* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Review Handout
Immune system wikipedia , lookup
Atherosclerosis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adaptive immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
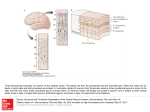
Dr. Janet D. Smith MICROSCOPIC ANATOMY MICROSCOPIC ANATOMY SLIDE REVIEW LYMPHOID ORGANS A. THYMUS Is a primary lymphoid organ (i.e., a site of lymphocyte differentiation rather than site of lymphocyte function in immune responses) Has 2 lobes derived from the fusion of right & left thymic primordia Thin connective tissue (CT) capsule Sheets of CT called septa arise from the capsule Septa divide the thymus into lobules Each lobule has a medulla (the pale central region) & cortex (the darker outer region of the lobule) Medulla is continuous throughout the organ Thymus normally contains no lymphoid nodules. Do not confuse the medulla with the germinal center of a secondary nodule. Blood vessels run in the capsule & septa, & then at the corticomedullary boundary Prothymocytes from the bone marrow enter the thymus via these vessels Stroma is composed of thymic epithelial cells (TECs), also called epithelial reticular cells (ERCs) Pale, euchromatic cells Recognizable by EM because they are joined to one another by desmosomes or tight junctions, & because they contain tonofibrils (bundles of tonofilaments) Poorly phagocytic (distinguishes them from macrophages) Functions of TECs: Provide physical support (stroma) throughout cortex and medulla Act as nurse cells that promote thymocyte differentiation (Types II & V) Create a protected environment in the cortex Contribute to blood-thymus barrier (Type I), which is tight in cortex; leakier in medulla Form a layer deep to the capsule (Type I) that shields the cortex from the environment outside the thymus Separates cortex from medulla (Types III & IV) Form Hassall’s corpuscles in medulla (Type VI) - center of corpuscle may become necrotic, keratinized, or calcified - play an indirect role in the production of regulatory T cells (T REG) Thymic cell types include: MICROSCOPIC ANATOMY TECs Thymocytes (= any lymphocyte within the thymus) Macrophages (recognizable by their phagocytic activity) Dendritic cells (DCs), also called interdigitating dendritic cells (IDCs) - a type of bone marrow-derived antigen-presenting cell (APC) - difficult to distinguish from TECs by light microscopy - by EM, DCs lack tonofilaments - found in the medulla; the other cell types are in both cortex & medulla - play a role in negative selection Thymus receives committed T cell precursors (prothymocytes) from bone marrow throughout life Prothymocytes enter thymus from blood vessels at cortico-medullary boundary, migrate to outer cortex of a lobule, & then migrate toward medulla Undergo positive selection in cortex (thymocytes that bind with sufficient strength to TECs will survive) Undergo negative selection mainly in medulla (thymocytes that bind with sufficient strength to DCs, TECs, or macrophages will die) > 95% of thymocytes fail these selection processes and die (by apoptosis) without ever leaving the thymus Naïve CD4+ cells and CD8+ cells that survive leave the thymic medulla via blood vessels or lymphatics Thymus begins to involute around puberty, but some functional tissue remains, & thymocyte maturation continues throughout life Involution affects cortex before medulla: - cortex becomes a discontinuous layer - white fat accumulates in the areas previously occupied by cortex B. LYMPH NODES: Are secondary lymphoid organs Filter antigens from afferent lymph & initiate immune responses to them Have a capsule & trabeculae (finger-like projections) of dense irregular CT Have a cortex (including the paracortex), and a medulla Cortex Lies immediately deep to subcapsular sinus Dark staining due to numerous lymphocytes & few trabecular sinuses Outer cortex includes lymphoid nodules (follicles) & internodular cortex - nodules are B cell territory (thymus-independent) - internodular cortex is T cell territory (thymus-dependent) Paracortex lies deep to the outer cortex MICROSCOPIC ANATOMY - lacks lymphoid nodules dark staining due to densely packed lymphocytes is predominantly T cell territory contains high endothelium venules (HEVs) rich in interdigitating dendritic cells (IDCs), which act as APCs to activate T cells - is the site where immune responses are most often initiated in a node Medulla The central region of the node Has 2 components: - medullary sinuses: numerous pale-staining lymph sinuses - medullary cords: dark-staining regions of closely packed cells that surround the medullary sinuses - cords have a mixed cell population including T & B lymphocytes, plasma cells & macrophages Can be distinguished from the light-staining medulla of the thymus because thymic medulla is uniformly pale; medulla of lymph node contains pale medullary sinuses plus dark-staining medullary cords HEVs Are postcapillary venules Characterized by cuboidal to columnar endothelial cells Most lymphocytes enter a node by crossing the wall of an HEV Other leukocyte types do not usually cross the HEV wall Stroma of a node consists of reticular CT cells and reticular fibers Attached to capsule and trabeculae Present throughout cortex & medulla, including within the lumen of lymphatic sinuses (subcapsular, trabecular, & medullary sinuses) PATHWAY OF LYMPH FLOW Afferent lymphaticsà subcapsular sinusà trabecular (= intermediate or cortical) sinusesà medullary sinusesà efferent lymphatics Afferent lymphatics Carry lymph to the node Nodes are the only organs with afferent lymphatics They pierce capsule anywhere except at the hilum Have no stroma within their lumen A valve is often present where an afferent enters the capsule Antigens (ags) most often enter a node via afferent lymphatics Subcapsular, trabecular, & medullary sinuses MICROSCOPIC ANATOMY Are all located interior to the capsule (i.e., within the node) Have stroma across their lumen, with macrophages adhering to it - are important sites of antigen trapping, especially subcapsular sinus Endothelial lining is discontinuous in many places (highly permeable) No valves Efferent lymphatics Leave from hilum Have no stroma within their lumen Have numerous valves Lymphocytes most often leave a node in efferent lymphatics Lymphatic vessels (afferent & efferent) have a continuous endothelium A lymphatic that is efferent to one node is often afferent to another node LYMPHOID NODULES (= LYMPHOID FOLLICLES) Are the areas to which B cells preferentially migrate after entering a node Contain: B lymphocytes (& small number of T cells) Follicular dendritic cells (FDCs) that bind ag-ab complexes via the Fc portion of the antibody, but are not antigen-presenting cells according to the strict definition of that term because they do not process the antigen Macrophages whose functions include phagocytizing apoptotic lymphocytes PRIMARY VS. SECONDARY NODULES Primary nodule: Uniformly dark-staining due to many small (inactive) B lymphocytes Secondary nodule: Develops from a primary nodule during an immune response Consists of: - germinal center: pale area where activated B cells enlarge & divide (blast transformation) - mantle (cap, corona): dark outer region surrounding ~ 3/4 of the germinal center (contains small B cells including memory B cells) Presence of secondary nodules indicates that an antibody-producing immune response is in progress Well-developed germinal centers have a dark zone & a light zone Dark zone (usually closest to paracortex) - contains the most recently activated B cells - these B cells are rapidly dividing and are called centroblasts MICROSCOPIC ANATOMY - they undergo somatic hypermutation, which helps generate antibody diversity Light zone - centroblasts move from dark zone into light zone - in the light zone they divide less actively & are called centrocytes - centrocytes undergo processes including: - affinity maturation, which results in individual B cells producing antibodies with increasing affinity for the antigen during the course of an immune reaction. - involves somatic hypermutation to generate ab diversity, followed by a selection process that involves interaction with ag-ab complexes on FDCs - class switching of antibody , e.g., IgM to IgG - high rates of apoptosis Some of the surviving centrocytes become plasmablasts Begin producing abs, but are not morphologically recognizable as plasma cells Migrate to medullary cords and develop into identifiable plasma cells Some plasma cells leave the node via efferent lymphatics Some centrocytes become memory B cells C. SPLEEN Is a secondary lymphoid organ that filters the blood to remove: Antigens and initiate immune responses to them Old or damaged red blood cells Has lymphoid regions collectively called the white pulp Has non-lymphoid regions called the red pulp that surround the white pulp White pulp and red pulp are so-named because of their appearance in a fresh unfixed specimen In H&E-stained sections, white pulp is darkly basophilic due the heterochromatic nuclei of its many lymphocytes; red pulp is eosinophilic due to large numbers of erythrocytes Spleen also has: A hilum where blood vessels enter and leave, and where efferent lymphatics leave A capsule & trabeculae composed of dense irregular CT No subcapsular or trabecular sinuses Trabeculae contain blood vessels (trabecular arteries & veins) A mesothelium that covers the outer surface of the capsule since the spleen is intraperitoneal MICROSCOPIC ANATOMY A stroma composed of reticular cells and reticular fibers Most abundant in the splenic cords of the red pulp and the basement membrane of splenic sinusoids (but absent from the lumen of the sinusoids) Less abundant in germinal centers of the white pulp NOTE: Spleen has no cortex or medulla WHITE PULP: Consists of discontinuous masses of tissue surrounded by red pulp Each area of white pulp is organized around a central artery White pulp has 2 components: Periarteriolar lymphatic sheath (PALS) (a cylindrical collar of T lymphocytes surrounding the central artery) Lymphoid nodules (primary or secondary) embedded in the PALS - where nodules are present, they often push the central artery aside, i.e., toward the edge of the white pulp There is often no obvious boundary between a nodule and the PALS MARGINAL ZONE: Is the area where immune responses are often initiated in the spleen because it is a region into which antigens, T cells, & B cells are delivered by side branches of a central artery Sometimes identifiable in H&E as several layers of flat reticular cells oriented circumferentially around white pulp Can be visualized by specialized techniques (immunocytochemistry, immunofluorescence) to reveal: Reticular fibers encircling the white pulp Cell types that are specific to the marginal zone (e.g. marginal zone B cells, several types of macrophages) Marginal zone B cells differ from other B cells in that: They don’t recirculate Many are specific for bacterial or viral antigens, and can be activated without T cell help They shuttle antigens from marginal zone to nodules of white pulp RED PULP: Looks red due to many RBCs, fewer lymphocytes MICROSCOPIC ANATOMY 2 components: Splenic (or venous) sinuses (sinusoids) characterized by: - cigar-shaped endothelial cells oriented longitudinally in the vessel - discontinuous basement membrane (organized into interconnected hoops that encircle the vessel) Splenic cords (Bilroth’s cords) - cords are the areas that surround the sinuses - contain stroma, macrophages and all blood cell types Blood from open circulation is dumped into splenic cords Macrophages in the cords trap particles and antigens; act as ACPs Red and white cells in the cords must cross the wall of a splenic sinus to reenter circulation NOTE: Splenic sinuses are blood vessels, not lymph sinuses BLOOD FLOW THROUGH THE SPLEEN: Human spleen has a vasculature that is probably entirely an open circulation In an open circulation the blood is not contained within a vessel at all times Pathway of splenic blood flow in open circulation: Splenic artery Capsular arteries Trabecular arteries Central arteries (leave trabeculae & are surrounded by white pulp) - have side branches, some of which open into the marginal zone Penicillar arterioles Sheathed capillaries - open into splenic cords, i.e., blood leaves the vascular system - sheath is composed of macrophages Splenic cords (where ags are trapped & old or defective RBCs are destroyed) Splenic sinuses Pulp veins (squamous endothelium & continuous basement membrane) Trabecular veins Capsular veins Splenic vein Hepatic portal vein NOTE: In a closed circulation, all the capillaries would be directly continuous with the splenic sinuses D. KEY FEATURES OF LYMPHOID ORGANS MICROSCOPIC ANATOMY FEATURE LYMPH NODE SPLEEN THYMUS Capsule Yes Yes Yes (thin) Mesothelium No Yes No Cortex & medulla Yes No Yes Cords & sinuses Yes (medullary) Yes (splenic) No Lymphoid nodules Yes Yes No Special features Lymph sinuses Red/white pulp Blood sinuses Hassall's corpuscles