 5(6) blood levels [6] . Beyond pharmacogenetics, it has become apparent that therapeutic index is a necessary concept in understanding how CYP450 polymorphism may inf luence personalized prescription [17] . A 1998 meta-ana lysis of 39 prospective studies in US hospitals estimated that 106,000 Americans die annually from ADRs [18] . Adverse drug events are also common (50 per 1000 person years) among ambulatory patients, particularly the elderly on multiple medications. The 38% of events classified as ‘serious’ are also the most preventable [19] . It is now clear that virtually every pathway of drug metabolism, transport and action is susceptible to gene variation [20] . Within the top 200 selling prescription drugs, 59% of the 27 most frequently cited in ADR studies are metabolized by at least one enzyme known to have gene variants that code for reduced or nonfunctional proteins [21] . In psychiatry, the high carrier prevalence of deficient CYP450 alleles has significant implications for healthcare management. Uninformed prescribing of psychotropics to individuals with highly compromised biochemical activity for the CYP450 isoenzymes, may expose 50% of patients to preventable severe side effects. In this study, the majority of psychiatric patients (57/73) were taking two or more psychotropic medications at the time of the study. If these patients were carriers of gene polymorphisms resulting in deficient psychotropic metabolism, their risk of adverse drug effects would substantially increase. Were DNA typing to be performed upon admission, such information could guide pharmacotherapy during hospitalization and after. The value of DNA typing for diagnosing severe drug side effects and treatment resistance has been documented in various case reports [8,22] . While it is well known that interindividual variation in drug metabolism is highly dependent on inherited gene polymorphisms, the debate regarding the role of genotyping in clinical practice continues. The aim of the current study was to compare the carrier prevalence of CYP2C9, CYP2C19 and CYP2D6 polymorphisms in psychiatric patients and controls in order to support DNA typing as a clinical tool for antidepressant management at a tertiary referral center. Methods Patient cohorts The study sample consisted of 73 psychiatric patients (48% male and 52% female, aged 5–86 years with a median age of 22 years) suffering from a MDD and treated with psychotropic future science group CYP450 genotyping in psychiatric referrals medication through the outpatient psychiatric services at The Institute of Living at Hartford Hospital (CT, USA). They were referred to the Laboratory of Personalized Health at Genomas (CT, USA) for CYP450 diagnostic genotyping as part of their clinical care because of efficacy or safety problems related to their medications. Self-reported ethnicities were 92% Caucasian, 5% African–American, 1.5% Hispanic and 1.5% Asian. The control sample consisted of 120 medical patients treated with statins at Hartford Hospital [23] . They were genotyped for CYP2C9, CYP2C19 and CYP2D6 in a recent survey of the prevalence of drug-metabolism deficiencies [24] . The patients provided informed written consent as approved by the Institutional Review Board of Hartford Hospital. Ages of patients ranged between 40 and 80 years; 63% were males and 37% were females. The self-reported ethnicities were 87% Caucasian, 3% African–American, 9% Hispanic and 1% Asian. CYP450 DNA typing data were obtained for all 73 psychiatric patients on CYP2D6, and for 72 patients on CYP2C9 and CYP2C19. Among controls, genotyping data was obtained for 120 patients on CYP2C9 and CYP2C19, and for 92 patients on CYP2D6, the difference attributable to specific gene assay yields. Data regarding CYP450 DNA polymorphisms in the control population have been previously published [24] . SNP assays Blood samples were collected into tubes containing either ethylenediamine tetra-acetic acid (EDTA) or citrate and were extracted from lymphocytes using the Qiagen (West Sussex, UK) EZ-1 robotic DNA isolation procedure. DNA typing was performed at the Genomas Laboratory of Personalized Health (LPH) at Hartford Hospital. LPH is a high-complexity clinical DNA testing center licensed by the Connecticut Department of Public Health (CL0644) and certified by the Centers for Medicare and Medicaid Services (ID #07D1036625) under Clinical Laboratory Improvement Amendments (CLIA). The Tag-It™ Mutation Detection assays (Luminex Corporation, TX, USA) were utilized for DNA typing of 14, 5 and 7 alleles in genes CYP2C9, CYP2C19 and CYP2D6, respectively, as previously described [25,26] . These assays employed PCR to amplify selectively the desired gene without co-amplifying pseudogenes or other closely related sequences. In addition, the kit employs a PCR strategy to amplify fragments future science group PERSONALIZED MEDICINE IN ACTION characteristic of unique genomic rearrangements in order to detect the presence of the deletion and duplication alleles in these genes. The kits use multiplexed allele-specific primer extension (ASPE) to identify small nucleotide variations including single-base changes and deletions of one or three bases on the Luminex xMAP® system (Luminex Corporation, TX, USA) [26] . Allele categorization We classified the alleles into clinically distinct categories for each of the three genes examined as null, deficient, functional or ultra based on well-defined molecular properties of the altered gene [24] . Null alleles lack any enzymatic activity because the altered gene does not produce a functional protein. Such null alleles include gene deletions, frameshift mutations, stop codons and splicing defects. Deficient alleles have subfunctional enzymatic activity due to nucleotide substitutions resulting in amino acid changes in the protein, and these variants may manifest subnormal enzymatic activity for some drug substrates. The functional allele refers to the genetic wild-type, the most common allele in the population with enzymatic activity considered normal. Ultra alleles exhibit increased enzymatic activity as a consequence of either gene duplication or a promoter change. TABLE 1 lists alleles detected in this study and their functional classification. To determine the combinatorial non-wild-type carrier prevalence across all three genes examined, we used the genotype data for each patient in each population and tallied the number of subjects who had variant alleles in 3, 2, 1 or no genes. Conventions for naming the alleles according to the Human Cytochrome P450 (CYP) Allele Nomenclature Committee have been followed in this study [101] . Accordingly, all variant alleles contain nucleotide changes that have been shown to affect transcription, splicing, translation, posttranscriptional or post-translational modifications or result in at least one amino acid change. Results Demographic characteristics The psychiatric and control populations differed slightly in age, and in numbers of men and women (TABLE 2) . Allele carrier status did not differ between male and female psychiatric patients (data not shown). Clinical characteristics All psychiatric patients were treated, and those psychotropic medications prescribed for three patients or more are provided in TABLE 3. www.futuremedicine.com 581 PERSONALIZED MEDICINE IN ACTION Ruaño, Villagra, Rahim et al. Table 1. Allele frequencies in control and psychiatric populations for the CYP2C9, CYP2C19 and CYP2D6 genes. Marker Control Psychiatric Gene Allele Change Phenotype Count Frequency (%) Count CYP2C9 WT *2 *3 *6 WT *2 *4 *8 Reference Arg 144 Cys Ile 359 Leu Frame shift Reference Splicing defect Start codon Trp 120 Arg Normal Deficient Deficient Null Normal Null Null Null 203 22 15 0 208 30 1 1 84.6 9.2 6.2 – 86.7 12.5 0.4 0.4 104 26 13 1 123 20 1 0 72.2 18.1 9.0 0.7 85.4 13.9 0.7 – WT Dup *2a Dup *4 *2a *5 *3 *4 *6 *9 *10 *12 *17 Reference Gene duplication (*2a) Gene duplication (*4) Promoter variant Gene deletion Frameshift Splicing defect Frameshift Lys 281 del Pro 34 Ser Gly 42 Arg Thr 107 Ile Normal Ultra Null Ultra Null Null Null Null Deficient Deficient Null Deficient 87 2 1 37 5 3 28 0 6 6 1 8 47.3 1.1 0.5 20.1 2.7 1.6 15.2 – 3.3 3.3 0.5 4.4 70 0 2 28 3 1 25 7 7 0 0 3 47.9 – 1.4 19.1 2.1 0.7 17.1 4.8 4.8 – – 2.1 CYP2C19 CYP2D6 Frequency (%) The total allele count differs among genes because of assay yields. WT: Wild-type. These drugs include antipsychotics, antidepressants and anticonvulsants. Most frequently prescribed were aripiprazole, risperidone, fluoxetine and lamotrigine. In addition, 57 patients (78%) concurrently received two or more psychotropic medications, 12 patients (16%) received only one medication, while for four patients (6%), no psychotropic medications were reported. In the case of the CYP2D6 gene, the *4 allele (null, splicing defect) was the most common null allele within both groups. Frequencies were 15.2 and 17.0% in the control and psychiatric groups, respectively. The *6 allele (a frameshift mutation) was only seen in the psychiatric group, appearing at a frequency of 4.8%. Carrier prevalences depicts the prevalence of carrier status for each of the three CYP2 genes. Noncarriers have two copies of normal alleles. Single carriers have one copy of a normal allele and one copy of a deficient or null allele. A double carrier may have two copies of deficient alleles, two copies of null alleles, or one copy each of a deficient and a null allele. Duplication of a functional allele, or homozygosity for the CYP2D6*2a allele, confers ultra-rapid metabolizer status [5] . The top panel of F IGUR E 1 illustrates the increased prevalence of CYP2C9 carrier status among the psychiatric group when compared with the control group, with 50% of the psychiatric group carrying two wild-type alleles compared with 74% of the control population (p < 0.001). The middle panel of FIGURE 1 shows no significant difference between the two populations with regards to the CYP2C19 carrier prevalence. The bottom panel of FIGURE 1 presents FIGURE 1 Allele frequencies lists the alleles of clinical significance detected in the CYP2C9, CYP2C19 and CYP2D6 genes and their frequencies for both study groups. In the CYP2C9 gene, the observed alleles in the control sample were all deficient while the patients from the psychiatric sample possessed both deficient and null alleles. The deficient *2 and *3 alleles were observed at higher frequencies in the psychiatric sample, 18.1 and 9.0%, respectively, compared with 9.2 and 6.3%, respectively, in the control group. The null (*6, frameshift mutation) allele was found in only one patient of the psychiatric group. In the CYP2C19 gene, all commonly observed alleles were null in both groups, with no significant differences between the control and the psychiatric populations. TABLE 1 582 Personalized Medicine (2008) 5(6) future science group CYP450 genotyping in psychiatric referrals the CYP2D6 allele carrier prevalence results. Of particular significance is that 43% of the control patients versus 36% of the psychiatric ones had no deficient alleles (p < 0.2). Additionally, in the psychiatric group 52% of the patients were single carriers compared with 37% of patients in the control group (p < 0.1). The prevalence of double carriers was 7 and 13% in the psychiatric and control groups, respectively. FIGURE 2 represents the differences in combinatorial carrier prevalence in CYP2C9, CYP2C19 and CYP2D6 genes between the psychiatric and control populations. As illustrated by FIGURE 2 , there is a much higher prevalence of carriers of non-wild-type alleles in two or three genes among the referred psychiatric patients than there is in the control population (p = 1.2 × 10 –5). Analysis of the genotype data results for each patient revealed that 36% of the control population had two or three genes with variant alleles resulting in deficient or null metabolism. Of those, 34% were deficient in two genes and 2% were deficient in three genes. In total, 52% of the control population had only one null or deficient gene, while 12% were wild-type for all three genes in question. In comparison, 57% of the psychiatric population possessed deficient or null alleles on more than one gene. A total of 47% had variant alleles in two genes and 10% had variant alleles in three genes. Only 6% were wild-type for all three genes and the remaining 36% had a deficient or null allele in one gene. Discussion & future perspective This study demonstrates that a psychiatric population of patients referred to a tertiary mental health center could have deficient PERSONALIZED MEDICINE IN ACTION Table 2. Patient characteristics. Control Psychiatric Sample size (n) 121 73 Age range (years) 40–80 5–86 Male 63 48 Female 37 52 Caucasian African–American 87 3 92 6 Hispanic Asian 9 1 1 1 Gender (%) Ethnicity (%) innate drug metabolism capacity. Compared with a hyperlipidemic population drawn from the same medical center, there was a significantly higher prevalence of patient carriers of subfunctional polymorphisms in the CYP2C9 and CYP2D6 genes, but not for the CYP2C19 gene. Furthermore, the study found a significant combinatorial metabolic deficiency in the psychiatric population. These genes code for isoenzymes involved in key metabolic pathways of numerous psychotropic drugs, including antidepressants such as fluoxetine and antipsychotics such as risperidone. These medications are associated with many side effects, which could be exacerbated if a patient is innately deficient for their metabolism. In addition to drug metabolism, the CYP450 isoenzymes metabolize endogenous substrates. For example, CYP2D6 is also a 3- and 4-methoxy phenylethylamine O-demethylase and a tyramine hydroxylase, both of which are pathways that lead to the endogenous Table 3. Medications given to three or more study patients. Brand name Generic name Class Abilify Risperdal® Prozac® Lamictal® Seroquel® Aripiprazole Risperidone Fluoxetine Lamotrigine Quetiapine Antipsychotic Antipsychotic Antidepressant Anticonvulsant Antipsychotic 10 8 7 7 6 Wellbutrin® Bupropion Venlafaxine Valproic acid Methylphenidate Paroxetine Oxcarbazepine Clonazepam Sertraline Topiramate Antidepressant Antidepressant Anticonvulsant Stimulant Antidepressant Anticonvulsant Anticonvulsant Antidepressant Anticonvulsant 6 6 6 5 4 4 4 3 3 ® Effexor® Depakote® Concerta® Paxil® Trileptal® Klonopin® Zoloft® Topamax® future science group www.futuremedicine.com Patients 583 PERSONALIZED MEDICINE IN ACTION Ruaño, Villagra, Rahim et al. Control Psych 5% 6% *21% *44% CYP2C9 *50% *74% 29% 27% CYP2C19 73% 71% 7% 5% 7% 13% ‡ ‡ 43% 36% CYP2D6 ‡ ‡ 37% Ultra rapid 52% Single carrier Noncarrier Double carrier Figure 1. Carrier prevalences of deficient and null alleles for CYP2C9, CYP2C19 and CYP2D6 between the control and psychiatric populations. * p < 0.001; ‡0.05 < p < 0.20. formation of dopamine [27] . CYP2C9 activity is modulated by endogenous substrates such as adrenaline, and serotonin and may be involved in the metabolism of serotonin and its metabolites in the brain [16] . The involvement of CYP2C9 in the metabolism of melatonin has also been suggested [28] . Polymorphisms in the CYP2C9 gene may interrupt or inhibit these endogenous pathways and thus contribute to susceptibility to psychiatric disorders. CYP2C9 is also involved in the metabolism of amitryptyline, fluoxetine and sertraline and its polymorphisms may contribute to altered CYP450 enzymatic activity and metabolism of such substances important for psychiatric patients [5,8] . In CYP2C9 we observed a highly significant increase (p < 0.001) in deficient alleles, specifically the CYP2C9*2 allele. These results parallel the previous report of CYP2C9*3 allele association with depression by a Spanish group [12] . Both *2 and *3 alleles are functionally deficient and are therefore both likely to reduce 584 Personalized Medicine (2008) 5(6) the metabolism of endogeneous and exogenous substrates processed by the CYP2C9 *2 and *3 gene product. Furthermore, in our study patients being treated with psychotropic drugs and evidencing treatment resistance or side effects was the main criteria for entry. In the Llerena cohort, disease diagnosis without regard to treatment outcome was the basis for enrolment. Adverse drug response phenotypes may unmask innate disease characteristics and allow genetic associations to otherwise latent phenotypes. The Institute of Living is a psychiatric tertiary care center that by virtue of its expertise treats patients with advanced mental illnesses referred from primary or secondary care centers. Such patients may not have responded positively to drug therapy or have suffered from serious side effects. By contrast, the cardiology patients at Hartford Hospital serve as a control group with regards to their disease status and ability to metabolize psychotropic drugs. These patients had been treated with statins for at least 1 month. Statins are metabolized primarily by the CYP3 family [29] . Hence, it is unlikely that these patients were selected for variants in the CYP2 family, although this possibility cannot be excluded. Considering this difference in populations, one would expect to see both a psychopathological and a pharmacotherapeutic referral bias in psychiatric patients referred to a tertiary center. The higher carrier prevalence of CYP2C9 and CYP2D6 gene variants in the psychiatric population could be attributed to either or both effects. Additionally, strong evidence for such a referral bias can be found in the data represented by FIGURE 2 , which illustrates the notable difference between the percentage of patients with non-wild-type genotypes when considering multiple genes at once. Thus, we note that patients who have been referred to a tertiary psychiatric hospital may be experiencing a high degree of adverse side effects or drug resistance in part due to a higher prevalence of polymorphisms across three CYP2 genes known to play an important role in the metabolism of psychotropic drugs. The present study has various limitations. There was no difference in CYP2C19 allele frequencies in this study between the psychiatric and control populations. CYP2C19 is less polymorphic than the other two genes, and the current study size did not provide enough statistical power to detect frequency differences. Although both populations are predominantly Caucasian, other patient demographics are future science group CYP450 genotyping in psychiatric referrals different between the psychiatric and control populations. The age range for the psychiatric patients is broader because many of the referred patients were adolescents. Since DNA is inherited and does not change with aging, adults are not expected to differ from children in the carrier prevalence of certain target SNPs. It is well known that referral psychiatric populations are disproportionately female. Reflecting clinical practice, this study does not attempt to restrict drug prescriptions or patient selection, and benefits from a naturalistic setting but at the expense of controlled conditions. Finally, the gamut of alleles for the CYP450 genes continues to expand with discovery efforts in various populations [14,30,31] . Nevertheless, we believe this study documents the prevalence of the most commonly observed ultra-rapid, deficient and null alleles for CYP2C9, CYP2C19 and CYP2D6, which are of immediate clinical relevance. We are also pursuing targeted recruitment of populations under-represented in this clinical survey, such as the Hispanic population. Recently the Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group assessed the use of CYP2C19 and CYP2D6 genotyping in adult patients beginning selective serotonin reuptake inhibitor for nonpsychotic depression [32] . This CYP2C9 • CYP2C19 • CYP2D6 Control *36% *64% Psych *43% *57% Non-wild-type alleles found in: 0–1 genes 2–3 genes Figure 2. Combinatorial CYP2C9, CYP2C19 and CYP2D6 deficiencies in control versus psychiatric populations. * p < 0.0001. future science group PERSONALIZED MEDICINE IN ACTION Group concluded that evidence was insufficient to support a recommendation for or against use of CYP450 genotyping in patients beginning selective serotonin reuptake inhibitor treatment. Notably, EGAPP did not consider CYP2C9 variability, and explicitly excluded from its purview treatment refractory or hospitalized patients. By contrast, our study included combinatorial genotyping of CYP2C9, CYP2C19 and CYP2D6, and applied it to patients referred to a tertiary psychiatry hospital because of repeated poor response and/or side effects to antidepressant therapy. Comprehensive, combinatorial genotyping and targeted applications to populations with the greatest medical need stand in sharp contrast to limited genotyping for broad population screening. In assessing the value of genotype-guided healthcare in psychiatry, it is apparent that the former scenario may be the most relevant. We believe the defi nition of a novel drugsensitivity syndrome is warranted in carriers of multiple null and defi cient alleles of CYP450 genes. We had already presented one patient in this series as a detailed case study [8] . Independently segregating alleles have the property of sporadic, nonfamilial, concurrence in an individual depending on chance. Such individuals are multiply deficient in CYP450 metabolic routes, which places them at risk for adverse reactions with several psychotropics. That 57% of referred psychiatric patients may be severely compromised in drug-metabolism capacity ascertained for two or three genes among CYP2C9, CYP2C19 and CYP2D6 should serve as a public health imperative for the wide use of DNA typing as an adjunct of psychopharmacology. As the field of personalized healthcare advances to clinical practice, we foresee DNA-guided medicine being used to prevent ADRs, particularly in high-risk populations referred to tertiary hospitals. We conclude that CYP2C9, CYP2C19 and CYP2D6 combinatorial genotyping could be useful for patients with histories of drug resistance and intolerance reactions to multiple psychotropics. As the field of pharmacogenetics advances, significant system and health economic value may materialize [33] . Genotype-guided prescription of psychotropics may prevent drug-induced morbidity in many psychiatric care settings, including treatment resistant and drug intolerant patients, as well as children and adolescents. Physicians and other healthcare providers should have an understanding of the relevance of drug-metabolism genetic polymorphisms in psychiatric practice. www.futuremedicine.com 585 PERSONALIZED MEDICINE IN ACTION Ruaño, Villagra, Rahim et al. Financial & competing interests disclosure Ruaño, Windemuth, Kocherla and Villagra are full-time employees of Genomas, Inc. Bower is a consultant to the company. Goethe, Szarek, and Rahim have no disclosures. Funds for this study were provided by Hartford Hospital grant #122959 and by Genomas internal research funds. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilized in the production of this manuscript. Executive summary CYP2C9, CYP2C19 and CYP2D6 genes play a role in the metabolism of numerous psychoactive substances. Common variants in these genes can result in deficient metabolic capacity for many psychotropic drugs and altered endogenous pathways. From the Institute of Living, a tertiary psychiatric hospital in Hartford, CT, USA, 73 outpatients were genotyped for common variants in the CYP2C9, CYP2C19 and CYP2D6 genes. The results were compared with 120 control (nonpsychiatric) cardiology patients from the same medical center genotyped for the same polymorphisms. Individuals in psychiatric versus control groups were carriers of two wild-type alleles for CYP2C9, CYP2C19 and CYP2D6 genes, as follows: 50 versus 74%, 71 versus 73%, and 36 versus 43%, respectively. Combinatorial genotype analysis revealed that 57% of individuals in the psychiatric population were carriers of multiple polymorphisms on two or three genes compared with 36% of individuals in the control population. CYP450 genotyping would allow for DNA-guided treatment in tertiary psychiatric centers and could be particularly useful for patients with treatment resistance and drug intolerance to multiple psychotropics. Bibliography 7 Susce MT, Murray-Carmichael E, de Leon J: Response to hydrocodone, codeine and oxycodone in a CYP2D6 poor metabolizer. Prog. Neuropsychopharmacol. Biol. Psychiatry 30, 1356–1358 (2006). 8 Ruaño G, Blair CL, Bower B et al.: Somatic complications of psychotropic medications in a patient with multiple CYP2 drug metabolism deficiencies. Conn. Med. 71, 197–200 (2007). 9 Ingelman-Sundberg M: Genetic polymorphisms of cytochrome P450 2D6 (CYP2D6): clinical consequences, evolutionary aspects and functional diversity. Pharmacogenomics. J. 5, 6–13 (2005). 10 11 Papers of special note have been highlighted as: of interest of considerable interest 1 2 Murray CJ, Lopez AD: Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet 349, 1498–1504 (1997). de Leon J, Armstrong SC, Cozza KL: Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychosomatics 47, 75–85 (2006). Very useful practical considerations on the clinical utility of CYP450 genotyping in psychiatry. 3 4 5 Mrazek DA: Clinical implementation of psychiatric pharmacogenomic testing. Pers. Med. 2, 93–95 (2005). Mrazek DA: Incorporating pharmacogenetics into clinical practice: reality of a new tool in psychiatry. The context of genetic testing in clinical psychiatric practice. CNS. Spectr. 11, 3–4 (2006). Black JL, III, O’Kane DJ, Mrazek DA: The impact of CYP allelic variation on antidepressant metabolism: a review. Expert Opin. Drug Metab. Toxicol. 3, 21–31 (2007). 12 Comprehensive, clinically focused treatise on psychotropic drug metabolism and the role of the CYP450 system. 6 Kirchheiner J, Nickchen K, Bauer M et al.: Pharmacogenetics of antidepressants and antipsychotics: the contribution of allelic variations to the phenotype of drug response. Mol. Psychiatry 9, 442–473 (2004). Pioneering study of genotype-guided dosing of psychotropics. 586 14 Bradford LD: CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics 3, 229–243 (2002). 15 Dahl ML: Cytochrome p450 phenotyping/ genotyping in patients receiving antipsychotics: useful aid to prescribing? Clin. Pharmacokinet. 41, 453–470 (2002). 16 Gervasini G, Martinez C, Agundez JA, Garcia-Gamito FJ, Benitez J: Inhibition of cytochrome P450 2C9 activity in vitro by 5-hydroxytryptamine and adrenaline. Pharmacogenetics 11, 29–37 (2001). Wedlund PJ, de Leon J: Cytochrome P450 2D6 and antidepressant toxicity and response: what is the evidence? Clin. Pharmacol. Ther. 75, 373–375 (2004). 17 de Leon J, Susce MT, Johnson M et al.: A clinical study of the association of antipsychotics with hyperlipidemia. Schizophr. Res. 92, 95–102 (2007). LLerena A, Edman G, Cobaleda J, Benitez J, Schalling D, Bertilsson L: Relationship between personality and debrisoquine hydroxylation capacity. Suggestion of an endogenous neuroactive substrate or product of the cytochrome P4502D6. Acta Psychiatr. Scand. 87, 23–28 (1993). 18 Lazarou J, Pomeranz BH, Corey PN: Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 279, 1200–1205 (1998). 19 Gurwitz JH, Field TS, Harrold LR et al.: Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA 289, 1107–1116 (2003). 20 Weinshilboum R: Inheritance and drug response. N. Engl. J. Med. 348, 529–537 (2003). 21 Ernst FR, Grizzle AJ: Drug-related morbidity and mortality: updating the cost-of-illness model. J. Am. Pharm. Assoc. (Wash.) 41, 192–199 (2001). 22 Johnson M, Markham-Abedi C, Susce MT, Murray-Carmichael E, McCollum S, de Leon J: A poor metabolizer for cytochromes P450 2D6 and 2C19: a case report on antidepressant treatment. CNS Spectr. 11, 757–760 (2006). LLerena A, Berecz R, Dorado P, Gonzalez AP, Penas-LLedo EM, De La Rubia A: CYP2C9 gene and susceptibility to major depressive disorder. Pharmacogenomics. J. 3, 300–302 (2003). Significant study of endogenous CYP2C9 metabolism deficiencies and potential relevance to psychiatric disease. 13 Sistonen J, Sajantila A, Lao O, Corander J, Barbujani G, Fuselli S: CYP2D6 worldwide genetic variation shows high frequency of altered activity variants and no continental structure. Pharmacogenet. Genomics 17, 93–101 (2007). Personalized Medicine (2008) 5(6) future science group CYP450 genotyping in psychiatric referrals PERSONALIZED MEDICINE IN ACTION 23 Ruaño G, Thompson PD, Windemuth A et al.: Physiogenomic analysis links serum creatine kinase activities during statin therapy to vascular smooth muscle homeostasis. Pharmacogenomics 6, 865–872 (2005). 26 Yu AM, Idle JR, Byrd LG, Krausz KW, Kupfer A, Gonzalez FJ: Regeneration of serotonin from 5-methoxytryptamine by polymorphic human CYP2D6. Pharmacogenetics 13, 173–181 (2003). 24 Ruaño G, Makowski G, Windemuth A et al.: High carrier prevalence of deficient and null alleles of CYP2 genes in a major USA hospital: implications for personalized drug safety. Pers. Med. 3, 131–137 (2006). 27 Facciola G, Hidestrand M, von Bahr C, Tybring G: Cytochrome P450 isoforms involved in melatonin metabolism in human liver microsomes. Eur. J. Clin. Pharmacol. 56, 881–888 (2001). 25 Melis R, Lyon E, McMillin GA: Determination of CYP2D6, CYP2C9 and CYP2C19 genotypes with Tag-It mutation detection assays. Expert Rev. Mol. Diagn. 6, 811–820 (2006). 28 Wilke RA, Moore JH, Burmester JK: Relative impact of CYP3A genotype and concomitant medication on the severity of atorvastatin-induced muscle damage. Pharmacogenet. Genomics 15, 415–421 (2005). Gordon J, Merante F, Weiss S, Zastawny R: Pharmacogenetic P-450 screening using the Tag-It universal bead-based array platform. In: Pharmacogenomics and Proteomics: Enabling The Practice of Personalized Medicine. Wong SH, Linder MW, Valdes R (Eds). AAC Press, Washington, DC, USA (2006). future science group 29 Cai WM, Nikoloff DM, Pan RM et al.: CYP2D6 genetic variation in healthy adults and psychiatric African–American subjects: implications for clinical practice and genetic testing. Pharmacogenomics. J. 6, 343–350 (2006). www.futuremedicine.com 30 Scott SA, Edelmann L, Kornreich R, Erazo M, Desnick RJ: CYP2C9, CYP2C19 and CYP2D6 allele frequencies in the Ashkenazi Jewish population. Pharmacogenomics 8, 721–730 (2007). 31 Recommendations from the EGAPP Working Group: testing for cytochrome P450 polymorphisms in adults with nonpsychotic depression treated with selective serotonin reuptake inhibitors. Genet. Med. 9, 819–825 (2007). 32 Andersson T, Flockhart DA, Goldstein DB et al.: Drug-metabolizing enzymes: evidence for clinical utility of pharmacogenomic tests. Clin. Pharmacol. Ther. 78, 559–581 (2005). Comprehensive review of CYP450 genotyping in medical practice. Website 101 Ingelman-Sundberg M, Daly AK, Nebert DW: Homepage of the Human Cytochrome P450 (CYP) Allele Nomenclature Committee (2008) www.cypalleles.ki.se 587