* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download BIOTRANSFORMATION PHASE I Phase II
NADH:ubiquinone oxidoreductase (H+-translocating) wikipedia , lookup
Citric acid cycle wikipedia , lookup
Proteolysis wikipedia , lookup
Enzyme inhibitor wikipedia , lookup
Nicotinamide adenine dinucleotide wikipedia , lookup
Human digestive system wikipedia , lookup
Biosynthesis wikipedia , lookup
Amino acid synthesis wikipedia , lookup
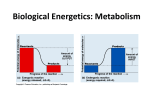
Oxidative phosphorylation wikipedia , lookup
Metalloprotein wikipedia , lookup
Specialized pro-resolving mediators wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
BIOTRANSFORMATION •Enzymatic processes in liver and other tissues that modify the chemical structure of xenobiotics, render them more water-soluble, increase their elimination, decrease their half-life •Biotransformed Biotransformed metabolites are chemically different from the parent molecule Xenobiotic PHASE I Expose or Add functional groups Oxidation Reduction H d l i Hydrolysis Lipophilic Primary products PHASE II Biosynthetic conjugation Secondary products Excretion Hydrophilic (Ionizable) e.g. barbital (water soluble) vs hexobarbital (highly liposoluble) t1/2= 55h (theoretical, real) vs t1/2 of months, real t1/2= 5hr PHASE I Add or expose functional groups: -OH, -SH, -NH2, -COOH, COOH … (small increase in hydrophilicity) Phase II Conjugation with endogenous molecules: glucuronic acid, sulfate, glutathione, ... covalent bonds formed (large increase in hydrophilicity) Table 6.1 C&D 1 Major organ of biotransformation LIVER (hepatocytes) Secondary organs of biotransformation kidney lungs testes skin intestines Preparation of Phase I enzymes (e.g. liver) endoplasmic reticulum (microsomes) and cytosol Liver homogenate Centrifuge at 9 000g (separation of mitochondria mitochondria, lysosomes, lysosomes nuclei, nuclei broken cells) Supernatant at 105 000g Precipitate (Phase I) Supernatant (Phase II) Biotransformation PHASE I Hydrolysis (chemical reaction of a compound with water, usually resulting in the formation of one or more new compounds) • Carboxylesterases, cholinesterases, organophosphotases • Peptidases • Epoxide Hydrolase (EH) -detoxifying detoxifying enzyme for epoxides -formation of diols -EH present in many tissues -epoxides: electrophilic, tend to bind to proteins, to nucleic acids Fig. 6.4 C&D, Hydrolyation of epoxides by EH 2 Role of EH in the biotransformation of benzo[a]pyrene B[a]P •Inactivation of benzo[a]pyrene 4,5-oxide •Conversion of B[a]P to tumorigenic diolepoxide Fig. 6.6 C&D REDUCTION e.g Azo- and Nitro-Reductions Azo-reduction N=N Prontosil [4H] -NH2 1,2,4-triaminobenzene -NH2 Sulfanilamide Fig. 6.8 C&D Azo- and Nitro-reductions can be catalyzed •by enzymes of intestinal flora • by cytochrome P450 (usually oxidizing enzyme), has the capacity to reduce xenobiotics under low oxygen or anaerobic conditions (substrate rather than oxygen, accept electrons and is reduced) •interactions with reducing agents (reduced forms of glutathione, NADP,…) 3 REDUCTION – Role of intestinal microbial flora in biotransformation • •Oxidation by cytochrome P450 •Conjugation with glucuronic acid by UDP-GT UDP GT •Excretion of glucuronide in bile •Reduction by microbial flora under anaerobic conditions •Reabsorption from intestine •Hydroxylation of amine group •Conjugation with sulfate or acetate •Reactive metabolites •Tumorigenic Fig. 6.9 C&D OXIDATION •Monoamine oxidase (MAO), Multiple function oxidase (MFO) •Flavin Monooxygenases (nicotine, cocaine,…) •Alcohol dehydrogenase (liver ADH, gastric ADH) oxidation of alcohols to aldehydes low ADH links to high blood alcohol levels lower gastric ADH in women/men ADH activity lower after fasting clinical alcoholics have lower gastric ADH racial differences in gastric ADH •Aldehyde dehydrogenase (ALDH) oxidation of aldehydes to carboxylic acid ADH R-CH2OH NAD+ ALDH R-C=O H NADH + H+ NAD+ + H2O R-C=O OH NADH + H+ Fig. 6.19 C&D 4 Biotransformation of alcohol Fig. 6.20C&D CYTOCHROME P450 • • Table 6.6 C&D • most versatile oxidative enzyme heme-containing protein ferric Fe3+ reduced to ferrous Fe2+ reduced cytP450 can bind oxygen 6.35 C&D 5 Nomenclature of cytochrome P450 – use of recombinant DNA CYP Amino acid sequence known for many cytP450s <40% a.a. homology, assigned to different genes (CYP1 CYP2 (CYP1, CYP2, CYP3 CYP3,..)) 40-55% a.a. homology, different subfamily (CYP2A, CYP2B, CYP2C,…) >55% a.a. homology, different members of same subfamily (CYP2A1, CYP2A2,…) Use of Knockout Mice Inhibition of cytochrome P450 (aminobenzotriazole – inhibits synthesis of cytP450) detergents, CO, … Fig. 6.35 C&D 6 Cytochrome P450 -can oxidize a substrate (e.g. a xenobiotic) -can transport electrons -many isoforms of cytP450 isolated (in human, rat, others) -importance of NADPH-cytochrome P450 reductase (embedded in ER membrane with cytP450) -catalytic catalytic cycle -inducible by specific substrates (e.g. phenobarbital, benzo[a]pyrene, methylcholanthrene) Simplified reaction: Substrate (RH) + O2 + NADPH + H+ Product (ROH) + H2O + NADP+ How can we demonstrate a role for cytP450 in biotransformation of a XB? -cytP450 activity increases -enzymatic inhibitors of cytP450 (e.g. aminobenzotriazole) -absorption spectrum of cytP450 -reaction can be reconstituted Hydroxylation of substrates by cytochrome P450 Fig. 6.36 C&D Deactivation (detoxication) 7 Role of cytochrome P450 and peroxidase in activation of benzene in bone marrow Fig. 6.29 C&D PHS – prostaglandin H synthase Halothane hepatitis and activation by oxidation and reduction Fig. 6.16 C&D 8 Reactions catalyzed by cytochrome P450 Fig. 6.43 C&D Experimental studies with biotransformation enzymes 1. Induction of enzymes exposure to inducing agents phenobarbital, PAH stimulation of protein synthesis “de novo” Characteristics Time of max effect Persistence of induction Protein synthesis Biliairy flow Cytochrome P450 Cytochrome P448 NADPH-cytochrome-c Reductase PAH hydroxylation Reductive dehalogenation Epoxide hydrolase …. phenobarbital 3-5 days 5-7 days large increase increase increase no effect PAH 1-2 days 5-12 days small increase no effect no effect increase increase small increase increase increase no effect increase no effect small increase 2. Inhibition of biotransformation enzymes e.g. inhibition cytP450 (see graph) 9 BIOTRANSFORMATION •Enzymatic processes in liver and other tissues that modify the chemical structure of xenobiotics, render them more water-soluble, increase their elimination, decrease their half-life •Biotransformed Biotransformed metabolites are chemically different from the parent molecule Xenobiotic PHASE I Expose or Add functional groups Oxidation Reduction H d l i Hydrolysis Lipophilic Primary products PHASE II Biosynthetic conjugation Secondary products Excretion Hydrophilic (Ionizable) Structure of cofactors for Phase II biotransformation PHASE II REACTIONS •biosynthesis of polar, hydrophilic metabolites eliminated in urine (small M.W.,250) or bile (M.W.>350) •requires cofactors and endogenous substrates •ATP dependent Fig. 6.45 C&D 10 Substrates that are glucuronidated 1. Glucuronidation major Phase II pathway in all mammals, except cats • • conjugation j g with g glucuronic acid mediated by UDP-GT Liver>>>>kidney, lung, brain localized in ER (other Phase II enzymes in cytosol) • • detoxication or bioactivation large increase in hydrophilicity Fig. 6.47 C&D Bioactivation of xenobiotics by Phase II reactions (glucuronidation) Fig. 6.49 C&D 11 bile Fig. 6.9 C&D 2. SULFATION Bioactivation by sulfation •cofactor: PAPS (3’-phosphoadenosine-5Phosphosulfate) •enzyme enzyme Sulfotransferase •detoxication or bioactivation 3. Methylation •cofactor: SAM (s-adenosyl methionine) •enzyme methyl transferase (minor, ~hydrophilicity) 4. Acetylation Fig. 6.50 C&D 12 Toxicity/Damage – alteration of the regulatory or maintenance function of the cell in target tissue Fig. 3.10 5. GLUTATHIONE CONJUGATION •cofactor: GSH (tripeptide glycine, glutamic acid, cysteine) •enzyme: glutathione-S-transferase (GST) localized in cytoplasm>>>ER liver>kidney, testes, intestine, adrenal GST GSH + Substrate (XB) polar metabolites •substrates for GST must have affinity for GSH be hydrophobic contain electrophilic carbon •glutathione conjugates are excreted in the bile (intact) excreted as mercapturic acid in urine 13 Biotransformation of acetaminophen – the good, the bad and the ugly Fig.6.28 C&D Biotransformation of acetaminophen Phase I Phase II: At low dose of Acetaminophen: 90% of dose excreted as sulfates (sulfotransferase has strong affinity, low capacity) no toxic intermediates, no toxicity At high dose, Phase II enzymes capacity is surpassed 43% of dose excreted as sulfates glucuronides, glutahione cojugates (low affinity, strong capacity) accumulation l i off toxic i iintermediates, di toxicity i i •Protective effect of GSH supplementation, e.g. NAC •Fasting for 1 day decreases liver GSH levels by 50% in rats (increase in toxicity of acetaminophen) – effect of nutritional status •Liver pathologies will also influence its biotransformation capacity, as will age, sex, species differences 14 Biotransformation and difficulties of predicting effects of mixtures Fig. 6.14 15 Toxicokinetics : study of modeling and mathematical description of the time course of xenobiotics in the whole organism •Dilution and distribution of agent A •Routes of excretion •Theoretical graphs of blood concentrations of A against time (at time A, B and C) Compare a mammal to fish to amphibian Stocking DDT, PCB in adipose tissue Stocking Pb, St in bone Ecobichon, p.13 C = f(t) C = dependent variable t = independent variable dC dt if > 0 → accumulation if < 0 → elimination Ecobichon 16 Classical approach to toxicokinetics: administer XB in a bolus mode (e.g. iv) take blood samples measure XB in blood •equilibrium reached rapidly between blood and tissues •body behaves as a homogenous unit C = Co x e –kel x t •more complex pattern of distribution •two (or more) compartments involved C = A x e –α x t + B x e –ß x t where A and B are proportionality constants of the change in C α= constant of distribution ß= constant of elimination Fig.7.1 One compartment model log of plasma concentrations vs time Fig.7.2 C = Co x e –kel x t straight line (monoexponential model) Log C = - (kel/2.303) /2 303) x t + log Co (logarithmic equation) Kel = elimination constant (elimination includes biotransformation, excretion and exhalation) C=plasma concentration Co=concentration at t= 0 (y intercept ) How does the dose or the remaining concentration in the plasma influence elimination? 17