* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Elaborate interactions between the immune and nervous systems
Monoclonal antibody wikipedia , lookup
Major histocompatibility complex wikipedia , lookup
Social immunity wikipedia , lookup
Myasthenia gravis wikipedia , lookup
DNA vaccination wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Immune system wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Innate immune system wikipedia , lookup
Autoimmunity wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
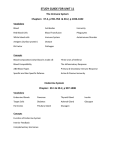
© 2004 Nature Publishing Group http://www.nature.com/natureimmunology REVIEW Elaborate interactions between the immune and nervous systems Lawrence Steinman The immune system and the nervous system maintain extensive communication, including ‘hardwiring’ of sympathetic and parasympathetic nerves to lymphoid organs. Neurotransmitters such as acetylcholine, norepinephrine, vasoactive intestinal peptide, substance P and histamine modulate immune activity. Neuroendocrine hormones such as corticotropin-releasing factor, leptin and α-melanocyte stimulating hormone regulate cytokine balance. The immune system modulates brain activity, including body temperature, sleep and feeding behavior. Molecules such as the major histocompatibility complex not only direct T cells to immunogenic molecules held in its cleft but also modulate development of neuronal connections. Neurobiologists and immunologists are exploring common ideas like the synapse to understand properties such as memory that are shared in these two systems. The nervous system and the immune system mount a variety of essential, coordinated responses to danger. These two systems communicate through intricate chemical messengers that are able to breach their independent and often sequestered anatomical locations. The central nervous system (CNS) is without ‘classical’ lymphatic drainage, meaning that in some ways it is devoid of the immune surveillance that is available for the rest of the body. In health there are mechanisms to exclude potentially destructive lymphoid cells from the brain, spinal cord and peripheral nerves1. However, multiple anatomic and physiological connections exist between the CNS and the immune system, including ‘hardwiring’ of the autonomic nervous system via the vagal nerve and sympathetic nerve fibers to the main sites of the immune system in the liver, spleen, bone marrow, thymus, lymph nodes, skin and gastrointestinal system2,3. Multiple chemical messengers, ranging from small molecules such as nitric oxide to neuroendocrine peptides such as corticotropin-releasing factor (CRF) to large proteins including cytokines and growth factors and their respective receptors, also tie these systems together. Thus, these two elaborate systems for both sensing danger and mounting a counterattack to these threats are inextricably linked. Much is known about the interactions of the brain and immune system, and a substantial framework exists for future exploration. There are three types of interactions between the CNS and the immune system: in the first, the CNS acts reciprocally with the immune system; in the second, the CNS drives immunity; and in the third, the immune system regulates the CNS. Perhaps the quintessential reciprocal interaction is the brain’s orchestration of the febrile response in reaction to the immune system’s mobilization against infection and Department of Neurological Sciences and Neurology and Pediatrics, Interdepartmental Program in Immunology, Beckman Center for Molecular Medicine, Stanford, California 94305, USA. Correspondence should be addressed to L.S. ([email protected]). Published online 26 May 2004; doi:10.1038/ni1078 NATURE IMMUNOLOGY VOLUME 5 NUMBER 6 JUNE 2004 inflammation. Infection is one of the primary stimuli for modulation of the brain by the immune system. The brain modulates the immune system in response to environmental stress through the hypothalamic pituitary axis, orchestrating immune responses with CRF4. Fever and the orchestration of neural and immune physiology The immune system signals the brain to respond to the ‘danger’ of viruses, bacteria and parasites through an elaborate system. The intricacies of brain-immune interaction require highly localized windows in the blood-brain barrier. These windows, known as the circumventricular organs, allow transmission of soluble mediators released by immune cells to precise sites located in the hypothalamus of the brain5. Probably nowhere in biology is there a better demonstration of the complex choreography of physiological response to ‘danger’ than is seen in the interactions of brain and immune system, resulting in fever and its subsidiary effects on behavior, including sleep, feeding and appetite. The first cytokine discovered in the immune system, interleukin 1 (IL-1), alerts the hypothalamus that there is ‘danger’ in the periphery. Other pyrogenic signals include tumor necrosis factor (TNF) and IL-6. These cytokines activate the febrile response through neurons in the preoptic area of the anterior hypothalamus5, although the actual mechanism whereby these hydrophilic peptides breach the blood-brain barrier remains controversial. Considerable evidence suggests that they pass through windows in the organum vasculosum laminae terminalis on the midline of the preoptic area in the hypothalamus. Evidence also exists for active transport of these cytokines through specific carriers that allow these key molecules to cross the blood-brain barrier5. Other theories for activation of the preoptic neurons’ mediating fever, which are not mutually exclusive with the other mechanisms, include the idea that pyrogenic cytokines such as IL-1, IL-6 and TNF may induce generation of prostaglandin E2 in cells at the blood-brain interface. Prostaglandin E2 is synthesized through a cyclooxygenase-2-dependent pathway in cerebral endothelial cells or microglia5,6. Prostaglandin E2 crosses the blood-brain barrier and 575 © 2004 Nature Publishing Group http://www.nature.com/natureimmunology REVIEW stimulates the temperature increase induced through the activity of preoptic neurons7. There is also evidence that afferent fibers in the vagal nerve may transport pyrogenic cytokines to the thermoregulatory centers in the hypothalamus8 (Fig. 1). Immunologists divide the physiological functions of cytokines into convenient subsets, such as the T helper type 1 (TH1)/TH2 dichotomy. TH1 cytokines, including interferon-γ (IFN-γ) and TNF, are associated with activation of many autoimmune diseases, including multiple sclerosis, rheumatoid arthritis and juvenile diabetes. TH2 cytokines, characterized by IL-4, IL-5 and IL-13, are associated with suppression of such diseases and the promotion of allergic responses, including asthma and food sensitivities9–12. The balance between TH1 and TH2 cytokines is also important in the control of fever. Cholesterol metabolism is important in the maintenance of TH1/TH2 balance10,12,13. The metabolic pathways leading from mevalonate to cholesterol lead to the formation of isoprenoids. These lipids, including farnesyl derivatives, are attached to molecules that are essential in the regulation of inflammation and the balance between TH1 and TH2 cytokines. Ultimately, the inhibition of the farnesylation of Ras leads to increased phosphorylation of STAT6, the key transcription factor for TH2 cytokines13. A deficiency in a key enzyme in cholesterol metabolism, mevalonate kinase, leads to a clinical syndrome characterized by hypergammaglobulinemia and periodic fever. In that syndrome there is increased secretion of IL-1 from peripheral blood lymphocytes14. Just as proinflammatory cytokines such as TNF and IL-1 can induce fever, the TH2 cytokines are required for defervescence15. Fever itself lowers production of IL-1 by influencing the proteolytic processing of IL-1, and this favors the production of TH2 cytokines such as IL-5 and IL-13 (ref. 16). Hardwiring of the CNS and lymphoid organs The brain and the immune system communicate through neurotransmitters, cytokines and endocrine hormones. The brain and the immune system are actually hardwired through the autonomic nervous system: the parasympathetic nervous pathways innervate lymphoid tissues via the neurotransmitter acetylcholine, and the sympathetic nervous pathways innervate lymphoid tissue via the neurotransmitter norepinephrine (Fig. 2). There is direct evidence of these rich neural connections with lymphoid tissue, including thymus and bone marrow as well as lymph nodes, spleen and gut-associated lymphoid tissue2,3. Receptors for various neurotransmitters beyond the parasympathetic mediator acetylcholine17,18 and the sympathetic mediator norepinephrine19–21 are also present on Thymus lymphocytes. These neurotransmitters include vasoactive intestinal peptide (VIP), pituitary Lymph nodes adenylate cyclase–activating polypeptide22–24, calcitonin gene–related peptide (CGRP), substance P25,26, histamine and serotonin27,28. Likewise, receptors for neuroendocrine mediators, including CRF4,29, α-melanocyteAfferent & efferent vagus stimulating hormone (α-MSH)4,30–32 and lepnerve activity Spleen tin4,33–37, are found on lymphoid tissue. These Bone marrow hardwired circuits are essential in regulating Sympathetic nerves the inflammatory response. The parasympathetic neurotransmitter acetylcholine potently modulates several classical immune reactions via the vagus nerve. Leptin In an animal model of arthritis, paw swelling PAC1 PACAP Leptin MC4 after injection of the inflammatory chemical receptor receptor carageenen could be suppressed by vagal nerve α−MSH Fat stimulation17. Vagal nerve stimulation can also Epinephrine suppress the systemic shock–like response after Sympathetic H1R injection of endotoxin17,18. Activation of the Adrenergic neuron Histamine receptor nicotinic acetylcholine receptor (AchR), AChR expressed in macrophages, inhibits secretion of H2R IL-1 and TNF18. Thus, a common neurotransmitter, acetylcholine, can modulate lethal ACh CGRP Cholinergic CRF immune reactions such as septic shock. neuron PAR2 The sympathetic nervous system can receptor VPAC1 VPAC2 alter the TH1/TH2 balance through stimulaSubstance P tion of the β-adrenergic receptor. IL-10 VIP Pain fiber release is provoked after brain injury19. IL-10 suppresses inflammatory responses. The macrophage-mediated release of IL-10 Figure 1 Neural pathways involved in immune regulation. Extensive parasympathetic and sympathetic can be blocked with propranolol, a classical inputs modulate immune activity through the AchR and adrenergic receptors. Pain fibers modulate β-adrenergic antagonist19. Sympathetic nerve immunity through substance P and CGRP, with these effects mediated by proteinase-activated receptor 2 (PAR2) receptors. VIP and pituitary adenylate cyclase–activating polypeptide (PACAP) and stimulation enhances production of TH2 histamine receptors regulate the balance of TH1/TH2 cytokine production. Histamine type 1 receptor cytokines while inhibiting TH1 cytokine pro(H1R) is found on TH1 T cells, and antagonism of H1R blocks TH1 immunity. H2R is found on TH2 T duction. Thus, exposure of TH1 cells to terbucells, and TH2 agonism upregulates TH2 immunity. Neuroendocrine mediators such as leptin, α-MSH taline before their activation inhibits IFN-γ and CRF also modulate immune activity. CRF is released from the hypothalamic pituitary axis. Leptin production by these cells. The β-adrenergic is released from the hypothalamus in response to increases in body fat. Increased CRF inhibits TH1 antagonists block this effect20. In the immunity, whereas increased leptin enhances TH1 immunity. 576 VOLUME 5 NUMBER 6 JUNE 2004 NATURE IMMUNOLOGY © 2004 Nature Publishing Group http://www.nature.com/natureimmunology REVIEW synovium of patients with rheumatoid arthritis, norepinephrine is a strong suppressor of inflammatory cytokines such as TNF and IL-6 (ref. 20). Unfortunately, in rheumatoid arthritis there is evidence of loss of sympathetic innervation in the joints, and this may contribute to the pathological effects of TNF on the synovium21. The sympathetic nervous system is involved in the transmission of prions from peripheral sites such as the gastrointestinal system to the brain. The follicular dendritic cell, an immune cell essential for the presentation of foreign antigens through the major histocompatibility complex (MHC), is key in the transmission of prions from the periphery to the central nervous system through an interaction between splenic monocytic cells and sympathetic neurons. This nerve-immune contact is essential in the pathology of the spongiform encephalopathies, transmitted through the blood or the gastrointestinal tract. These acquired prion diseases include bovine spongiform encephalopathy (‘mad cow disease’)38,39. The neurotransmitter VIP and pituitary adenylate cyclase– activating polypeptide are also produced in lymphoid cells, where they are potent suppressors of inflammatory cytokines and chemokines. VIP blocks delayed-type hypersensitivity reactions22 through inhibition of various chemokines23. VIP has two G protein–coupled receptors, VPAC1 and VPAC2. VPAC2-null mice have decreased immediate-type hypersensitivity and enhanced delayed-type hypersensitivity22. Pituitary adenylate cyclase–activating polypeptide and its receptor PAC1 are important in inflammation. PAC1 is involved in the production of IL-6, an important mediator of septic shock24. The intimate relationship between neural pathways that mediate pain, and the immune regulation of inflammation are extensive. Sensory nerves, especially those mediating pain reflexes, are afferent nerves connecting the peripheral organs such as skin to the spinal cord. These nerves conveying the sensation of pain, are stimulated by tryptase produced in mast cells. Mast cells are mobile lymphoid cells that act as sentinels of immune brain interactions. They pack secretory granules filled with neurotransmitters, such as histamine, and enzymes, such as tryptase, which can directly activate sensory neural fibers. Activation of these nerves as part of the pain reflex stimulates the release of both CGRP and substance P from C-type sensory nerve fibers in both peripheral tissues and spinal cord. Neural release of CGRP and substance P also causes edema and widespread inflammation in skin25,26. Tryptase triggers this nerve-mediated inflammatory response, involving CGRP and substance P, through proteinaseactivated receptor 2 in dorsal root ganglion neurons. These dorsal root ganglia just outside the spinal cord contain the cell bodies for the sensory neurons in skin25,26. Tryptase can also activate blood mononuclear cells to release TNF, IL6, and IL-1 (ref. 40). Tryptase is increased in the autoimmune disease of the brain multiple sclerosis and in rheumatoid arthritis41–44. Tryptasetriggered pain pathways may thus mediate the immune pathogenesis of these organ-specific autoimmune diseases. Mast cells, chief producers of tryptase, not only act within the CNS but also are involved in demyelinating disease as well as in models of arthritis27,41–43,45–47. The function of the neurotransmitter histamine, also produced by mast cells, is important in autoimmunity. Histamine acts on blood vessels to cause dilatation and on bronchi to cause constriction. Histamines can modulate TH1 and TH2 cytokine production. Histamine receptors are found on lymphocytes, with an excess of histamine type 1 receptors on TH1 T cells and a preponderance of histamine type 2 receptors on TH2 cells27,28. Blockade of histamine 1 receptors can block classical TH1-mediated organ-specific autoimmune diseases such as experimental autoimmune encephalomyelitis (EAE)27,28,42. Modulation of mast cell activity or deletion of mast cells NATURE IMMUNOLOGY VOLUME 5 NUMBER 6 JUNE 2004 attenuates EAE45. Histamine 1 receptors are found in abundance in brain lesions of multiple sclerosis41. Modulation of immunity with behavioral stimuli Stimuli such as overeating, sleep and stress, and even operant conditioning in which a positive or negative stimulus is paired with a particular behavioral outcome, can influence the immune response. The well known feeling of sleepiness and the lack of appetite associated with fever is in part a result of proinflammatory mediators acting on the hypothalamus4. IL-6 can induce sleep, and TNF, also known as cachectin, can induce anorexia4,48. Leptin, a molecule produced in response to levels of fat stores and that thereby regulates body weight, is a potent stimulator of TH1 immunity4,33,34,37. The structure of leptin resembles that of other cytokines including IL-6, IL-11, IL-12, leukemia inhibitory factor, granulocyte colony-stimulating factor, ciliary neurotrophic factor and oncostatin M. The leptin receptor family is a member of the class I cytokine receptor family, which includes gp-130, a component similar to the signal-transducing module of the IL-6 family of cytokines35. Leptin is produced by neurons at the site of inflammation in multiple sclerosis and its animal model, EAE4,33,34,41. The genetically obese mouse (ob/ob), which has a deficiency in leptin production, mounts a poor TH1 response and is relatively resistant to EAE33,34. Sympathetic denervation blocks the leptin-induced changes in T and B cell function, suggesting that leptin mediates its effects on immune cell function through the sympathetic nervous system and stimulation of the β2-adrenergic receptor36,37. Two other hypothalamic peptides that reduce appetite are CRF and α-MSH. Both of these hormones are important in immunity. CRF is released from the hypothalamus in response to environmental stress and activates the pituitary to produce adrenocorticortropin hormone (ACTH), which in turn activates the adrenals to produce corticosteroids. Increased CRF inhibits TH1 immunity. Infusions of CRF will suppress EAE, even in adrenalectomized mice, indicating that CRF acts directly on lymphoid cells4,29. Similarly, infusion of antalarmin, a CRF receptor antagonist, suppresses experimental arthritis in rats49. α-MSH inhibits activation of transcription factors such as NF-κB and is thus anti-inflammatory30. It has been used to induce tolerance to antigens applied cutaneously and is normally present in the highly immunosuppressive environment of the anterior chamber of the eye31. Given the existence of hardwiring of the nervous system to the immune system through neurotransmitters and neuroendocrine mediators, it has been possible to demonstrate modulation of the immune response with behavioral experiments in which animals are stressed. Placement of animals in restraints induces stress in the animals, activating CRF and adrenocorticoids. Restraint stress augments delayed-type hypersensitivity in the skin, and these effects can be abrogated in IFN-γ knockout mice, demonstrating that the stress response modulated one of the key local mediators of cell-mediated immunity in the skin50. The hardwiring between the nervous system and the immune system can be exploited with experimental psychology. Classic behavioral modification techniques can produce immune suppression. Operant conditioning, in which a behavioral outcome is paired with a positive or negative stimulus, has been used to ‘train’ lupus-prone NZB/W mice to suppress manifestations of autoimmunity. A conditioned stimulus with saccharin was paired with cyclophosphamide, the unconditioned stimulus. The rate of proteinuria and mortality were decreased in conditioned mice compared with that of untreated control and nonconditioned mice51,52. These experiments indicate that behavioral conditioning can strongly modulate the immune response. 577 REVIEW Myelin © 2004 Nature Publishing Group http://www.nature.com/natureimmunology Hypothalamus Narcolepsy? Anorexia? Multiple sclerosis GluR Purkinje cells AChR Rasmussen epilepsy Paraneoplastic ataxia Myasthenia gravis Skeletal muscle Figure 2 The immune system targets various levels of the nervous system. In multiple sclerosis, immune responses are directed to targets in white matter. In Rasmussen encephalitis, epilepsy results from an antibody directed to glutamate receptors (GluR). Paraneoplastic immunity targets Purkinje cells in the cerebellum, resulting in ataxia and incoordination. In myasthenia gravis, antibodies are directed to the AchR in muscle. Diseases such as narcolepsy (in which there is a deficit in orexin) and anorexia may also be due to autoimmunity, although definitive proof is lacking. Autoimmune attacks against the nervous system In some cases the immune system regulates and even destroys normal brain activities (Fig. 2). The immune system can injure various brain systems in autoimmune attacks, culminating in destruction of white matter and the underlying axon in multiple sclerosis10–12 or in blockade of glutamate-mediated synaptic transmission, resulting in epilepsy, as in Rasmussen disease53. In Rasmussen encephalitis, the immune system mounts a response to glutamate receptor, resulting in epilepsy that is often difficult to treat. Various immune therapies have been tried in Rasmussen encephalitis, but the greatest success has come from removal of large areas of brain, sometimes an entire hemisphere53,54. In the paraneoplastic syndromes, the immune system, in attacking an epitope expressed in or on the cancer cell, mounts an autoimmune response to brain tissues, where the same epitope or one immunologically similar to it is also expressed55. The term ‘molecular mimicry’ is sometimes attached to this pathological manifestation of molecular modularity. Cerebellar ataxia occurs, albeit infrequently, when the immune systems attacks ovarian cancer. Temporal lobe epilepsy sometimes occurs after immunity to oat cell carcinoma. Immunity to neuroblastoma can produce the clinical appearance of ‘dancing eyes and dancing feet’55. In stiff-man syndrome, the immune system mounts an autoimmune attack against glutamic acid decarboxylase, the enzyme involved in the synthesis of the main inhibitory transmitter in the central nervous system. Patients with antibodies to glutamic acid decarboxylase develop stiffness and spasms. In many cases of stiff-man syndrome, insulin-dependent diabetes mellitus develops, because glutamic acid decarboxylase is one of the prevalent targets of the autoimmune response to insulin-secreting beta cells in the pancreas56,57. Stiff-man syndrome can occur as a paraneoplastic syndrome58. Breast cancer has 578 been associated with immunity to glutamic acid decarboxylase in some cases of stiff-man syndrome. In the course of mounting antitumor immunity to breast cancer, in the case of stiff-man syndrome, the immune system attacks an antigen located in the central nervous system. Other paraneoplastic syndromes include encephalitis of the limbic system of the brain, with seizures and behavioral abnormalities; cerebellar ataxia, with incoordination; and disorders of neuromuscular transmission, resulting in weakness55,59. In myasthenia gravis, the immune system somehow becomes intolerant to its own nicotinic AchR. Both T cell and B cell responses are directed to the AchR. The antibodies impair neuromuscular transmission and induce a receptor-mediated shedding of the AchR, ultimately causing structural changes in the neuromuscular junction60–63. The thymus, the immune organ in which central tolerance to self is shaped, expresses AchRs. One of the enduring therapies for myasthenia is removal of the thymus gland64. Bulimia and anorexia and perhaps some psychiatric disorders may have at least part of their pathogenesis in autoimmunity, with autoantibodies to α-MSH and ACTH detected65. At present there is no evidence to suggest that psychiatric disorders such as autism or schizophrenia are caused by an autoimmune response to brain. However, myasthenia gravis was recognized as a defect in neuromuscular transmission, yet only in the early 1970s was it discovered that myasthenia gravis was due to antibodies to the AchR60,61. Subsequent immunohistochemical studies with bungarotoxin, isolated from a deadly snake (the Formosan banded krait), unraveled the pathogenesis of myasthenia. The snake toxin irreversibly binds to nicotinic AchRs, and staining of the myasthenic neuromuscular junction with this snake poison showed that the architecture of the synapse between nerve and muscle was badly distorted by the autoantibody-induced modulation of the AchR60–63. Could such a breakthrough revolutionize our thinking about some psychiatric diseases? The immune response has an adaptive component and an innate component. In most of the diseases discussed above, adaptive immunity can be demonstrated to be central to disease pathogenesis: Specific antibody and T cell responses to AchRs are seen in myasthenia gravis; antibody and T cell responses to glutamic acid decarboxylase are evident in stiff-man syndrome; antibody responses to glutamate receptor are apparent in Rasmussen syndrome; and a wide spectrum of T and B cell responses to myelin components are seen in multiple sclerosis66. In the neurodegenerative diseases Alzheimer disease and Parkinson disease, it has been difficult to identify the main target of the adaptive immune response. Instead, aspects of an innate immune response, including the presence of molecules of the MHC, complement components and cytokines such as TNF are present in the CNS67,68. The lack of adaptive immunity in Alzheimer and Parkinson disease thus contrasts with its presence in diseases such as myasthenia, multiple sclerosis, Rasmussen encephalitis and stiff-man syndrome. Not all autoimmune responses in the brain are necessarily destructive. This positive aspect of the immune response has been justifiably called ‘protective autoimmunity’69. Thus, osteopontin may have proinflammatory effects in mediating TH1 responses70, whereas it may have trophic effects on the nervous system71. Immune cells release brainderived neurotrophic factor72, whereas nerve growth factor can modulate inflammatory autoimmune responses, inducing TH2 cytokines73. These growth factors have restorative and even anti-inflammatory properties. Even destructive cytokines such as TNF, the main immunological mediator of damage in the joint in rheumatoid arthritis or in the intestinal mucosa in Crohn disease74, can have beneficial effects on the brain. TNF is a repair and growth factor for the cells that make the VOLUME 5 NUMBER 6 JUNE 2004 NATURE IMMUNOLOGY REVIEW © 2004 Nature Publishing Group http://www.nature.com/natureimmunology myelin sheath75. Anti-TNF therapy, which is successful in rheumatoid arthritis and in Crohn disease, actually worsens multiple sclerosis, perhaps because TNF is a protective factor in the brain, whereas it is a harmful mediator elsewhere. Another example of the dual properties of a molecule is α4 integrin. Neural stem cells ‘home’ to their desired destinations to repair damaged tissues by using the same integrin molecules expressed by lymphocytes that caused the initial damage76–78. Immune and neurological synapses The immunoglobulin supergene family79 includes many molecules with functions in the brain, including the myelin proteins myelin oligodendroglial glycoprotein, myelin-associated glycoprotein and myelin protein P0; many molecules known for their adhesion functions, such as neural cell adhesion molecule and intercellular adhesion molecule; and the glycoprotein molecule Thy-1, found on neurons and T cells. Some of the quintessential molecules of adaptive immunity, including the TCR, another member of the immunoglobulin supergene family, are expressed in both the nervous system and the immune system. T cells recognize a fragment of antigen in a cleft of the MHC molecule, which is yet another member of the immunoglobulin supergene family. The trimolecular complex of TCR and an antigen fragment bound in the MHC is the main recognition element of T cells. Many molecules first understood because of their functions in one of these two systems have been found to be involved in the other system: The MHC, which is the most essential molecule in the regulation of genetic control of the immune response, is important in neural development80. Molecules associated with inflammation and immunity, including the MHC and complement, are found in the CNS in degenerative conditions, such as Alzheimer and Parkinson disease67,68. In normal adult CNS, these molecules have either very low expression (MHC class I molecules) or none at all (MHC class II molecules)81–83. Their induction and expression at the site of neurodegeneration suggests either that inflammation may be central to the pathogenic process of these conditions, or that their presence signifies a response to neural injury and death. The MHC is essential in the development of the visual system80. Mice deficient in the MHC class I molecules or deficient in a receptor for these molecules (CD3ζ) develop abnormal connections in the lateral geniculate body of the thalamus, which serves as a relay station to the visual cortex at the rear of the brain80. The lateral geniculate body receives optic nerve inputs from the retina and relays these inputs to the visual cortex. MHC molecules are somehow essential in the dynamic development of connectivity that occurs during the neonatal period. The exact mechanism that mediates this effect is not understood. MHC molecules are also essential for specialized electrical activities in the brain. MHC knockout mice have alterations in longterm potentiation and long-term depression in hippocampal neurons. Thus, the MHC is involved in both the development of normal neuronal connections and in the physiology of long-term electrical activities in structures such as the hippocampus that are associated with events such as neurological memory. TCR β-chain transcripts are also expressed dynamically during neuronal development84. These TCRs do not undergo rearrangements characteristic of the development of antigen-specific T cell recognition, however. Further functions for the MHC have been demonstrated in studies of MHC class Ib molecules that selectively associate with pheromone receptors in the olfactory cortex of mice85. Similarly, H-2M nonclassical MHC class I molecules are coexpressed in vomeronasal neurons in rodents in association with certain pheromone receptors86. The MHC may be involved not only in immune recognition but also in more subtle sensing, including the selection of a mate. Other molecules known NATURE IMMUNOLOGY VOLUME 5 NUMBER 6 JUNE 2004 as semaphorins, which are key in axon guidance, are also expressed in the immune system, where they interact with modulators of T cell activity such as the family of T cell immunoglobulin domain and mucin domain molecules87,88. The term ‘synapsis’ was first used by cytogeneticists in the late nineteenth century to describe the pairing and close apposition of homologous maternal and paternal chromosomes in meiosis. Sherrington introduced the term to neurobiology in 1897 to describe the complex structures that arise at points where nerves transmit signals to other nerves or to specialized end organs such as muscle at the neuromuscular junction89. The term ‘synapse’ was first used in the field of immunology in 1984 (ref. 90). The original idea of the ‘immune synapse’ involved CD4, the TCR and MHC antigen complexes in close apposition to the CD3 membrane molecules. Secretory proteins such as the cytolytic molecules used by cytotoxic T cells were compared with neurotransmitters, as they were released into the synaptic cleft. In many ways this view from 1984 was prescient of our understanding of the immune synapse today91,92. We now know the immune synapse is dynamic and elaborately organized with a plethora of molecules at the interface between T cells, antigen and the MHC molecules. What was formerly considered ‘trimolecular ‘ recognition is now understood to be considerably more complex. The dynamics of adhesion and the sensing of antigen in the MHC cleft involve the interaction of several adhesion molecules, the TCR, antigen and the MHC. This provides for positional stability of the TCR with the antigenic fragment in the MHC cleft allowing for nuances in signaling for the TCR and is even perhaps involved in the ‘decision’ by T cells to remain tolerant or intolerant to the antigen held in the MHC cleft91. Immunologists and neurobiologists have collaborated to see functional similarities and differences in their respective synapses, and insights gained in one system should illuminate processes taking place in the other system. One of the notable similarities between the immune and the neurological synapse is that both structures are activated in a ‘quantal’ way. There is calcium flux in T cells in response to a single ‘quantum’ of MHC-peptide complex. However, the T cell synapse will not organize into a functional unit until at least ten peptide-MHC complexes are present93. Photoreceptors in the eye are also maximally sensitive, with measurable responses to single photons. However, effective signaling in the retina only occurs after several photons together trigger the outer segments of the receptor93,94. It seems that both the immune system and the nervous system have developed control mechanisms to prevent a single quantum from fully triggering the T cell or neuron93,94. Although thresholds of sensitivity are present down to the level of a single quantum, with the TCR recognizing a single MHC-peptide complex and the photoreceptor sensing a single photon, the cellular machinery will not fully activate until at least about ten quanta are present and contact the receptor. Obviously the immune system and the nervous system are linked functionally and anatomically. From fever to stress, the influence of one system on the other has evolved in an intricate manner to help sense danger. It remains to be seen whether immune memory and neurological memory have anything in common at the molecular level, even though they share some remarkable features in terms of the amount of information that can be stored in each system. Nevertheless, the speeds at which memories are consolidated and recalled in the two systems are very different. It is perhaps more likely that when the immune system and the nervous system are compared, other functions for the same protein will be found when it is used in a different context. Thus the function of MHC in the nervous system and in the immune system may be completely different, just as a molecule such as osteopontin can have different functions in bone, in the 579 REVIEW immune system and in the brain70,71. Thus, these two systems influence each other and interact with each other, and understanding one system may give us insights into the physiology of the other system. ACKNOWLEDGMENTS Supported by the National Institutes of Health and the Phil N. Allen Trust. © 2004 Nature Publishing Group http://www.nature.com/natureimmunology COMPETING INTERESTS STATEMENT The author declares that he has no competing financial interests. Published online at http://www.nature.com/natureimmunology/ 1. Steinman, L. Connections between the immune system and the nervous system. Proc. Natl. Acad. Sci. USA 90, 7912–7914 (1993). 2. Felten, S.Y. et al. Noradrenergic sympathetic innervation of lymphoid organs. Prog. Allergy 43, 14–36 (1988). 3. Livnat, S., Felten, S.Y., Carlson, S.L., Bellinger, D.L. & Felten, D.L. Involvement of peripheral and central catecholamine systems in neuroimmune interactions. J. Neuroimmunol. 10, 5–30 (1985). 4. Steinman, L., Conlon, P., Maki, R. & Foster, A. The intricate interplay among body weight, stress and the immune response to friend or foe. J. Clin. Invest. 111, 183–185 (2003). 5. Blatteis, C.M. The afferent signaling of fever. J. Physiol. 526, 470 (2000). 6. Li, S., Goorha, S., Ballou, L.R. & Blatteis, C.M. Intracerebroventricular interleukin 6, macrophage inflammatory protein 1β and IL-18: pyrogenic and PGE(2)-mediated? Brain Res. 992, 76–84 (2003). 7. Engblom, D. et al. Prostaglandins as inflammatory messengers across the blood brain barrier. J. Mol. Med. 80, 5–15 (2002). 8. Goehler, L.E. et al. Interleukin-1β in immune cells of the abdominal vagus nerve: a link between the immune and nervous systems? J. Neurosci. 19, 2799–2806 (1999). 9. Mosmann, T.R. & Coffman, R.L. TH1 and TH2 cells: different patterns of lymphokine secretion lead to different functional properties. Annu. Rev. Immunol. 7, 145–73 (1989). 10. Wekerle, H. Tackling multiple sclerosis. Nature 420, 39–40 (2002). 11. Steinman, L., Martin, R., Bernard, C.C.A., Conlon, P. & Oksenberg, J.R. Multiple sclerosis: deeper understanding of its pathogenesis reveals new targets for therapy. Annu. Rev. Neurosci. 25, 491–505 (2002). 12. Zamvil, S. & Steinman, L. Diverse targets for intervention during inflammatory and neurodegenerative phases of multiple sclerosis. Neuron 38, 685–688 (2003). 13. Youssef, S. et al. The HMG-CoA reductase inhibitor, atorvastatin, promotes a TH2 bias and reverses paralysis in CNS autoimmune disease. Nature 420, 78–84 (2002). 14. Frankel, J. et al. Lack of isoprenoid products raises ex vivo interleukin 1β secretion in hyperimmunoglobulinemia D and periodic fever syndrome. Arthritis Rheum. 46, 2794–2803 (2002). 15. Cartmell, T., Ball, C., Bristow, A.F., Mitchell, D. & Poole, S. Endogenous interleukin10 is required for the defervescence of fever evoked by local lipopolysaccharideinduced and Staphylococcus aureus-induced inflammation in rats. J. Physiol. 549, 653–664 (2003). 16. Boneberg, E.M. & Hartun, T. Febrile temperatures attenuate IL-1β release by inhibiting proteolytic processing of the proform and influence TH1/TH2 balance by favoring TH2 cytokines. J. Immunol.171, 664–668 (2003). 17. Tracey, K.J. The inflammatory reflex. Nature 420, 853–859 (2002). 18. Borovikova, L.V. et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405, 458–462 (2000). 19. Woiciechowsky, C. et al. Sympathetic activation triggers systemic interleukin-10 release in immunodepression induced by brain injury. Nat. Med. 4, 808–813 (1998). 20. Sanders, V.M. et al. Differential expression of the β2-adrenergic receptor by Th1 and Th2 clones: Implications for cytokine production and B cell help. J. Immunol. 158, 4200–4210 (1997). 21. Miller, L.E., Grifka, J., Scholmerich, J. & Straub, R.H. Norepinephrine from synovial tyrosine hydroxylase positive cells is a strong indicator of synovial inflammation in rheumatoid arthritis. J. Rheumatol. 29, 427–435 (2002). 22. Voice, J.K. et al. Roles of vasoactive intestinal peptide (VIP) in the expression of different immune phenotypes by wild-type mice and T cell-targeted type II VIP receptor transgenic mice. J. Immunol. 170, 308–314 (2003). 23. Grimm, M.C. et al. Vasoactive intestinal peptide acts as a potent suppressor of inflammation in vivo by trans-deactivating chemokine receptors. J. Immunol. 171, 4990–4994 (2003). 24. Martinez, C. et al. Anti-inflammatory role in septic shock of pituitary adenylate cyclase-activating polypeptide receptor. Proc. Natl. Acad. Sci. USA 99, 1053–1058 (2002). 25. Brain, S.D. & Williams, T.J. Substance P regulates the vasoldilator activity of calcitonin gene-related peptide. Nature 335, 73–75 (1988). 26. Steinhoff, M. et al. Agonists of proteinase-activated receptor 2 induce inflammation by a neurogenic mechanism. Nat. Med. 6,151–158 (2000). 27. Pedotti, R. et al. An unexpected version of horror autotoxicus: anaphylactic shock to a self-peptide. Nat. Immunol. 2, 216–222 (2001). 28. Jutel, M. et al. Histamine regulates T-cell and antibody responses by differential expression of H1 and H2 receptors. Nature 413, 420–425 (2001). 29. Poliak, S. et al. Stress and autoimmunity: The neuropeptides corticotropin releasing 580 factor and urocortin suppress encephalomyelitis via effects on both the hypothalamic-pituitary-adrenal axis and the immune system. J. Immunol. 158, 5751–5756 (1997). 30. Grabbe, S. et al. α-Melanocyte-stimulating hormone induces hapten-specific tolerance in mice. J. Immunol. 156, 473–478 (1996). 31. Streilein, J.W., Okamoto, S., Sano, Y. & Taylor, A.W. Neural control of ocular immune privilege. Ann. NY Acad. Sci. 917, 297–306 (2000). 32. Fekete, C. & Liposits, Z. Histamine-immunoreactive neurons of the tuberomammillary nucleus are innervated by α-melanocyte stimulating hormone-containing axons. Brain Res. 969, 70–77 (2003) 33. Matarese, G. et al. Requirement for leptin in induction and progression of experimental autoimmune encephalomyelitis. J. Immunol. 166, 5909–5916 (2001). 34. Sanna, V. et al. Leptin surge precedes autoimmune encephalomyelitis and correlates with disease susceptibility, inflammatory anorexia and the development of pathogenic T cell responses. J. Clin. Invest. 111, 241–250 (2003). 35. Baumann, H. et al. The full-length leptin receptor has signaling capabilities of interleukin 6-type cytokine receptors Proc. Natl. Acad. Sci. USA 93, 8374–8378 (1996). 36. Demas, G.E. Splenic denervation blocks leptin-induced enhancement of humoral immunity in Siberian hamsters (Phodopus sungorus). Neuroendocrinology 76,178–84 (2002). 37. Rayner, D.V. & Trayhurn, P. Regulation of leptin production: sympathetic nervous system interactions. J. Mol. Med. 79, 8–20 (2001). 38. Prinz, M. et al. Positioning of follicular dendritic cells within the spleen controls prion neuroinvasion. Nature 425, 957–62 (2003). 39. Prinz, M. et al. Lymph nodal prion replication and neuroinvasion in mice devoid of follicular dendritic cells. Proc. Natl. Acad. Sci. USA 99, 919–924 (2002). 40. Malamud, V. et al. Tryptase activates peripheral blood mononuclear cells causing the synthesis and release of TNF, IL-6 and IL-1: possible relevance to multiple sclerosis. J. Neuroimmunol. 138, 115–122 (2003). 41. Lock, C. et al. Gene microarray analysis of multiple sclerosis lesions yields new targets validated in autoimmune encephalomyelitis. Nat. Med. 8, 500–508 (2002). 42. Pedotti, R. et al. Multiple elements of the allergic arm of the immune response modulate autoimmune demyelination. Proc. Natl. Acad. Sci. USA 100, 1867–1872 (2003). 43. Pedotti, R., DeVoss, J., Steinman, L. & Galli, S. Involvement of both ‘allergic’ and ‘autoimmune’ mechanisms in EAE, MS and other autoimmune diseases. Trends Immunol. 24, 479–484 (2003). 44. Woolley, D.E. & Tetlow, L.C. Mast cell activation and its relation to proinflammatory cytokine production in the rheumatoid lesion. Arthr. Res. 2, 65–74 (2000). 45. Tanzola, M.B., Robbie-Ryan, M., Gutekunst, C.A. & Brown, M.A. Mast cells exert effects outside the central nervous system to influence experimental allergic encephalomyelitis disease course. J. Immunol. 171, 4385–4391 (2003). 46. Benoist, C. & Mathis, D. Mast cells in autoimmune disease. Nature 420, 875–878 (2002). 47. Lee, D.M. et al. Mast cells: a cellular link between autoantibodies and inflammatory arthritis. Science 297, 1689–1692 (2002). 48. Tracey, K.J. et al. Cachectin/tumor necrosis factor induces cachexia, anemia, and inflammation. J. Exp. Med. 167, 1211–1227 (1988). 49. Webster, E.L. et al. Corticotropin releasing hormone (CRH) antagonist attenuates adjuvant induced arthritis: role of CRH in peripheral inflammation. J. Rheumatol. 29, 1252–1261 (2002). 50. Dhabhar, F.S., Satoskar, A.R., Bluethmann, H., David, J.R. & McEwen, B.S. Stressinduced enhancement of skin immune function: a role for γ interferon. Proc. Natl. Acad. Sci. USA 97, 2846–2851 (2000). 51. Ader, R. & Cohen, N. Behaviorally conditioned immunosuppression. Psychosomatic Med. 37, 333–340 (1975). 52. Ader, R. & Cohen, N. Behaviorally conditioned immunosuppression and murine systemic lupus erythematosus. Science 215, 1534–1536 (1982). 53. Rogers, S.W. et al. Autoantibodies to glutamate receptor GluR3 in Rasmussen’s encephalitis. Science 265, 648–651 (1994). 54. Counce, D., Limdi, N. & Kuzniecky, R. Rasmussen’s encephalitis. Curr. Treat. Options Neurol. 3, 555–563 (2001). 55. Darnell, R.B. & Posner, J.B. Paraneoplastic syndromes involving the nervous system. N. Engl. J. Med. 349, 1543–1554 (2003). 56. Solimena, M., Folli, F., Aparisi, R., Pozza, G. & De Camilli, P. Autoantibodies to GABA-ergic neurons and pancreatic beta cells in stiff-man syndrome. N. Engl. J. Med. 322,1555–1560 (1990). 57. Baekkeskov, S. et al. Identification of the 64K autoantigen in insulin-dependent diabetes as the GABA-synthesizing enzyme glutamic acid decarboxylase. Nature 347,151–156 (1990). 58. Rosin, L. et al. Stiff-man syndrome in a woman with breast cancer: an uncommon central nervous system paraneoplastic syndrome. Neurology 50, 94–98 (1998) 59. Sakai, K., Mitchell, D., Tsukamoto, T. & Steinman, L. Isolation of a complementary cDNA clone encoding an autoantigen recognized by an anti-neuronal antibody from a patient with paraneoplastic cerebellar degeneration. Ann. Neurol. 28, 692–698 (1990). 60. Lennon, V.A & Carnegie, P.R. Immunopharmacological disease: a break in tolerance to receptor sites. Lancet 1, 630–633 (1971). 61. Patrick, J. & Lindstrom, J. Autoimmune response to acetylcholine receptor. Science 180, 871–872 (1973). 62. Engel, A.G., Tsujihata, M., Lambert, E.H., Lindstrom, J.M. & Lennon, V.A. Experimental autoimmune myasthenia gravis: a sequential and quantitative study of the neuromuscular junction ultrastructure and electrophysiologic correlations. J. Neuropathol. Exp. Neurol. 35, 569–587 (1976). VOLUME 5 NUMBER 6 JUNE 2004 NATURE IMMUNOLOGY © 2004 Nature Publishing Group http://www.nature.com/natureimmunology REVIEW 63. Drachman, D.B., Angus C.W., Adams R.N., Michelson J.D. & Hoffman G.J. Myasthenic antibodies cross-link acetylcholine receptors to accelerate degradation. N. Engl. J. Med. 298,1116–1122 (1978). 64. Steinman, L. & Mantegazza, R. The prospects for specific immunotherapy in myasthenia gravis. FASEB J. 4, 2726–2731 (1990). 65. Fetissov, S.O. et al. Autoantibodies against α-MSH, ACTH, and LHRH in anorexia and bulimia nervosa patients. Proc. Natl. Acad. Sci. USA 99, 17155–17160 (2002). 66. Steinman L. Multiple sclerosis: A two stage disease. Nat. Immunol. 2, 762–765 (2001). 67. McGeer, E.G. & McGeer, P.L. Inflammatory processes in Alzheimer’s disease. Prog. Neuropsychopharmacol. Biol. Psychiatry 27, 741–749 (2003). 68. Imamura, K. et al. Distribution of major histocompatibility complex class II-positive microglia and cytokine profile of Parkinson’s disease brains. Acta Neuropathol (Berl) 106, 518–526 (2003). 69. Moalem, G. et al. Autoimmune T cells protect neurons from secondary degeneration after central nervous system axotomy. Nat. Med. 5, 49–55 (1999). 70. Chabas, D. et al. The influence of the pro-inflammatory cytokine, osteopontin, on autoimmune demyelinating disease. Science 294, 1731–1735 (2001). 71. Karpuj, M.V. et al. Prolonged survival and decreased abnormal movements in transgenic model of Huntington’s disease, with administration of cystamine, a transglutaminase Inhibitor. Nat. Med. 8, 143–149 (2002). 72. Kerschensteiner, M., Stadelmann, C., Dechant, G., Wekerle, H. & Hohlfeld, R. Neurotrophic cross-talk between the nervous and immune systems: implications for neurological diseases. Ann. Neurol. 53, 292–304 (2003). 73. Villoslada, P. et al. Human nerve growth factor protects common marmosets against autoimmune encephalomyelitis by switching the balance of T helper cell type 1 and 2 cytokines within the central nervous system. J. Exp. Med. 191, 1799–1806 (2000). 74. Feldmann, M. & Maini, R.N. Lasker Clinical Medical Research Award. TNF defined as a therapeutic target for rheumatoid arthritis and other autoimmune diseases. Nat. Med. 9, 1245–1250 (2003). 75. Arnett, H.A. et al. TNF-α promotes proliferation of oligodendrocyte progenitors and remyelination. Nat. Neurosci. 4, 1116–1122 (2001). 76. Pluchino, S. et al. Injection of adult neurospheres induces recovery in a chronic model of multiple sclerosis. Nature 422, 688–694 (2003). NATURE IMMUNOLOGY VOLUME 5 NUMBER 6 JUNE 2004 77. Steinman, L. Collateral damage repaired. Nature 422, 671–672 (2003). 78. Yednock, T. et al. Prevention of experimental autoimmune encephalomyelitis by antibodies against α4β1 integrin. Nature 356, 63–66 (1992). 79. Hood, L., Kronenberg, M. & Hunkapiller, T. T cell antigen receptors and the immunoglobulin supergene family. Cell 40, 225–229 (1985). 80. Huh, G.S. et al. Functional requirement for class I MHC in CNS development and plasticity. Science 290, 2155–2159 (2000). 81. Joly, E., Mucke, L. & Oldstone, M.B. Viral persistence in neurons explained by lack of major histocompatibility I expression. Science 253, 11283–11285 (1991). 82. Neumann, H., Cavalie, A. Jenne, D.E. & Wekerle, H. Induction of MHC class I genes in neurons. Science 269, 549–552 (1995). 83. Steinman, L. The unexpected benefits of stealth. Neurology 42, 276–277 (1992) 84. Syken, J. & Schatz, C. Expression of T cell receptor β locus in central nervous system neurons. Proc. Natl. Acad. Sci. USA 100, 13048–13053 (2003). 85. Loconto J. et al. Functional expression of murine V2R pheromone receptors involves selective association with the M10 and M1 families of MHC class Ib molecules. Cell 112, 607–618 (2003). 86. Ishii, T., Hirota, J. & Mombaerts, P. Combinatorial coexpression of neural and immune multigene families in mouse vomeronasal sensory neurons. Curr. Biol. 13, 394–400 (2003). 87. Kumanogoh, A. et al. Class IV semaphorin Sema4A enhances T cell activation and interacts with Tim-2. Nature 419, 629–633 (2002). 88. Kuchroo, V.K., Umetsu, D.T., DeKruyff, R.H. & Freeman, G.J. The TIM gene family: emerging roles in immunity and disease. Nat. Rev. Immunol. 3, 454–462 (2003). 89. Ueda, R & Sugiyama, S. Nerve impulse in the 19th century: it’s nature and the method of research. Kgakushi Kenkyhu 42, 76–87 (2003). 90. Norcross, M.A. A synaptic basis for T-lymphocyte activation. Ann. Immunol. (Paris) 135, 113–134 (1984). 91. Huppa, J.B. & Davis, M.M. T-cell-antigen recognition and the immunological synapse. Nat. Rev. Immunol. 3, 973–83 (2003). 92. Dustin, M.L. & Colman, D.R. Neural and immunological synaptic relations. Science 298, 785–789 (2002). 93. Irvine, D., Purbhoo M., Krogsgaard M. & Davis, M.M. Direct observation of ligand recognition by T cells. Nature 419, 845–849 (2002). 94. Baylor, D.A., Lamb, T.D. & Yau, K.W. Responses of retinal rods to single photons. J. Physiol. (Lond.) 288, 613–634 (1979). 581