* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Innate Immune Response,
DNA vaccination wikipedia , lookup
Immune system wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adaptive immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Lymphopoiesis wikipedia , lookup
X-linked severe combined immunodeficiency wikipedia , lookup
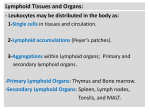
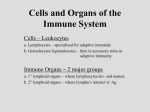
Immune system Immune System Organs Lymphoid Organs • A number of morphologically and functionally diverse organs and tissue contribute to the development of immune responses. • These organs can be distinguished by function as primary and secondary organs. • The thymus and bone marrow are the primary (or central) lymphoid organs, where maturation of lymphocytes takes place. • The secondary (or peripheral) lymphoid organs include lymph nodes, the spleen, the various mucosa-associated lymphoid tissues (MALT) such as gut-associated lymphoid tissue (GALT) and bronchus associated lymphoid tissue (BALT). These organs provide sites for mature lymphocytes to interact with antigen. Bone Marrow Bone Marrow • Bone marrow is a complex tissue that is site of hematopoisis and fat deposit. • In fact, with the passage of time, fat eventually fills 50% or more of the marrow compartment of bone. • Hematopoietic cells generated in bone marrow move through the walls of blood vessels and enter the blood stream, which carries them out of the marrow and distributes these various types to the rest of the body. Thymus Thymus • These thymocytes then move into the medulla, where they undergo further differentiation and selection and finally migrate via circulation to the secondary lymphoid organs/ tissues where they are able to respond to microbial antigens. • Most (95%) of the thymocytes generated each day in the thymus die by apoptosis with less than 5% surviving. • Molecules important to T cell function such as CD4, CD8 and T cell receptor develop at different stages during the differentiation process. • The main functions of the thymus as a primary lymphoid organ are: 1. 2. To produce sufficient numbers (millions) of different T cells each expressing unique T cell receptors such that, within this group, there are at least some cells potentially specific for huge number of microbial antigens in our environment (generation of diversity). To select for survival those T cells which bind weakly to self MHC molecules (positive selection), but then to eliminate those which bind too strongly to these same self MHC molecules (negative selection) so that the chance for an autoimmune response is minimized. Different Kinds of Dendritic Cells & Their Origins Dendritic cells Found mainly in lymphoid tissue Function as antigen presenting cells (APC) Most potent stimulator of T-cell response Different Kinds of Dendritic Cells & Their Origins Human Lymphoid System Structure of a Lymph Node Circulation of lymphocytes Structure of the Spleen The spleen is the largest lymphoid organ. It is specialized for trapping blood-borne antigens. The white pulp forms a sleeve, the periarteriolar lymphoid sheath (PALS), around the arterioles; this sheath contains numerous T cells. Closely associated with PALS is the marginal zone, an area rich in B cells Sites of effector function Primary (Central): Bone marrow Thymus Secondary (Pheripheral): Lymph nodes Spleen Peyer’s patches Lymph node distribution in the body Common Immune System of Mucous Membranes MALT (Mucous Associated Lymphoid Tissue) GALT: tecido linfóide associado ao trato gastrointestinal. Possui as placas de Peyers no íleo. BALT: tecido linfóide associado aos brônquios NALT: tecido linfóide associado ao nariz SALT: tecido linfóide associado à pele VALT: tecido linfóide associado aos vasos sangüíneos CALT: tecido linfóide associado ao olho (à conjuntiva) Mucosa Associated Lymphoid Tissue (MALT) Cross-sectional diagram of the mucous membrane ling the intestine, showing a Peyer’s patch lymphoid nodule in the submucosa. The intestinal lamina contains loose clusters of lymphoid cells and diffuse follicles. Gut Associated Lymphoid Tissue (GALT) Structure of the M cells and production of Ig A at inductive sites. M cells,situated in mucous membranes, endocytose antigen from the lumen of the digestive, respiratory, and urogenital tracts. The antigen is transported into the large basolateral pocket. Bronchus Associated Lymphoid Tissue (BALT) Cutaneous Associated Lymphoid Tissue (CALT) The skin is the largest organ in the body and plays an important role in nonspecific (innate ) defences. The epidermal (outer) layer of the skin is composed of specialized cells called keratinocytes. These cells secrete a number of cytokines that may function in local inflammatory reaction. Scattered among the epithelial-cell matrix of the epidermis are Langerhann’s cells, atype of dendritic cell, which internalize antigen by phagocytosis or endocytosis. They undergo maturation and migrate from the epidermis to regional lymph nodes, where they function as potent activators of naïve TH cells. In addition to Langerhans cells, the epidermis also contaions so-called intraepidermal lymphocytes, which are mostly T cells. The underlying dermal layer of the skin also contains scattered T cells and macrophages. Most of these dermal cells appear to be either previously activated cells or memory cells. Innate vs. adaptive immunity Cells of innate immunity Figure 13-9 Dendritic cells initiate immune responses. Immature dendritic cells constantly internalize and process proteins, debris, and microbes, when present. Binding of microbial components to Toll-Like Receptors (TLRs) activates the maturation of the DC so that it ceases to internalize any new material, moves to the lymph node, upregulates MHC II, B7 and B7.1 molecules for antigen presentation, and produces cytokines to activate T cells. Release of IL-6 inhibits release of TGF β and IL-10 by T regulatory cells. The cytokines produced by DC and its interaction with TH0 cells initiate immune responses. IL-12 and IL-2 promote TH1 responses while IL-4 promotes TH2 responses. Most of the T cells divide to enlarge the response, but some remain as memory cells. Memory cells can be activated by DC, macrophage, or B cell presentation of antigen for a secondary response.