* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download REGULATION OF KETONE BODY AND COENZYME A
Proteolysis wikipedia , lookup
Oligonucleotide synthesis wikipedia , lookup
Deoxyribozyme wikipedia , lookup
Point mutation wikipedia , lookup
Peptide synthesis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Butyric acid wikipedia , lookup
Specialized pro-resolving mediators wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
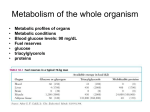
Basal metabolic rate wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Isotopic labeling wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Biosynthesis wikipedia , lookup
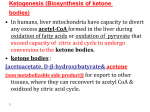
Citric acid cycle wikipedia , lookup
Biochemistry wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
REGULATION OF KETONE BODY AND COENZYME A METABOLISM IN LIVER by SHUANG DENG Submitted in partial fulfillment of the requirements For the Degree of Doctor of Philosophy Dissertation Adviser: Henri Brunengraber, M.D., Ph.D. Department of Nutrition CASE WESTERN RESERVE UNIVERSITY August, 2011 SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of __________________ Shuang Deng ____________ _ _ Doctor of Philosophy candidate for the ________________________________degree *. Edith Lerner, PhD (signed) ________________________________________________ (chair of the committee) Henri Brunengraber, MD, PhD ________________________________________________ Colleen Croniger, PhD ________________________________________________ Paul Ernsberger, PhD ________________________________________________ Janos Kerner, PhD ________________________________________________ Michelle Puchowicz, PhD ________________________________________________ June 23, 2011 (date) _______________________ *We also certify that written approval has been obtained for any proprietary material contained therein. I dedicate this work to my parents, my son and my husband TABLE OF CONTENTS Table of Contents…………………………………………………………………. iv List of Tables………………………………………………………………………. viii List of Figures……………………………………………………………………… ix Acknowledgements………………………………………………………………. xii List of Abbreviations………………………………………………………………. xiv Abstract…………………………………………………………………………….. xvii CHAPTER 1: KETONE BODY METABOLISM 1.1 Overview……………………………………………………………………….. 1 1.1.1 General introduction of ketone bodies……………………………….. 1 1.1.2 Ketogenesis is stimulated by fasting, stress and diabetes………… 1 1.1.3 Ketone body utilization in peripheral tissues………………………. 2 1.2 Adipose tissue lipolysis and regulation…………………………………….. 3 1.2.1 General introduction of lipolysis………………………………………. 3 1.2.2 Lipolysis is regulated by dietary, hormonal and neurological factors…………………………………………………………………... 3 1.2.3 Enzymes involved in lipolysis…………………………………………. 4 1.2.4 Mechanism of lipolysis…………………………………………………. 5 1.2.5 Measurement of lipolysis………………………………………………. 7 1.2.6 Adipocyte lipolysis provides substrates for ketogenesis…………… 8 1.3 Fatty acid β-oxidation and its regulation……………………………………. 9 1.3.1 Formation of acyl-CoA and its regulation……………………………. 9 1.3.2 CPT system and its regulation by malonyl- CoA, dietary and iv hormonal factors………………………………………………………... 10 1.3.3 The mitochondrial β-oxidation cycle and its regulation…………….. 12 1.3.4 Generation and utilization of acetyl-CoA…………………………….. 13 1.4 The β-hydroxy-β-methylglutaryl-CoA (HMG-CoA) cycle and its regulation.……………………………………………………………….. 14 1.4.1 Overview of the HMG-CoA cycle……………………………………... 14 1.4.2 Function of the mitochondria HMG-CoA…………………………….. 14 1.4.3 Regulation of the HMG-CoA cycle……………………………………. 14 1.5 C5-ketogenesis and its regulation…………………………………………… 15 1.5.1 Overview………………………………………………………………… 15 1.5.2 Sources of odd-chain fatty acids in animals…………………………. 17 1.5.3 C5-ketone body formation and its regulation………………………… 17 1.6 The ketone body utilization…………………………………………………... 18 1.6.1 The ketone body utilization pathway…………………………………. 18 1.6.2 The ketone body utilization in fetal liver…………………………….. 20 1.6.3 The ketone body utilization in peripheral tissues…………………… 21 1.7 The role of ketone bodies in mammalian metabolism…………………….. 24 1.8 The measurement of ketone body turnover………………………………... 25 1.8.1 The measurement of ketone body turnover with isotopic methods.. 25 1.8.2 Pseudoketogenesis…………………………………………………….. 27 CHAPTER 2: ANAPLEROSIS 2.1 Overview……………………………………………………………………….. 29 2.2 The cataplerosis……………………………………………………………… 29 v 2.3 The anaplerosis……………………………………………………………….. 31 2.3.1 The significance of anaplerosis……………………………………….. 31 2.3.2 Anaplerotic substrates…………………………………………………. 32 2.3.3 The measurement of anaplerosis…………………………………….. 35 2.3.4 The anaplerotic diet therapy…………………………………………... 36 CHAPTER 3: THE SYNTHESES OF ADENINE NUCLEOTIDES, COENZYME A (CoA) AND DEOXYRIBONUCLEIC ACID (DNA) IN RAT LIVER 3.1 Overview of the biosynthesis pathways of adenine nucleotides, CoA and DNA………………………………………………………………………... 38 3.1.1 Overview………………………………………………………………… 38 3.1.2 The biosynthesis pathway of adenine nucleotides………………… 38 3.1.3 The CoA biosynthesis pathway……………………………………….. 42 3.1.4 The DNA biosynthesis pathway………………………………………. 45 3.2 The techniques used for tracing the biosynthesis pathways…………….. 46 3.2.1 The techniques used for tracing ATP synthesis from ADP………… 47 3.2.2 The echniques used for tracing CoA synthesis……………………... 48 3.2.3 The techniques used for tracing DNA synthesis……………………. 48 3.3 Tracing the syntheses of biopolymers with [2H]water…………………….. 49 3.3.1 Overview………………………………………………………………… 49 3.3.2 Principle of the use of [2H]water to trace the biosyntheses of (pseudo)-biopolymers………………………………………………….. 50 3.3.3 General protocols of application of [2H]water……………………….. 53 vi 3.3.4 The pros and cons of using [2H]water………………………………... 54 3.3.5 Tracing the syntheses of biopolymers……………………………….. 56 CHAPTER 4: RESEARCH PROPOSAL 4.1 Project 1. C4- and C5-ketogenesis in rat liver……………………………… 62 4.2 Project 2. Tracing the syntheses of adenine nucleotides, CoA and DNA 65 in rat liver………………………………………………………….. 4.3 Publications…………………………………………………………………… 68 4.3.1 Deng S., Zhang G.F., Kasumov T., Roe C.R., and Brunengraber H. Interrelations between C4-ketogenesis, C5-ketogenesis, and anaplerosis In the perfused rat liver. J Biol Chem 284:2779927807,2009. …………………………………………………………………………… 68 4.3.2 Deng S., Zhang G.F., Kombu R.S. Harris S.R. DeSantis D., Vasquez E.J., Puchowicz M.A., Anderson V.E., Brunengraber H. Tracing the syntheses of adenine nucleotides, CoA and DNA in rat liver. To be submitted to J Biol Chem. …………………………………………………………………………… 105 CHAPTER 5: IMPLICATIONS AND FUTURE DIRECTIONS 5.1 C4-and C5-ketogenesis in rat liver…………………………………………... 146 5.1.1 Results and Discussion………………………………………………. 146 5.1.2 Future directions……………………………………………………….. 148 5.2 Tracing the syntheses of adenine nucleotides, CoA and DNA in rat liver …………………………………………………………………………... 150 5.2.1 Discussion and conclusions…………………………………………... 150 5.2.2 Future directions……………………………………………………….. 152 LITERATURE CITED…………………………………………………………….. 154 vii LIST OF TABLES Table 4.1. Apparent kinetics of the labeling of CoA and its components from 2H-enriched body water in rats over 10 and 31 days………. viii 129 LIST OF FIGURES Figure 1.1. Mechanism of adipocyte lipolysis regulation mediated by PKA… 6 Figure 1.2. Formation of ketone bodies from fatty acid partial β-oxidation…. 16 Figure 1.3. Pathway of ketone-body utilization in peripheral tissues………… 19 Figure 1.4. Pseudoketogensis in extrahepatic tissues………………………… 28 Figure 2.1. Main anaplerotic processes feeding into citric acid cycle……….. 30 Figure 3.1. Biosynthesis pathways of adenine nucleotides, CoA and DNA ………………………………………………………………………… 39 Figure 3.2. Pathway of Coenzyme A synthesis………………………………... 43 Figure 3.3. Protocol for using [2H]water to trace the rates of synthesis and degradation of biopolymers in vivo………………………………… 55 Figure 4.1. Scheme of C4-ketogenesis and C5-ketogenesis in the liver…….. 95 Figure 4.2. Comparison between the uptake of octanoate (A), heptanoate (B), or propionate (C) and the production of C4-ketone bodies and C5-ketone bodies………………………………………………… 96 Figure 4.3. Competition between octanoate and heptanoate for uptake by perfused rat livers……………………………………………………. 97 Figure 4.4. Competition between C4-ketogenesis from octanoate and C5ketogenesis from heptanoate in perfused rat livers……………… 98 Figure 4.5. Profiles of concentrations of octanoate (●) and propionate (▲) in the effluent perfusate……………………………………………… Figure 4.6. Labeling pattern of effluent β-hydroxybutyrate (BHB) and tissue acetyl-CoA from livers perfused with increasing concentrations ix 99 of [1-13C]octanoate (A) or [8-13C]octanoate (B)………………….. 100 Figure 4.7 Sharing of acetyl groups between C4- and C5-ketogenesis reflected by the mass isotopomer distribution of BHB and BHP… 101 Figure 4.8 Mass isotopomer distribution of HMG-CoA (A) and HEG-CoA (B) in livers perfused with constant 1 mM [1-13C]heptanoate and increasing concentrations of unlabeled octanoate……………….. 102 Figure 4.9 Mass isotopomer distribution of BHB-CoA and AcAc-CoA in livers perfused with increasing concentrations of [1-13C]octanoate …………………………………………………………………………. 103 Figure 4.10 Anaplerosis and glucose labeling from increasing concentrations of [13C3]propionate (♦) or [5,6,7-13C3]heptanoate (■,▲)…………………………………………………………………. 104 Figure 4.11. Sites of labeling of nucleotides, CoA and DNA from [2H]water ………………………………………………………………………... 132 Figure 4.12. In vivo labeling of liver CoA from [2H]water over 31 days……… 133 Figure 4.13. In vivo labeling of liver dR-DNA [2H] from water over 10 days… 134 Figure 4.14. Mass isotopomer distribution of liver perfusate glucose in 100% 2H2O buffer…………………………………………………... 135 Figure 4.15. Mass isotopomer distribution of glucose-6-P, ribose-5-P and PEP in livers perfused with 4 mM unlabeled glucose in 100% 2 H2O buffer………………………………………………………….. 136 Figure 4.16. M1 enrichment of AMP, ADP, ATP and CoA in livers perfused with 4 mM unlabeled glucose in 100% 2H2O buffer……………… 137 x Figure 4.17. M1 enrichment of AMP, ADP, ATP in livers perfused with 4 mM unlabeled glucose in buffers enriched 0 to 100% with 2 H2O…………………………………………………………………... 138 Figure 4.18. M1 enrichment of CoA and its components in livers perfused with 4 mM unlabeled glucose in buffers enriched 0 to 100% with 2H2O…………………………………………………………….. 139 Figure 4.19. Mass isotopomer distribution of perfusate glucose in liver perfusion experiments starting with 4 mM [13C6]glucose……….. 140 Figure 4.20. Mass isotopomer distribution of glucose-6-P, ribose-5-P and glycerate-3-P from livers perfused with 4 mM [13C6]glucose…… 141 Figure 4.21. Mass isotopomer distribution of AMP, ATP and CoA in livers perfused with 4 mM [13C6]glucose………………………………… 142 Figure 4.22. Mass isotopomer distribution of perfusate glucose in liver perfusion experiments starting with 4 mM unlabeled glucose + 2 mM [13C5]ribose………………………………………………….. 143 Figure 4.23. Mass isotopomer distribution of glucose-6-P, ribose-5-P, PEP and glycerate-3-P from livers perfused with 4 mM unlabeled glucose + 2 mM [13C5]ribose……………………………………….. 144 Figure 4.24. Mass isotopomer distribution of AMP, ADP, ATP and CoA in livers perfused with 4 mM unlabeled glucose + 2 mM [13C5]ribose………………………………………………………….. xi 145 ACKNOWLEDGEMENTS I owe many thanks and appreciations to those people who are with me during the past four years. First and foremost, I would like to thank my adviser, Dr. Henri Brunengraber. I sincerely thank him for giving me the chance to continue my education. I thank him for his scientific guidance, support, patience and humor on the 5,000 li road. He is an adviser who not only teaches me critical thinking, but also is always willing to sit and discuss every detail of my experiments, presentations and scientific writings. His guidance gives me enough confidence to face the challenge of my future endeavors. Undoubtedly, this four-year training experience has changed my life for ever. I would also give my sincere gratitude to my dissertation committee: Dr. Edith Lerner, Dr. Colleen Croniger, Dr. Paul Ernsberger, Dr. Janos Kerner and Dr. Michelle Puchowicz. Their unlimited advices and kindness helped me get through frustrating times. They witnessed my scientific growth and I deeply appreciate it. I also want to thank all my colleagues who made my life here really enjoyable. I would like to thank Dr. Guo-Fang and Dr. Rajan for offering their help whenever it was needed. I started with my first living perfusion with France David and John Koshy four years ago; This was the best team I ever worked with. I thank Stephanie Harris for sharing so many things with me. She made me feel that I am always on the “short-cut”. I had such great time work with Sharon, lan, Qinlin and Edwin. I will never forget it! I am so grateful to Fred, Brian and David, without xii their help, I could not finish my experiments. I thank Asha for cleaning my messy stuffs. Last but not least, I give my deepest thanks to Sophie for spending countless hours on my papers and figures. Finally, I want to give my special thanks to my family and my friends. My parents, my son and my husband supported me with their love in the long way. My friends were always there when I needed them. All of these friends and colleagues made me enjoy my life in this country! xiii LIST OF ABBREVIATIONS AcAc Acetoacetate ACC Acetyl-CoA carboxylase ADP Adenosine diphosphate ACBP Acyl-CoA binding protein AMP Adenosine monophosphate ATLG Adipose triglyceride lipase ATP Adenosine triphosphate BBB Blood brain barrie BHB β-Hydroxybutyrate BHP β-Hydroxypentanoate BKP β-Ketopentanoate BrdU 5’- Bromo - 2’- deoxyuridine CAC Citric acid cycle CDP Cytidine diphosphate CoA Coenzyme A CPT Carnitine-palmitoyltransferae DAG Diacylglycerol dATP Deoxyadenosine triphosphate dCTP Deoxycytidine triphosphate DNA Deoxyribonucleic acid dNTP Deoxyribonucleotide-triphosphate dGTP Deoxyguanosine triphosphate xiv dR Deoxyribose dTTP Deoxythymidine triphosphate GC-MS Gas chromatography – mass spectrometry GNG Gluconeogenesis FABP Fatty acid binding protein FOD Fatty acid oxidation disorders GABA γ-Aminobutyric acid GDP Guanosine diphosphate HEG-CoA β-Hydroxy-β-ethylglutaryl-CoA HMG-CoA β-Hydroxy-β-methylglutaryl-CoA HPLC High performance liquid chromatorgraphy HSL Hormone-sensitive lipase MCD Malonyl-CoA decarboxylase MCT Monocarboxylate transporter MGL Monoacylglycerol lipase MPE Molar percent enrichment OAA Oxaloacetate Ra Rate of appearance PC Pyruvate carboxylase PEPCK Phosphoenolpyruvate carboxylase PKA Protein kinase A PRPP Phosphoribosylpyrophosphate TDP Thymidine diphosphate xv TG Triglycerides xvi Regulation of Ketone Body and Coenzyme A Metabolism in Liver Abstract by SHUANG DENG The dietary treatment of patients with long-chain fatty acid oxidation disorders is in a transition period from classical medium-even-chain trioctanoin to mediumodd-chain triheptanoin. In my first project, I investigated the interrelations between C4- ketogenesis (production of β-hydroxybutyrate + acetoacetate), C5ketogenesis (production of β-hydroxypentanoate + ketopentanoate), and anaplerosis in isolated rat livers perfused with 13C-labeled octanoate, heptanoate, or propionate. Although the uptakes of octanoate and heptanoate by the liver are similar, the rate of C5-ketogenesis from heptanoate is much lower than the rate of C4-ketogenesis. This results from the channeling of the propionyl moiety of heptanoate into anaplerosis and gluconeogenesis. C5-ketogenesis from propionate is virtually nil because the kinetics of acetoacetyl-CoA thiolase do not favor the formation of β-ketopentanoyl-CoA from propionyl-CoA and acetyl-CoA. Anaplerosis and gluconeogenesis from heptanoate are inhibited by octanoate. The data have implications for the design of diets for the treatment of long-chain fatty acid oxidation disorders, such as the triheptanoin-based diet. xvii The goal of my second project was to sort out some of the mechanisms by which 2 H from 2H-enriched body fluids becomes incorporated into C-H bonds during the biosyntheses of adenine nucleotides, coenzyme A and DNA in rat liver. I perfused rat livers with 2H-enriched water, or buffer containing [13C6]glucose, or [13C5]ribose. The mass isotopomer distribution of glucose and glycolytic intermediates reveals intense cycling and redistribution of label through glycolysis, gluconeogenesis, the citric acid cycle and the pentose phosphate pathway. In the presence of 2H-enriched water, most of the 2H found in adenine nucleotides and CoA is incorporated between ribose-5-P and AMP. Most of the turnover of adenine nucleotides is supported by salvage pathways. In rat livers perfused with [13C6]glucose, I showed that the non-oxidative branch of the pentose phosphate pathway is more active than the oxidative branch in the fasted state. The fractional turnover rate of liver CoA is 33%/h in rat liver perfused with 100% 2H2O buffer. The fractional turnover rate of liver adenine nucleotides is 7%/h. xviii CHAPTER 1: KETONE BODY METABOLISM 1.1 Overview 1.1.1 General introduction of ketone bodies In the metabolic literature, the expression “ketone bodies” refers to three watersoluble compounds: acetoacetate (AcAc), D-3-hydroxybutyrate (BHB) and acetone (for extensive reviews of ketone body metabolism, see (1-3). Ketone bodies are strongly acidic and water-soluble compounds derived from the partial beta-oxidation of long-chain fatty acids in liver. Acetone is formed by the decarboxylation of AcAc, catalyzed by free amino groups of proteins (4). The concentrations of ketone bodies in plasma range from 0.1- 0.3 mM in the fed state (5; 6), 1-3 mM in fasting (7-11) and up to 25 mM in decompensated diabetes (12; 13). In most cases, ketone bodies are derived from even-chain fatty acids and have 4 carbons (C4-ketone bodies). When ketone bodies are derived from odd-chain fatty acids, they have 5 carbons (C5-ketone bodies, which are described in section 1.5). 1.1.2 Ketogenesis is stimulated by fasting, stress and diabetes Ketone body production is stimulated by fasting, stress or diabetes. Mobilization of lipids in white adipose tissue lipolysis releases free fatty acids, which travel through the circulating system, bound to plasma albumin and enter into the liver (14-16). The liver is the only organ that synthesizes ketone bodies (1). Under some special conditions (such as suckling), ketogenesis also occurs in the small intestine, kidney and brain astrocytes (17). Long-chain fatty acids are converted to long-chain acyl-CoAs in the hepatocyte cytosol. These CoA esters are then 1 transported into the mitochondria via the carnitine palmitoyltransferase (CPT) system (1; 14; 18). Malonyl-CoA inhibits CPT I and regulates the entrance of long-chain acyl-CoAs into the mitochondria (19; 20). Soluble medium-chain fatty acids (8-10 carbons) enter directly into the mitochondria and their oxidation is independent of the CPT system (1). In the mitochondria, fatty acids are oxidized to acetyl-CoA. The liver, a small organ (2-3% of body weight), cannot oxidize all the acetyl-CoA derived from fatty acid β-oxidation. The excess acetyl-CoA (80% of the nonesterified fatty acids carbons going down β-oxidation) enters the βhydroxy-β-methylglutaryl-CoA (HMG-CoA) cycle and produces ketone bodies (1). 1.1.3 Ketone body utilization in peripheral tissues For a long time, ketone bodies were regarded as harmful because high concentrations of acidic ketone bodies accumulate in decompensated diabetics (12; 13). However, ketone bodies are good fuels for peripheral tissues if the capacity of these tissues to utilize ketone bodies is not inhibited by a large supply of competing substrates such as glucose (2). Ketone body utilization occurs by two pathways: oxidation in the mitochondria of non-hepatic tissues (21) and lipogenesis in the cytosol of liver, lactating mammary gland, and developing brain (22; 23). Ketone bodies provide alternative fuels to peripheral tissues when glucose is in short supply or cannot be efficiently used. This is especially important for the brain because glucose is its main energy substrate (2). Owen et al. (24) found that the brain can also use ketone bodies during extended starvation. The developing brain uses ketone bodies to synthesize lipids (25-27). 2 Ketone body utilization spares muscle proteins in starvation (28). The lactating mammary gland uses ketone bodies to synthesize milk lipids (29). 1.2 Adipose tissue lipolysis and regulation 1.2.1 General introduction of lipolysis In mammals, about 95% of body fats are stored in adipose tissue during abundant energy supply. A small amount of fat is found in muscle, liver and pancreas (30). The fats are stored mostly as hydrophobic lipids – triglycerides (TGs). In adipose tissue, the fats are mobilized when there is a shortage of dietary substrates (31). Body fat distribution is different between man and woman. Females have more total body fat and a higher percentage of lower body fat than males do (32). In addition to supplying stored energy for the body, adipose tissue is also an endocrine organ which secretes adipokines (31). Adipose tissue has two main metabolic functions: lipogenesis and lipolysis. Lipolysis is a process by which triglycerides are hydrolyzed to fatty acids and glycerol. It occurs in extracellular space, regulated by lipoprotein lipase in postprandial conditions, and in intracellular space mediated by hormonesensitive lipase. Adipocyte lipolysis controls the release of fatty acids into the circulating system and is a major regulator of lipid metabolism (33). 1.2.2 Lipolysis is regulated by dietary, hormonal and neurological factors Lipolysis is highly reglulated by diet, hormonal and neural factors. Variations in dietary composition have obvious effects on TG lipolysis. Ingestion of a high fat diet increases glycerol release in gut. A high carbohydrate decreases glycerol release in gut (34). Leptin, glucocorticoids, glucagon, catecholamines, T3 and T4 3 are lipolytic hormones that stimulate lipolysis (31). Insulin, prostaglandins, IL-6 are antilipolytic and reduce lipolysis (34). The most important hormonal factors are lipolytic catecholamines and antilipolytic insulin. Catecholamines are “fight or flight” hormones produced by the adrenal glands and sympathetic nerves: they respond to stress. The most abundant catecholamines are epinephrine, norepinephrine and dopamine. Catecholamines trigger lipolysis by increasing cAMP and activating protein kinase A (PKA) (30). Another potent lipolytic compound, atrial natriuretic peptide, triggers lipolysis during repeated bouts of exercise (35). Catecholamine resistance is found in obese patients, caused by the decreased number of β2-adrenoreceptors. Catecholamine resistance contributes to reduced lipolysis both in vivo and in vitro (36). In contrast, the most important antilipolytic hormone insulin blocks lipolysis via degrading cAMP and activating protein phosphatase (37). 1.2.3 Enzymes involved in lipolysis Hormone-sensitive lipase (HSL) Hormone-sensitive lipase (HSL) is the rate-limiting enzyme of lipolysis. Its activity is regulated by catecholamines and insulin. The structure of HSL from rat adipose tissue was first identified by Holm’s group (38). It consists of 768 amino acids and the molecular weight is 84 kDa (39). The phosphorylation sites responding to lypolytic stimulations are within 150 amino acids close to the Cterminal (40). HSL is mainly expressed in adipose tissue (41), but it is also found in muscle (42), macrophages (43) and pancreatic β-cells (44). Obese people have decreased adipocyte HSL activity and expression. This contributes to the 4 decrease of lipolysis and the increases in adipose tissue mass (45). Fatty acids also inhibit the HSL hydrolytic function; this inhibition is reduced by HSL binding to adipocyte lipid-binding protein both in vivo and in vitro (46). Adipose triglyceride lipase (ATGL) Another lipase with triacylglycerol hydrolase activity is adipose triglyceride lipase (ATGL) (also called desnutrin or phospholipase A2)(47). ATGL is highly expressed in adipose tissue with a higher activity to hydrolyze triacylglycerols than HSL. ATGL predominates in basal lipolysis (48). ATGL-null mice show disruption of energy homeostasis by the defective lipolysis (49). ATGL does not respond to catecholamines. Unlike HSL, ATGL cannot be phosphorylated by PKA (50): it is under the control of peroxisome proliferator-activated receptor γ and insulin (51). Monoacylglyerol lipase (MGL) Monoacylglycerol lipase (MGL) is a necessary enzyme to hydrolyze monoacylglycerols to free fatty acids and glycerol (30). This enzyme is not under hormonal regulation and is not the rate-limiting step in lipolysis (52). 1.2.4 Mechanism of lipolysis A well known control mechanism of lipolysis is exerted by the regulation of HSL (Fig 1.1). This regulation is mediated by cAMP and protein kinase A (PKA) (53). β-adrenergic catecholamines, the release of which is triggered by the sympathetic nervous system, increase during fasting, physical exercise or stressful conditions. They bind to G-protein coupled β-adrenoreceptors, which 5 Figure 1.1: Mechanism of adipocyte lipolysis regulation mediated by PKA. Modified from Fukao et al. (54) Prostaglandins, Leukotrienes and Essential Fatty Acids 70 (2004): 243-251. 6 activate adenyl cyclase and increase intracellular cAMP concentration (55). The and Ser660 residues (41). PKA also phosphorylates perilipin, which is a protein located on the surface of lipid droplets and blocking the contact of HSL with lipids (56). There are two possible mechanisms by which phosphorylated perilipins influence lipolysis. Londos et al. (57) reported that once perilipins are phosphorylated, they disassociate from the lipid droplets and leave the lipid surface for the activated HSL. Another mechanism proposed by the Granneman group (58; 59) is that perilipins are “scaffold proteins”. The phosphorylated perilipins change their structures and recruit HSL to access the lipid surface. ATGL and HSL together hydrolyze 95% of TGs to diacylglycerol (DAG) in mouse adipose tissue (60). HSL continues to hydrolyze DAG to MAG. MGL is the last enzyme that converts MAG to one glycerol and one fatty acid molecule. The released fatty acid and glycerol bound to transporters are exported into the blood (30). 1.2.5 Measurement of lipolysis Adipocyte lipolysis is measured both in vivo and in vitro. In vivo measurements provide more accurate and reliable results than in vitro measurements because all physiological influence come to play (61). Triglycerides are hydrolyzed to free fatty acids and glycerol in a 3/1 ratio. If the ratio is lower than 3:1, this means that some free fatty acids have been reesterified in adipose tissue (62). Plasma free fatty acid and glycerol concentration are indicators of adipose tissue lipolysis. Radioactive or stable tracers are reliable techniques to determine systemic lipolysis in vivo (33). Stable isotopes techniques use gas-chromatography, HPLC 7 and mass spectrometry techniques. Tracers of free fatty acids (63; 64) or glycerol (65) are infused in vivo, and the appearance rate (Ra) of free fatty acids and glycerol are determined from their steady-state labeling in plasma. Palmitate or oleate are good tracers because the Ra of these single fatty acids reflects the Ra of plasma total free fatty acids. Local lipolysis is mostly determined by arteriovenous (A-V) differences or microdialysis (33). A-V differences are based on the measurement of metabolite concentrations across subcutaneous adipose tissue (66). Microdialysis uses semipermeable dialysis catheters implanted in a tissue, and analyzes the metabolite concentrations in the effluent dialysis fluid. However, this method can only measure the interstitial glycerol not fatty acid concentration because fatty acids are not dialyzed via standard dialysis membranes (67). 1.2.6 Adipocyte lipolysis provides substrate for ketogenesis TG lipolysis in adipose tissue (adipocyte lipolysis) is the first key step for ketogenesis since it provides ketogenic substrates (free fatty acids) to the liver. Scow et al. (68) found that in pancreatectomized rats depleted of adipose tissue, there was no ketosis, even at extremely low level of insulin. Under modest starvation conditions, plasma free fatty acid concentration is less than 1 mM, and ketone body level is lower than 5 mM. However, in decompensated diabetes, the free fatty acid level ranges from 2 - 4 mM, which increases ketone body concentration to 20 mM (69; 70). Although free fatty acids and ketone bodies are “precursor and product”, the nonparallel relation between the fatty acid and ketone body levels results from variations in the esterification rate (71). 8 1.3 Fatty acid β-oxidation and its regulation 1.3.1 Formation of acyl-CoA and its regulation It is still not clear whether long-chain fatty acids enter hepatic cells via diffusion (72) or protein-mediated fatty acid transporters. Transported insoluble long-chain fatty acids (normally C14-18) bind to cytosolic fatty acid binding proteins (FABP), which decrease the potential toxicity of free fatty acids (17). Inhibition of the binding potentially decreases fatty acid flux in liver (73). Long-chain acyl-CoAs are formed by acyl-CoA synthetases, which are present in mitochondria (74), peroxisomes (75) and endoplasmic reticulum (76). The ratio of NAD/NADH is a major control of β-oxidation. Even if the formation of acyl-CoA is not a major control site of β-oxidation, the ratio of [acyl-CoA]/[CoASH] affects β-oxidation flux via regulation of acyl-CoA synthetase in vitro (17). Before acylCoA binding protein (ACBP) was isolated from mammalian tissues, acyl-CoAs were found binding to FABPs (17). ACBP has a very high affinity for long-chain acyl-CoAs; this minimizes the hydrolysis of the esters (77). It is generally accepted that the activated fatty acids are used by two metabolic pathways in liver: cytosolic lipid synthesis via glycerol-3-phosphate, and mitochondrial oxidation. The two processes are highly regulated. Three proposed pathways for delivering fatty acids from plasma to mitochondria were summarized by Eaton (17): first, fatty acids enter the cytosol via transporter proteins and bind to FABPs. They are either converted to acyl-CoAs in the plasma membrane or in the cytosol. Second mechanism is that the ACBP-bound acyl-CoAs move to the mitochondrial outer membrane. The third mechanism makes fatty acids bind to 9 FABP and migrate to the mitochondrial membrane, where they are converted to acyl-CoAs. 1.3.2 The CPT system and its regulation by malonyl - CoA, dietary and hormonal factors The mitochondrial carnitine palmitoyltransferase (CPT) system and its regulation The transport of long-chain fatty acyl-CoAs from cytosol to mitochondria is highly dependent on the CPT system. Acyl-CoAs are first converted by carnitine palmitoyl-transferase I (CPT I) at the outer mitochondrial membrane to acylcarnitines, which are transferred to the mitochondrial matrix via a translocase. Finally, mitochondrial carnitine-palmitoyl-transferase II (CPT II) catalyzes the reconversion of acylcarnitines back to acyl-CoAs. Unlike long-chain fatty acids, short-chain or medium-chain fatty acids bypass the carnitine system and directly enter into mitochondria, where they are acylated to acyl-CoAs by mitochondrial acyl-coA synthetase (17). As a result, the oxidation of short-chain or medium-chain fatty acids is independent of CPT I regulation. The concept that CPT I is the control site for hepatic β-oxidation originated from data generated in rat livers perfused with octanoate (1). McGarry (1) et al. found that the octanoate oxidation rate is similar in livers from fed and fasted rats. However, the oleate β-oxidation rate varies with nutritional conditions (1). This is because octanoate directly enters mitochondria independent of the CPT I system. This finding lead to the understanding that CPT I is subject to metabolic regulation. CPT I has two isoforms: L-CPT I in liver and M-CPT I in muscle, 10 which have different kinetic properties (54). CPT I is regulated by fuel status (fatty acids, ketone bodies, glucose) via controlling malonyl-CoA and hormonal levels (78). Malonyl-CoA regulation In the liver, malonyl-CoA is a signaling metabolite as well as an intermediate of fatty acid synthesis (79). The concentration of hepatic malonyl-CoA level is about 13 nmol•g-1 in the fed state; it decreases to half in the fasted state (80). MalonylCoA is the product of acetyl-CoA carboxylase (ACC), the activity of which is highly up-regulated by insulin and down-regulated by glucagon and AMPK. The increased glucogon or epinephrine raises cAMP levels which lead to the activation AMPK. AMPK phosphorylates ACC and inhibit its enzyme activity. Insulin activates a phosphatase to dephosphorylate ACC and makes it inactive. Thus, ACC has for a long time been considered as the major enzyme responsible for the changes in malonyl-CoA level (81). Another relevant enzyme is malonyl-CoA decarboxylase (MCD) which converts malonyl-CoA to acetyl-CoA and provides a way to dispose of malonyl-CoA. Whether MCD is regulated by AMPK are in debate. Park et al. (82) showed that MCD are positively regulated by AMPK in rat liver, muscle and adipose tissue after exercise. The opposite opionin was proposed by Habinowski et al. (83). They found that MCD is not a substrate in fast twitch muscle and 832/13 ISN-1 islet cell line. The inhibition of MCD increases malonyl-CoA concentration and decreases β-oxidation (84). ACC and MCD work together to control cytosolic malonyl-CoA which regulates CPT I activity. 11 Malonyl-CoA plays an important role during the transition from the fed to the fasted states by switching hepatic fatty acid metabolism from synthesis to oxidation and ketogenesis. In the normal fed state, malonyl-CoA inhibits CPT I and thus decreases the transport of long-chain fatty acyl-CoAs into mitochondria: this leads to the decrease in acyl-CoA oxidation. However, in the fasted state, liver CPT I is less sensitive to malonyl-CoA because of an increased Ki (85). Upon refeeding, insulin restores the sensitivity of CPT I to malonyl-CoA within 24 hours (86; 87). Other studies concluded that the desensitization may be caused by changes in the CPT I membrane environment (79). Hormonal regulation The [glucagon]:[insulin] ratio affects the carnitine acyltransferase reaction. The liver carnitine content increases with the increase of the [glucagon]:[insulin] ratio (88). Insulin and glucagon regulate the L-CPT I gene expression (89). The addition of glucagon to cultured fetal hepatocytes increases L-CPT I mRNAs. In contrast, insulin depresses CPT-I mRNA abundance to about 10-fold in 8 hr in H4IIE rat hepatoma cells (90). 1.3.3 The mitochondrial β-oxidation cycle and its regulation The β-oxidation cycle in mitochondria catalyzes the sequential removal of twocarbon units from the acyl-CoA chain. By this process, fatty acids are converted into acetyl-CoA to produce energy. Four intramitochondrial enzymes regulate this cycle. Acyl-CoA dehydrogenases catalyze the first step of β-oxidation cycle and convert acyl-CoAs to enoyl-CoAs. There are three isozymes of acyl-CoA dehydrogenases, each of them is responsible for specific fatty acyl chain lengths. 12 Acyl-CoA dehydrogenase has the lowest activity of the β-oxidation enzymes in rat tissues (91; 92). One of the most common fatty acid oxidation disorder (FOD) affects very long-chain acyl-CoA dehydrogenase. Those patients accumulate toxic long-chain or very long-chain fatty acyl-CoA in cells. This damages cell membrane (93). The second step of β-oxidation is the formation of βhydroxyacyl-CoAs from enoyl-CoAs catalyzed by enoyl-CoA hydratase. This step is not a control point of β-oxidation (17). In the third step, β-hydroxyacyl-CoAs are dehydrogenated to β-ketoacyl-CoA by β-hydroxyacyl-CoA dehydrogenase. The final step of the β-oxidation cycle is catalyzed by 3-ketoacyl-CoA thiolase, which releases one acetyl-CoA molecule. The last three enzymes are linked together in a trifunctional protein. The complete deficiency of this enzyme is rare and causes sudden death (94). 1.3.4 Generation and utilization of acetyl-CoA Early studies claimed that oxaloacetate (OAA), a citric acid cycle (CAC) intermediate, is a primary regulator of ketogenesis in vivo (95). The low level of anaplerosis would decrease acetyl-CoA flux to the CAC, and increase the conversion of acetyl-CoA to ketone bodies. Williamson et al. (96) disagreed with this mechanism. By perfusing radioactive labeled octanoate in rat livers under different physiological conditions, they showed that enhanced hepatic fatty acid β-oxidation produces more acetyl-CoA than can be oxidized by the CAC. The acetyl-CoA builds up and flows to the ketogenic pathway. The latter mechanism is generally accepted today. 13 1.4 The β-hydroxy-β-methylglutaryl-CoA (HMG-CoA) cycle and its regulation 1.4.1 Overview of the HMG-CoA cycle HMG-CoA is produced by different cytosolic and mitochondrial HMG-CoA synthases. It is a key branch point for hepatic cholesterogenesis in the cytosol and for ketogenesis in the mitochondria (97). In 1950’s, Rudney proved that acetyl-CoA and AcAc-CoA react to form HMG-CoA in rat and beef liver mitochondria (98). HMG-CoA then undergoes a cleavage to form acetoacetate and acetyl-CoA (139). The ketogenic pathway is also called the HMG-CoA cycle (97). In the cytosol, HMG-CoA is reduced to mevalonate, an intermediate of cholesterogenesis (97). 1.4.2 Function of the mitochondrial HMG-CoA The formation of ketone bodies in the liver occurs via the HMG-CoA cycle. The old view was that thiolase catalyzes the condensation of two molecules of acetylCoA to produce acetoacetyl-CoA (AcAc-CoA), which reacts with another acetylCoA molecule to form HMG-CoA, the latter is cleaved to AcAc. However, AcAcCoA is actually derived from the last four carbons of long-chain fatty acids that undergo β-oxidation. The rate limiting step of ketogenesis is the formation of HMG-CoA (see figure 1.2). 1.4.3 Regulation of the HMG-CoA cycle Hepatic mitochondrial HMG-CoA synthase and HMG-CoA lyase are responsible for ketogenesis. The absence of one or both enzymes causes the incapability to synthesize ketone bodies in liver. Mitochondrial HMG-CoA synthase in avian 14 liver is a homodimer consisting of two 53-57 kDa monomers (99). This enzyme was first identified as a control site for ketogenesis by Williamson’s group in 1968 (23). In 1975, Lane’s group proved that mitochondrial and cytosolic HMG-CoA synthases have different chemical structures and functions (97) Covalent modification by succinyl-CoA is the main mechanism of regulation of mitochondrial HMG-CoA synthase activity (100). Succinyl-CoA binds reversibly to HMG-CoA synthase to form an inactive succinyl-enzyme complex. This inactive enzyme converts to active enzyme via the release of succinate (101). In the fasted state, increased glucagon lowers mitochondrial succinyl-CoA level and hepatic ketogenesis is stimulated via desuccinylation of HMG-CoA synthase (102). Moreover, a high fat or a high carbohydrate diet (103) decreases HMGCoA synthase activity. 1.5 C5-Ketogenesis and its regulation 1.5.1 Overview β-Hydroxypentanoate (BHP) and β-ketopentanoate (BKP) are homologues of the physiological ketone bodies BHB and AcAc. They derive from the partial-oddchain fatty acid β-oxidation. Odd-chain fatty acids are absent from the diet of non-ruminant mammals, thus only trace amounts of C5-ketone bodies are found in human plasma. The oxidation of 1,3-pentanediol, a potential animal nutritent, in dog liver produce C5- ketone bodies (104). In the clinical field, BHP and BKP were found in the urine of patients who have inherited deficiency of propionylCoA carboxylase (105). Instead of acetyl-CoA, the accumulated body propionylCoA is carboxylased by ACC to form odd-chain fatty acids, which are oxidized to 15 Fatty acids β-oxidation O (AcAc-CoA) O CH3-C-CH2-C-SCoA O (Ac-CoA) HMG-CoA Synthase CH3-C-SCoA (HMG-CoA) O OH O C CH2 CH2 C C CH3 O SCoA CH3-C-SCoA HMG-CoA lyase O O -OOC-CH2-C-CH3 (Acetoacetate) Acetoacetate decarboxylase O D-β-hydroxybutyrate dehydrogenase CO2 CH3-C-CH3 OH -OOC-CH2-CH-CH3 D-β-hydroxybutyrate Acetone Figure 1.2: Formation of ketone bodies from fatty acid partial β-oxidation. 16 form C5-ketone bodies via HMG-CoA cycle. The clinical names of BHP and BKP are 3-hydroxyvelerate and 3-oxovalerate which are considered as abnormal metabolites (105). Plasma C5-ketone bodies are also reported in patients who have long-chain FOD, and are treated with anaplerotic triheptanoin diet (106). 1.5.2 Sources of odd-chain fatty acids in animals Odd-chain fatty acids are absent or present in only trace amounts in most plants (107). Humans acquire odd-chain fatty acids mainly from ruminant milk. They are produced by rumen bacteria via de novo synthesis (108). Thus, the concentration of milk odd- and branched-chain fatty acids serve as a biomarker of the duodenal microbial flora (109). A small amount of odd-chain fatty acids is produced from de novo synthesis in the ruminant mammary gland. Odd-chain fatty acids are synthesized using propionyl-CoA as the primer instead of acetylCoA (110). 1.5.3 C5-ketone body formation and its regulation Like C4-ketone bodies, C5-ketone bodies are synthesized in liver mitochondria from the partial β-oxidation of odd-chain fatty acids. After several β-oxidation cycles, odd-chain fatty acids generate BKP-CoA. C5-ketone body production uses the HMG-CoA cycle. The counterpart of HMG-CoA in C5- ketogenesis is 3hydroxy-3-ethylglutaryl-CoA (HEG-CoA). Incubation of liver extract with propionyl-CoA and [1-14C]acetyl-CoA produces [14C]HEG-CoA (111). BHP and BKP are interconverted by mitochondrial BHB dehydrogenase (112). In patients with deficiency of biotin (113) or vitamin B12 (114), C5-ketone bodies are found in body fluids. The formation of C5-ketone bodies involves either the conversion of 17 propionyl-CoA to BKP-CoA via 3-oxoacyl-CoA thiolase or the β-oxidation of oddchain fatty acids (115). 1.6 The ketone body utilization 1.6.1 The ketone body utilization pathway Under normal physiological conditions, the production of ketone bodies in liver is well balanced by their utilization in peripherial tissues. Ketone bodies are produced during starvation as alternative substrates. Ketone bodies are used as fuels for energy and lipogenesis (2). AcAc is the ketone body directly used in peripherial tissues. BHB is first converted into AcAc by 3-hydroxybutyrate dehydrogenase (116). The utilization of AcAc includes 2 steps: the first step is the conversion of AcAc to its CoA ester, the second step is the formation of acetyl-CoA (see figure 1.3). The formation of acetoacetyl-CoA is catalyzed by two different enzymes: (i) AcAc + succinyl-CoA ↔ acetoacetyl-CoA + succinate This reaction is catalyzed by 3-oxoacid-CoA transferase, which is a mitochondrial enzyme that is absent in liver (19), but is present in peripherial tissues. This reaction is reversible. (ii) AcAc + ATP + CoA → AcAc-CoA + AMP + pyrophosphate Acetoacetyl-CoA synthetase catalyzes this irreversible reaction. This cytosolic enzyme has lower enzymatic activity than 3-oxoacid-CoA transferase (117). The second step is the cleavage of acetoacetyl-CoA into 2 acetyl-CoA by acetoacetyl-CoA thiolase. Acetoacetyl-CoA + CoA ↔ 2 acetyl-CoA 18 Figure 1.3: Pathway of ketone-body utilization in peripheral tissues. Modified from Williamson DH et al. (2) Physiol Rev 60: 13-187, 1980. a: 3-hydroxybutyrate dehydrogenase; b: 3-oxoacid-CoA transferase; c: acetoacetyl-CoA thiolase; d: citrate synthase; e: acetoacetyl-CoA synthetase; f: ATP citrate lyase; g: acetoacetyl-CoA reductase or β-ketoacyl-ACP reductase; h: enoyl-CoA hydratase or β-hydroxyacyl-ACP dehydrase; i: enoyl-CoA reductase, enoyl-ACP reductase, or enoyl-ACP reductase (NADPH); j; 3-hydroxybutyrylCoA synthetase or butyryl-CoA synthetase. 19 This reversible reaction occurs in mitochondria. It strongly favors the formation of acetyl-CoA rather than acetoacetyl-CoA. Acetoacetyl-CoA thiolase is also found in the cytosol (118), where it is part of the synthesis of lipids (119). C5-ketone bodies are metabolized in a similar way to C4-ketone bodies (104). The administration of BHP and BKP to conscious dogs in a dose corresponding to 75% of caloric requirement leads to only 1.3 mM plasma C5-ketone body concentration (104). This shows the rapid metabolism of C5-ketone bodies. BHP is first oxidized to BKP by BHB dehydrogenase present in most cells, followed by converting of BKP to its CoA ester: BKP-CoA in peripheral tissues by 3-oxoacidCoA transferase. The last step is the cleavage of BKP-CoA to acetyl-CoA and propionyl-CoA for energy utilization. 1.6.2 The ketone body utilization in fetal liver The normal adult liver is traditionally considered as a ketone body producer but not a ketone utilizer because of the absence of 3-oxoacid-CoA transferase (120). A study reported a low activity of 3-oxoacid-CoA transferase in normal rat liver (23). This report was disputed based on labeling patterns of ketone bodies in liver which are incompatible with the presence of 3-oxoacid transferase (121). However, the fetal liver uses ketone bodies for lipogenesis. The increased insulin dephosphorylates ACC via a phosphatase and increase the lipids synthesis in fetal liver. The mammalian fetus uses glucose supplied by the mother as the main energy substrate (122). During the late pregnancy period, the mother has increased ketone body levels (123) and pregnant rats develop hyperketonemia 20 very fast (124). The increased ketone bodies are transported from mother to fetus; the fetal liver acts like a peripherial tissue as reflected by the increased activity of ketone-utilizing enzymes (125). Yokoo et al. (126) found that ketone bodies are oxidized in isolated hepatocytes from fetal liver, and that BHB is utilized faster than AcAc. 1.6.3 The ketone body utilization in peripheral tissues The ketone body utilization in brain (developing and adult) The brain and nervous tissues use glucose as the primary energy substrate for energy production (127; 128). A shift in energy substrate utilization (129) (129; 129)from glucose to ketone bodies occurs under certain nutritional conditions during fasting, feeding a high-fat diet (130) and early development and throughout the suckling period (131). Ketone bodies have become a potential therapeutic agent for the treatment of seizure disorders, Alzheimer’s and Parkinson’s diseases, which are caused by the malfunctions of brains (132). As monocarboxylates, the uptake of ketone bodies by brain is highly dependent on their transport across the blood brain barrier (BBB), and thus any therapeutic strategy involving the use of KB’s should include a component for conditions when KB uptake by brain is maximal. The first step to transport ketone bodies is via monocarboxylase transporter (MCT-1), which is a primary carrier-mediated transporter and locates in the endothelial cell membranes of BBB (133). The exact location of this transporter in rat brain endothelium and glia has been identified by Gerhart et al. by using immunoelectron microscopy technique (134). MCT-1 is regulated in brain by nutritional status such as with feeding the 21 ketogenic diet (135). It has been shown that MCT-1 significantly increased in the brain of the rats treated with ketogenic diet compared to the rats on a regular chow (135; 136). “NOTES Summary on the use of diet or any conditions such as with infusion, the transport capacity is limiting must be considered before the treatment can be efficient ore effective.” Tracer conditions are not an issue but transport capacity is. The mature brain uses glucose as the main energy substrate in the fed state. The circulating ketone body concentration is a main regulator of ketone body utilization in the brain (137). The decreased permeability to BHB of the adult brain shows that compared to the suckling rat brain, the mature brain relies more on glucose than on ketone bodies (138) . Ketone bodies in adult brains are mostly used for oxidation to produce energy and not for the syntheses of lipids (139; 140). The developing rat brains are different from adult brains. After birth, circulating ketone bodies in the suckling pups reach between 1-2 mM (hyperketonemic condition) (141) because of the high fat content of maternal milk (142). The capacity of the ketone body transporter is high during the suckling period (138). In the developing rat brain, ketone bodies are lipogenic. In suckling rat brains, ketone bodies are also important precursors for the synthesis of cholesterol, which is very important for the brain growth (143). AcAc is rapidly incorporated into brain cholesterol during the first week of life (25). Ketone bodies are also 22 used to synthesize other types of lipids such as phospholipids and sphingolipids, which are required for brain development (144). The ketone body utilization in the lactating mammary gland During lactation, substrates such as glucose, lactate, pyruvate (145) and ketone bodies are used for lipogenesis in the lactating mammary gland. In ruminants, over 90% of milk fat consists of fatty acids or triglycerides. Humans’ breastmilk have even more fat than the rumints. One of the sources of the fatty acids is the de novo synthesis from acetate and BHB. The latter is produced by the rumen epithelial from absorbed butyrate (146). The ketone-body utilization enzymes show high activities in the lactating mammary gland of fed lactating rats (147). Incubation experiments with ketone bodies and [3H]water showed that ketone bodies increase the fatty acid synthesis rate in slices of mammary gland of lactating rats (148). The incorporation of [314 C]BHB into lipid in the mammary gland was 5-fold higher than in the liver. Insulin increased this lipid incorporation (29). Given that the oxidation of [314 C]AcAc accounted for 65% of the net ketone-body utilization in vitro (147), the mammary gland is regarded as the major tissue of ketone-body utilization in fed lactating rats. However in starved lactating rats, ketone-bodies are not used as an alternative substrate to glucose (169). The ketone body utilization in kidney and heart The kidney is an important user of ketone bodies. Experiments in nephrectomized rats showed that the kidney removes about 30% of total body ketone bodies (149). During prolonged starvation, obese subjects have increased 23 renal reabsorption rate of AcAc and BHB. This minimizes ammonium loss through urine and prevents the breakdown of body proteins(150). The heart uses glucose and fatty acids as main energy substrates in the fed state. However, during starvation, this organ has the highest ketone body utilization rate (2). The uptake of plasma ketone bodies is proportional to their circulating concentrations (151). The perfused rat heart completely oxidizes ketone bodies. This process can account for up to 75% of the organ’s oxygen consumption (152). 1.7 The role of ketone bodies in mammalian metabolism Ketone bodies were originally considered to be harmful because of their association with uncontrolled diabetes. The ketone bodies accumulate up to 25 mM in diabetic patients’ plasma (1). It causes the changed body pH, disrupted electrolyts balance and cardiac arrest. On the other hand, this wide range of concentrations shows that ketone body concentration is a sensitive physiological index of metabolic changes. Ketone bodies are alternative fuels during fasting and hypoglycemic conditions (12). In peripherial tissues, especially in the nervous system, ketone bodies decrease glucose utilization and inhibit proteolysis (153). They are important lipogenic precursors in fetal liver, lactating mammary gland and developing brain (2). Nowadays, ketone bodies are not considered only as energy substrates in peripherial tissues. Ketone bodies are involved in whole-body metabolism because they are the signal of lack of carbohydrates. They may also play important role in the regulation of proteolysis (2). Although there is no direct 24 evidence to show the inhibition of ketone body on protein breakdown, the use of ketone bodies spares the muscle proteins is a good physiological consideration. 1.8 The measurement of ketone body turnover 1.8.1 The measurement of ketone body turnover with isotopic methods Overview of measurement of ketone bodies Ketone body turnover is generally assessed by two methods in vivo: hepatic arteriovenous difference (154) and isotopic method (155). Compared to the arteriovenous difference technique, isotopic-dilution technique is more applicable because it is noninvasive. Thus, this technique is suitable for humans. The isotopic method is used to measure the steady-state ketone body turnover rate (155). Two isotopic methods have been applied to trace ketone body turnover: single-isotope and double (dual)-isotope techniques. The general principle is to infuse radioactive or stable-isotope labeled ketone bodies into a vein, and then measure the specific activity or labeling of ketone bodies in the arterial plasma. The dilution of specific activity reflects the rate of hepatic ketogenesis. Different isotope labeled tracers including 2H-, 3H-, 13 C-,14C-ketone bodies have been used (7; 156; 157). Single-Isotopic method The single-isotope technique used either [14C]AcAc or [14C]BHB to measure ketone body production or utilization rate, using the “total ketone body specific activity” describled by McGarry et al. (158). However, the disequilibrium of labeling between the two ketone bodies was not taken into account by the calculation. Although AcAc and BHB are interconverted very fast, the specific 25 radioactivity of the two substrates takes a long time to reach equilibrium (159). Despite the above problem, ketone body kinetics has been extensively used in animals and humans. In diabetic dogs, total ketone body production rate is 38.1 ± 5.6 μmol/kg•min, which is much higher than that of the control group: 11.4 ± 1.9 μmol/kg•min (155). Balasse (190) showed that in obese fasting patients, infusion of [14C]AcAc or [14C] BHB results in similar production rate of total ketone bodies: 1908 ± 80 μmol/min. This result is almost double as that from Wolfe’s group (160). Double-isotopic method A double-isotope (dual-isotope) technique was also used to evaluate ketogenesis in vivo. The general equation used for the measurement is following (161): Ra = [I- (C x V x dSR / dt)] / SR Ra: is the rate of appearance for the individual ketone body; I: is the tracer infusion rate; C: is the concentration; V: is the assumed volume distribution (35% of body weight); SR: is the specific radioactivity. Reed et al. (161) used [4-3H] and 14 C-labeled ketone bodies to study the kinetics of ketone-bodies in the rat. They simultaneously infused [3-14C]AcAc and [43 H]BHB into rats. The two different tracers yielded similar kinetics of ketone bodies. Miles et al. (162) compared single-isotope and dual isotope techniques. When they infused [14C]BHB alone or simultaneously infused [13C]AcAc and [14C]BHB in mongrel dogs, basal ketone body turnover were similar: 2.2 ± 0.2 μmol/kg•min and 2.7 ± 0.2 μmol/kg•min, respectively. But infusion of [13C]AcAc 26 overestimated the turnover by 55%. This shows that the choice of a single tracer affects the measurement. 1.8.2 Pseudoketogenesis Isotopic artifacts may overestimate ketone body turnover. When labeled AcAc or BHB is infused and enters extrahepatic tissues such as heart or muscle (163). AcAc is activated to AcAc-CoA via 3-oxoacid-CoA transferase. Unlabeled glucose and fatty acids produce cold AcAc because of the reversal of the reaction catalyzed by 3-oxoacid-CoA transferase. This results in the decrease of the specific activity of plasma ketone bodies. This dilution is caused only by labeling exchange via reversal of 3-oxoacid-CoA transferase in extrahepatic tissues and not by net ketogenesis. This process is called pseudoketogenesis because it results from an isotopic exchange (see figure 1.4). The minimal pseudoketogenesis ranges from 19-32% of the uptake of ketone body metabolism in heart (163). Pseudoketogenesis occurrs in the isolated working rat heart (164) and in the hepatectomized dog (163). 27 Figure 1.4: Pseudoketogensis in extrahepatic tissues. Modified from Des Rosiers et al (165). Am J Physiol 258: E519-E528, 1990. (1) 3-oxoacid-CoA transferase; (2) acetoactyl-CoA thiolase; (3) 3-hydroxybutyrate dehydrogenase. 28 CHAPTER 2: ANAPLEROSIS 2.1 Overview Anaplerosis is a process that refills the catalytic intermediates of the CAC. The CAC involves eight reactions which oxidize acetyl groups to carbon dioxide and regenerate the acceptor of the acetyl groups. The total pool size of the eight intermediates is small and the individual intermediates have very different sizes (See Figure 2.1) (166). The moderate leakage of intermediates through the mitochondrial membrane and the cell membrane is a physiological process. The leakage of intermediates from the CAC is called cataplerosis. Anaplerosis and cataplerosis are two reciprocal processes working together to balance the CAC flux and sustain cell homeostasis (167). 2.2 The cataplerosis Cataplerosis is a component of gluconeogenesis and glyceroneogenesis. Cataplerosis via phosphoenolpyruvate carboxykinase (PEPCK) contributes to gluconeogenesis in liver and kidney (167). During starvation, the liver and kidney use PEP for gluconeogenesis. PEP is derived from the CAC intermediate oxalacetate formed by pyruvate carboxylase. In adipose tissue, OAA and PEP are used for glyceroneogenesis (168). In normal healthy subjects, cataplerosis is well balanced by anaplerosis. During metabolic transitions, the CAC intermediate concentrations vary in response to these changes. Afterward, anaplerotic influx be balanced by cataplerotic outflux (169). Some pathological conditions lead to excessive loss of CAC intermediates. One typical example is FOD. Patients with FOD have deficiency of long-chain or very long-chain acyl-CoA dehydrogenase. 29 Figure 2.1: Main anaplerotic processes feeding into citric acid cycle. Modified from Brunengraber H et al .(166): J Inherit Metab Dis (2006) 29: 327-331. 30 This causes the accumulation of toxic long-chain or very long-chain acyl-CoAs. As a result, the mitochondrial membrane is damaged and large amounts of CAC intermediates leak out (63). 2.3 The anaplerosis 2.3.1 The significance of anaplerosis Anaplerosis plays an important role in mammalian tissues. In the brain, transmitter glutamate, γ-aminobutyric acid (GABA) in neurons and glutamine from glia are all derived from α-ketoglutarate. The loss of α-ketoglutarate from the CAC would decrease the energy production by the cells if the cataplerosis was not balanced by anaplerosis (170). The heart is another organ where anaplerosis is especially important. The heart can oxidize almost all energy substrates such as glucose, fatty acids, ketone bodies, acetate and even amino acids under special conditions. This is because the heart needs to work non-stop (171). When rat hearts are perfused only with C4-ketone bodies, heart contraction is severely impaired. The decrease is reversed by addition of an anaplerotic substrate such as pyruvate (172). The most effective anaplerotic substrates for the heart are pyruvate and propionate (173). Anaplerosis contributes to the maintenance of energy production. It also works as a signal to regulate insulin release in pancreatic β-cells. The increase of anaplerosis : cataplerosis ratio in pancreas raises insulin release by insulinoma cells (174). The increased blood glucose leads to the increased CAC intermediates and thus increase β-cell ATP:ADP ratio, which triggers insulin release (175). It has been shown that pyruvate carboxylase activity, an anaplerotic enzyme, tightly coupled 31 with glucose-induced insulin secretion. Anaplerosis is especially important in many pathological conditions related to energy metabolism reviewed below. 2.3.2 Anaplerotic substrates Overview As mentioned before, the loss of CAC intermediates must be replenished via anaplerotic processes. Figure 2.1 demonstrates that three main anaplerotic substrates enter the CAC: pyruvate, glutamine/glutamate and propionyl-CoA. Pyruvate is the most studied anaplerotic substrate. It enters the CAC via OAA or malate formed by pyruvate carboxylase or malic enzyme, respectively. Glutamate and glutamine are the precursors of α-ketoglutarate. They enter the CAC via glutamate dehydrogenase and/or aminotransferases (166). The third important entrance point is via the CAC intermediate succinyl-CoA. PropionylCoA is converted to methylmalonyl-CoA, which is continuously converted to succinyl-CoA. A number of precursors of propionyl-CoA enter the CAC through this pathway, such as odd-chain fatty acids, propionylcarnitine and C5-ketone bodies (166). Pyruvate Two enzymes are responsible for the anaplerosis from pyruvate: pyruvate carboxylase (PC) and malic enzyme. PC was first identified as a gluconeogenic enzyme in liver and kidney in 1959 (176). Later, this enzyme was found in nongluconeogenic tissues such as adipose tissue (177), brain (178) and pancreatic islets (179). PC catalyzes the conversion of pyruvate to oxaloacetate in the mitochondria, and serves as an anaplerotic enzyme. It has been reported that 32 50% of pyruvate is carboxylated to form OAA in the β-cells (180). Pyruvate also enters the CAC as malate via malic enzyme. Inhibition of malic enzyme by hydroxymalonate decreased the incorporation of 14 C from [1-14C]pyruvate into malate and impaired heart contraction (181). Malic enzyme activity increases in hypertrophied rat heart (182). In contrast, PC activity does not change compared to control. This shows that in this model, malic enzyme is more anaplerotic than PC. The physiological concentration of pyruvate is 0.1 mM to 0.2 mM (183). The conversion of pyruvate to OAA is important for cell proliferation and repair (184). High concentrations of pyruvate increased myocardium function in isolated guinea-pigs heart (185). The Infusion of dipyruvyl-acetyl-glyerol for 2 hr in anesthetized pigs decreased the coronary infarct size after temporary coronary clamping (186). In PC knockdown β-cells, the incorporations of 14 C from [U- 14 C]glucose into lipids and the acid pellet were decreased 20 – 30% compared to control cells within 45-min incubation. This is because deficiency of PC reduced the conversion of pyruvate to OAA. Thus less OAA was transported from mitochondria to cytosol for further biosynthesis (180). Isolated rat pancreatic islets perifused with buffer containing phenylacetate, an inhibitor of PC, showed a decrease in insulin secretion. This resulted from the disruption of pyruvate cycling (187). Glutamine/glutamate The glutamate/glutamine couple is an effective anaplerotic system. Glutamate enters the CAC through α-ketoglutarate formed by glutamate dehydrogenase and 33 glutamate aminotransferase. Glutamine is first converted to glutamate via glutaminase and then enters the CAC. The onset of exercise causes the increase of CAC intermediate concentrations up to 4 fold in skeletal muscle (248). This happens mainly via anaplerotic glutamate. Muscle glutamate content decreases about 60% (188) and glutamate provides anaplerotic carbon at the level of αketoglutarate (189). Subjects who ingested glutamine before exercise increased CAC intermediates pool size (190). In contrast, ingestion of ornithine αketoglutarate did not expand the CAC pool size. After ischemia, the perfused working rat heart is rescued by glutamine, but not by glutamate and αketoglutarate. If the exogenous glutamine concentration reaches 2.5 mM, the heart goes to complete post-ischaemic cardiac functional recovery (106). This is because the transport of gluctamine into cells is much efficient than the transport of gluctamate. As a result, glutamine is a better anaplerotic substrate than glutamate in the heart (191). However, it is difficult to evaluate the anaplerotic efficiency of the two substrates by stable isotopic techniques because of their interconversion. Precursors of propionyl-CoA Anaplerotic propionyl-CoA is very effective even at a low concentration. This is because of the irreversible conversion of propionyl-CoA to succinyl-CoA. Oddchain fatty acids, C5-ketone bodies and branched-chain amino acids are all precursors of propionyl-CoA. These anaplerotic substrates enter the CAC via the same pathway. These substrates are metabolized to propionyl-CoA, which is 34 continuously converted to succinyl-CoA (a CAC intermediate) by propionyl-CoA carboxylase, methylmalonyl-CoA racemase and methylmalonyl-CoA mutase. The circulating propionate concentration is only 0.05 mM (192). This low concentration results from the rapid uptake of 99% of the gut propionate by the liver (192). In perfused rat heart, 0 – 2 mM [13C3]propionate increased total heart anaplerosis (192). The only fate of propionate in the perfused heart is anaplerosis. This showed the high efficiency of this anaplerotic substrate. C5ketone bodies are effective anaplerotic substrates in heart, brain and kidney (157). C5-ketone bodies are rapidly metabolized and produce propionyl-CoA. Finally, the oxidation of heptanoate, a medium-chain fatty acid, produces propionyl-CoA as well as acetyl-CoA. The important therapeutic role of triheptanoin will be discussed in section 2.3.4. 2.3.3 The measurement of anaplerosis The contribution of anaplerotic substrates to the CAC intermediates has been calculated by isotopic techniques combined with mass spectrometry and NMR techniques (193). There are two related ways to quantify anaplerosis: relative anaplerosis and absolute anaplerosis. Relative anaplerosis Relative anaplerosis represents the contribution of anaplerotic substrates to the turnover of CAC intermediates. It is calculated by two ways: (i) the ratio of labeling of a CAC intermediate versus the labeling of the anaplerotic substrate, or (ii) the uptake of anaplerotic substrate divided by the rate of CAC flux, which is related to oxygen comsumption (194). When [13C3]propionate is infused in 35 anesthetized pigs for 1 hr, the heart anaplerotic flux ratio is 8.9 % calculated by the enrichment ratio (M3 succinate) / ( M3 proionate) (194). The use of the M3 isotopomer is because M3 succinate derives only from M3 propionate. When Kasumov et al. (192) perfused rat hearts with [3-13C]propionate instead of [13C3]propionate, the apparent relative anaplerotic ratio was 3-fold higher in the [3-13C]propionate perfusion ((M1 succinyl-CoA) / (M1 propionyl-CoA)) than that in the [13C3]propionate perfusion ((M3 succinyl-CoA) / (M3 propioyl-CoA)). This overestimation resulted from the contribution of M1 succinyl-CoA via αketoglutarate dehydrogenase. If one used [13C3]pyruvate as the anaplerotic substrate, 13 C labeled citrate shows the highest M3 labeling of CAC intermediates. As a result, the ratio (M3 OAA moiety of citrate) / (M3 pyruvate) is also used to evaluate relative anaplerosis from pyruvate(195). Absolute anaplerosis When the measurement of relative anaplerosis is coupled to the measurement of metabolic CAC activity (oxygen consumption), one calculates absolute anaplerosis expressed as μmol•g-1•min-1 (194). In pigs infused with [13C]pyruvate, the absolute rates of pyruvate carboxylation in the heart is 1.6 μmol•g-1•min-1; this accounts for about 6% of the total turnover of CAC intermediates. 2.3.4 The anaplerotic diet therapy FODs are inherited metabolic disorders associated with energy deprivation. FOD can effect the carnitine cycle as well as the mitochondrial β-oxidation spiral. Patients with FOD often suffer from muscle weakness, hyponia and cardiac problems. Acute stress such as enteritis triggers the sudden shock or death. The 36 most common disorder affects very long-chain acyl-CoA dehydrogenase (63). Since the 1980’s, the classical dietary treatment is to use medium-eventriglycerides (trioctanoin) as part of the energy supply, and to prevent the ingestion of long-chain triglycerides, thus avoiding the accumulation of toxic longchain acyl-CoAs (196). In 2002, Roe et al (106) replaced trioctanoin with oddmedium-chain triheptanoin. As reviewed before, heptanoate, the fatty acid component of triheptanoin, is oxidized to produce acetyl-CoA as well as the anaplerotic and gluconeogenic precursor propionyl-CoA. When the patients’ dietary treatments were switched from octanoin to triheptanoin, there was remarkable improvement in muscle strength, endurance and activity. Pyruvate carboxylase (PC) is a key enzyme of gluconeogenesis in liver and kidney. PC deficiency is a very rare and severe autosomal recessive disease characterized with impaired gluconeogenesis and lactic acidosis (197). A six-dayold girl was diagnosed as biotin-unresponsive pyruvate carboxylase deficiency type B. When she was given triheptanoin from day 7, her major hepatic failure was reversed within 48 hr. At 3 months of age, her psychomotor development, EEG and MRI reached to the normal level. At the age of 6 months, ageappropriate myelination had developed (197). 37 CHAPTER 3: THE SYNTHESES OF ADENINE NUCLEOTIDES, COENZYME A (CoA) AND DEOXYRIBONUCLEIC ACID (DNA) IN RAT LIVER 3.1 Overview of the biosynthesis pathways of adenine nucleotides, CoA and DNA 3.1.1 Overview The biosynthesis pathways of adenine nucleotides, CoA and DNA are interrelated via the synthesis of adenine nucleotides (See figure 3.1). The synthesis of adenine nucleotides involves the de novo synthesis pathway and the purine salvage pathways. The two processes are demonstrated in figure 3.1. Both processes use phosphoribosylpyrophosphate (PRPP) as the key precursor. PRPP is formed via the phosphorylation of ribose-5-phosphate, which is mainly derived from glucose-6-phosphate produced by glycolysis, gluconeogenesis (GNG) and glycogen breakdown. The cycling of pentose groups between RNA, ribose, ribose-1-phosphate and ribose-5-phosphate also partially contributes to the formation of ribose-5-phosphate (198). The synthesis of CoA is related to the adenine nucleotide synthesis pathway via ATP. ATP contributes to the formation of CoA through two ways: phosphorylation of CoA precursors, and the transfer of the adenine-ribose nucleus to dephospho-CoA. The DNA synthesis pathway is shown in figure 3.1. 3.1.2 The biosynthesis pathway of adenine nucleotides The de novo synthesis pathway 38 Figure 3.1: Biosynthesis pathways of adenine nucleotides, CoA and DNA. 39 The purine de novo synthesis pathway appears almost identical in all living organisms. The pathway was discovered by Buchanan et al. in the 1950’s (199). The de novo synthesis pathway begins with non-purine precursors: amino acids, ribose-5-phosphate, carbon dioxide and ammonium. The rate-limiting step is the formation of PRPP by PRPP amidotransferase. After ten sequential steps, inosinate, the first intermediate with a complete purine ring, is formed. The conversion of inosinate to AMP requires aspartate and GTP (200). The incorporation of radioactive glycine into purine is most frequently used to measure the rate of purine de novo synthesis (201). Tullson et al. (202) used [114 C]glycine as a tracer to study the rate of de novo synthesis of adenine nucleotides in isolated rat hindquarters. Rates of de novo synthesis were highest in fast-twitch red muscles (57 nmol / h x g) and lowest in fast-twitch white muscles (26 nmol / h x g). The rate in slow-twitch muscles was between those of the two types of fast-twitch muscles. The de novo synthesis of adenine nucleotides accounts for a small fraction of adenine nucleotide turnover in rat heart (203). The turnover rate of the ATP nucleus is 0.08 nmol / min x g in rat heart (204). This rate increases 10-fold by administration of ribose (205). This is because ribokinase and ribose-phosphate pyrophosphokinase increase the availability of PRPP for adenine nucleotide synthesis. Not all the tissues can synthesize purines de novo. Bone marrow (206), leukocytes (207) and blood cells (208) are not able to synthesize purines de novo. In these cells, the purine salvage pathway is the only source of purines. 40 Abnormal high rates of purine de novo synthesis result in gout. This disease of joints is clinically expressed as acute arthritis. The deposition of crystals of sodium urate in the joints leads to inflammation and pain. The precise cause of gout is still not identified, but it results partly from purine overproduction via the de novo synthesis (209). The purine salvage pathways Compared to the de novo synthesis pathway, the purine salvage pathways are much simpler. The salvage pathways recycle free bases (hypoxanthine, guanine and adenine) and nucleosides (adenosine and guanosine) from nucleic acid breakdown (210). About 90% of free purines are recycled in liver (211). The regulation of this recycling is related to the production of ribose-5-phosphate and PRPP (211). The salvage pathway is also very important for the de novo pathway. This is because four enzymatic steps in the de novo pathway use ATP (211). The purine salvage pathways are especially important for those tissues that are not able to synthesize purines de novo such as bone marrow (206), leukocytes (207) and blood cells (208). The liver is the major organ that salvages purines (212). The salvage pathways also regulate the heart nucleotide pools (210). The rate of purine salvage in heart is evaluated at 0.2 nmol / mg wt x min (213). The most important salvage enzyme is hypoxanthine/guanine phosphoribosyltransferse. The total quantity of purine salvaged by this enzyme was estimated by measuring the amount of uric acid excreted in the urine. A healthy adult on a purine-free diet excretes around 400 mg uric acid per day. This corresponds to 6 mg purine / kg body weight per 41 day (214). A healthy child produces about 10 mg purine / kg body weight per day calculated from the average uric acid excretion (215). The difference in rates of purine synthesis between adults and children shows the high needs of purine for child growth. Lesch-Nyhan syndrome is a disease caused by a defect in purine salvage pathways. This sex-linked recessive disorder results from the lack of hypoxanthine/guanine phosphoribosyltransferase. This enzyme which salvages hypoxanthine is highly expressed in brain (216). This is why patients with LeschNyhan syndrome show major neurological symptoms. 3.1.3 The CoA biosynthesis pathway General CoA synthesis pathway CoA was first discovered by Lipmann in 1946 (217). This heat-stable cofactor was named for its function in acetylation. CoA plays an important role as an acylgroup carrier and carboxyl-activating group in more than 100 biochemical reactions. About 4% of enzymes use CoA as an cofactor (218). The biosynthesis of CoA is a five - step pathway ubiquitous in bacteria, plants and mammals (see figure 3.2). CoA synthesis starts with pantothenate, also called vitamin B5, which cannot be de novo synthesized in mammalian cells. The only source of pantothenate for mammals is the diet (218). Some bacteria can de novo synthesize pantothenate from β-alanine and α-ketoisovalerate (219) . The first and rate-limiting step of CoA synthesis is the phosphorylation of pantothenate to 4’-phosphopantothenate by pantothenate kinase. After 4’-phosphopantothenate reacts with cysteine, a decarboxylation step forms 4’-phosphopantetheine. Next, 42 Figure 3.2: Pathway of Coenzyme A synthesis. Modified from Tahiliani AG et al. (220) J Mol Cell Cardiol 1987 (19): 1161-1167. 43 ATP transfers its AMP moiety to 4’-phosphopantetheine to produce dephosphoCoA, which is finally phosphorylated to CoA by ATP (218). Labeled CoA was synthesized by incubating murine hepatocytes in media containing [13C3,15N1]pantothenate. The cellular uptake of labeled pantothenate from the media initiates the formation of [13C3,15N1]CoA (221). Regulation of CoA contents in tissues CoA is unequally distributed between cell cytosol and mitochondria (220). The cytosolic concentration of CoA is between 0.02 mM to 0.14 mM in animal tissues. Mitochondrial CoA has a much higher concentration ranging from 2 mM to 5 mM (218). The hepatic CoA content changes in response to extracellular signals. Some hormones regulate the CoA contents. In rats fasted for 48 hr, the decrease in insulin and the increase in glucagon raise the total hepatic CoA contents from 544 to 870 nmol / g dry wt (222). The hepatic CoA content in type I diabetic rat liver is twice that of controls, possibly because of the depletion of insulin. Feeding a high fat diet to the rats also increases hepatic CoA content (223). The heart CoA content is lower than that of liver. Myocardial CoA total content (free + esterified) is normally 500 nmol / g dry wt (3). The isolated perfused heart from diabetes rats has high level of total CoA (750 nmol / g dry wt). The addition of insulin to the perfusate significantly decreased the CoA contents to 670 nmol / g dry wt (224). CoA synthesis as an antimicrobial drug target The treatment of infectious diseases faces increasing challenges. The selection of more and more drug-resistant pathogens leads to treatment failure (219). The 44 characteristics of the CoA biosynthesis pathway make it a potential antimicrobial drug target. However, the disruption of genes encoding the enzymes in the pathway of CoA synthesis results in lethal phenotypes (219). The inhibition of the rate-limiting utilization of pantothenate stops CoA synthesis in some microorganisms. Pantothenate analogues have been synthesized as antibacterial and antifungal agents. Pantoyltaurine was the first synthesized pantothenate analogue (225). This sulphonic acid analogue inhibits bacteria growth both in vitro (225) and in vivo (226). Pantoyltaurine works for those bacteria that require exogenous pantothenate. However, it has no effect on bacteria that can synthesize pantothenate de novo. More and more potential inhibitors of pantothenate utilization and biosynthesis have been discovered (for an extensive review, see (219)). 3.1.4 The DNA biosynthesis pathway The true precursors of DNA synthesis are four deoxyribonucleotide-triphosphates (dNTPs). They are dATP, dGTP, dCTP and dTTP (227). The proper synthesis of DNA requires the balanced supply of the four dNTPs in mammalian cells (see figure 3.1). The de novo synthesis pathway The de novo synthesis pathway is irreversible. Four ribonucleotides (ADP, GDP, CDP and TDP) are first synthesized via the nucleotide synthesis pathway. Then three deoxyribonucleotides, i.e. dADP, dCDP and dGDP are formed from ADP, CDP and GDP respectively via ribonucleotide reductase. This enzyme is the first de novo synthetic enzyme that is allosterically regulated. The formation of dTDP , 45 besides the use of ribonucleotide reductase, also uses another allosterically controlled enzyme dCMP deaminase, followed by dTMP synthase and thymidylate synthase (227). The phosphorylation of the four dNDPs by nucleoside diphosphate kinase produces dNTPs for DNA synthesis. The DNA salvage pathway The cell reuses ribonucleosides and deoxyribonucleosides released from the degradation of DNA. This process is called the salvage pathway. This pathway helps to maintain dNTP levels by regulating the flux of ribonucleosides and deoxyribonucleosides to the dNTP pools (227). Significance of the dNTP pools The deoxyribonucleotide-triphosphate pools are small (228). They reach their largest sizes during the S phase of the cell cycle (229). The dGTP pool has the smallest size among the four dNTPs (230). The size of the pool is balanced by DNA synthesis and degradation. Ultraviolet rays (231) and mutagens (232) disturb dNTP pools and thus impair DNA synthesis. The depletion of dNTP pools causes severe consequences. dTTP deprivation, also called thymineless death, first reported in bacteria, is also found in mammalian cells (233). The depletion of dTTP leads to the breakage of DNA strands and to cell death (234). Inherited deficiencies in adenosine deaminase and purine nucleoside phosphorylase lead to accumulation of dATP and dGTP in the immune system. The accumulation of dATP and dGTP interferes with ribonucleotide reductase in lymphocytes and thus causes DNA damage and cell death (235). 3.2 The techniques used for tracing the biosynthesis pathways 46 3.2.1 The techniques used for tracing ATP synthesis from ADP ATP is a main energy source for biological reactions. Thus the measurement of the rate of ATP synthesis (i.e. of ADP phosphorylation) is generally related to the mitochondrial energy generating system. This rate only reflects the oxidative phosphorylation and not the turnover of the adenine-ribose nucleus. The production of ATP and the ratio of [ATP]/[ADP] are the biomarkers to evaluate the mitochondrial energy generating system capacity (236). The dynamic of cellular ATP synthetic activity is quantitatively assessed by luciferin-luciferase reactions (237). The oxidative synthesis of ATP follows fast kinetics evaluated by stop-flow rapid – mixing experiments in rat liver mitochondria (238) . After the supply of oxygen to rat liver mitochondria, the rapid oxidation of NADH via the respiratory chain initiates the synthesis of ATP within 20 ms. This synthetic reaction is half-completed within 100 ms. The liver and brain ATP production in isolated mitochondria of Fisher - 344 rats are not affected by age and caloric restriction (239). The basal rate of ATP synthesis from ADP is 180 μmol / g muscle wt / min in human skeletal muscles (240). In human muscle, the aerobic ATP synthesis rate reaches to the maximum after 9 seconds of maximal exercise. This was evaluated by Walter et al. (241) from the resynthesis rate of phosphocreatine. However, in perfused pig intercostal muscles, anaerobic ATP turnover rate is 6.1 μmol / min•g during the first minute of tonic stimulation of the nerve. In contrast, the anaerobic ATP synthesis rate drops to 0.4 μmol / min•g in unperfused muscles (242). 47 3.2.2 The techniques used for tracing CoA synthesis The methods used to trace CoA synthesis have been developed using labeled or unlabeled synthetic intermediates. [14C]Pantothenate is the most used tracer to evaluate CoA synthesis in vivo and in vitro. Reibel et al. (222) injected [14C]pantothenate into control, fasting and diabetic rats. After 90 min, they measured pantothenate incorporation into CoA from rat organs. Another strategy is to perfuse an isolated organ such as the heart with [14C]pantothenate (243). The calculation of CoA synthesis rate is based on two parameters measured by liquid scintillation counting: (i) the amount of [14C]pantothenate incorporated into CoA, and (ii) the average tissue [14C]pantothenate specific activity (244). Isolated control hearts show high CoA synthesis rates measured with [14C]pantothenate. The addition of exogenous energy substrates (such as glucose and fatty acids) to the perfusate decreases CoA synthesis (245). The incorporation of [14C]pantothenate into CoA is almost undetectable in the perfused heart from type I diabetics rats (246). 4’-Phosphopantetheine is another CoA precursor used to evaluate the CoA synthesis rate in subcellular preparations. Tahiliani et al. (220) incubated isolated mitochondria from rat hearts with 4’-phosphopantetheine in buffer containing ATP. The apparent Vmax for the CoA synthesis was 0.02 nmol / mg protein x min. The increase of pH from 7.4 to 8.5 causes an increase in synthesis. 3.2.3 The techniques used for tracing DNA synthesis Classical techniques for tracing the rate of DNA synthesis use thymidine analogs (247). Thymidine analogs become incorporated into DNA during the cell division, 48 and have been used to measure cell proliferation rates. Two commonly used thymidine analogs are [3H]thymidine and bromodeoxyuridine (BrdU: 5-bromo-2’deoxyuridine). [3H]Thymidine incorporated into DNA strand is detected by autoradiographic techniques (248). This process normally takes several weeks of contact with the film. BrdU is a halopyrimidine. The incorporation of BrdU into DNA is detected by immunohistochemistry using a monoclonal antibody against a DNA strand containing BrdU (249). BrdU is delivered to an animal by intraperitoneal or intravenous injection (247). Multiple injections are required to label the total proliferating population of cells over several days or weeks. The i.p. dose used for the measurement of rodent adult neurogenesis is 50 – 100 mg/kg; 200 mg/kg is the maximal dose. The animal is sacrificed 1-3 hr after injection of BrdU (247). A high dose of BrdU triggers neurocyte death (250). Compared to [3H]thymidine, the BrdU technique is faster and nonradioactive. However, both precursors are toxic and mutagenic. They impair cell division and kill susceptible cells (251; 252). The addition of a bromine atom into the DNA molecule changes the stability of DNA-double strands resulting in chain breakage and mutations. As a result, these techniques cannot be safely used in humans. [2H]Water has been extensively used to trace DNA synthesis. This will be reviewed in section 3.3. 3.3 Tracing the syntheses of biopolymers with [2H]water 3.3.1 Overview Since Von Hevest (253) first used a radioactive isotope for biological investigation in 1926, more and more isotopes of C, H, N and O have been used 49 in metabolic studies. In the 1930’s, deuterium was discovered and began to be used to study metabolic processes (253). Stable isotopes do not decay and can be used for tracing organic syntheses and metabolic processes. Over the past 30 years, the use of stable isotopes has extensively increased, driven by safety concerns and the development of mass spectrometric and NMR techniques (254). 3.3.2 Principle of the use of [2H]water to trace the biosyntheses of (pseudo)biopolymers Overview Biopolymers refer to compounds made of repeated building blocks. Pseudobiopolymers refer to compounds made of different building blocks. Fatty acids, proteins and DNA are all considered as polymers. CoA and adenine nucleotides are pseudo-biopolymers. The general principle of using [2H]water to evaluate the syntheses of biopolymers is based on the incorporation of 2H from [2H]water into the building blocks of biopolymers (254). During the synthesis of many biopolymers, a number of H atoms in C-H bonds are derived from H2O. If water is enriched with 2 H, the building blocks become 2 H-labeled before they are incorporated into biopolymers. When the polymer is synthesized, the labeled building blocks are assembled. The 2 H-enrichment of the building blocks, measured by mass spectrometry, reflects the rate of biosynthesis of the polymer. One assumption, proved by many experiments, is that once the polymer is assembled, the labeling of the building blocks does not change (no new labeling 50 into the block; no loss of label from the block) (255). For an extensive review, see (256). Mechanism of incorporation of [2H]water into building blocks of biopolymers The incorporation of [2H]water into building blocks of molecules occurs through different mechanisms: hydration of double bonds (257), reduction of carbonyl groups by NADH + H+ (258; 259), reduction of double bonds by NADPH + H+, isotopic exchanges (260) (keto-enol tautomerism, reversible transaminations and direct exchange C-H for C-2H) and splitting of C-C bond (261). Hydration of double bonds Water participates in biological reactions. When an enzyme catalyzes the reaction of water with biomolecules containing double bonds, those molecules are hydrated and form new C-H bonds. The hydrogen in the new C-H bonds derives from water. When body water is 2 H-enriched, those biomolecules become 2H-enriched because of the formation of C-2H bonds. In the CAC, the conversion of cis-aconitate to isocitrate, and the conversion of fumarate to malate introduce water into the products (257). Reduction of carbonyl groups by NADH + H+ The NAD+ / NADH + H+ couple works as hydride-accepting and hydride-donating (262). NAD+ dehydrogenases catalyze the interconversion of the members of the redox couples. The two hydrogen atoms (position A and position B) on C-4 of NADH are not equal. Two classes of NAD+ dehydrogenases are responsible for the transfer of one of the two hydrogen atoms on C-4 of NADH to the substrates. 51 There are A-stereospecific and B-stereospecific enzymes. Alcohol dehydrogenase is an A-stereospecific enzyme (258). It transfers the hydrogen at position A from NADH to acetaldehyde. Glyceraldehyde phosphate dehydrogenase is a B-stereospecific enzyme (259). It transfers the hydrogen at position B from NADH to glyceraldehyde 3-phosphate. The NADH-dependent reduction reaction transfers two hydrogen atoms to the product in the form of a hydride ion and a proton. The hydride ion is added directly to the carbonyl group to form new C-H bond. The hydride ion of NADH transferred to the substrate is either non-labeled or 2H-lableled. It depends on the original labeling of the NADH. The proton directly becomes 2H labeled by equilibrium with [2H]water solvent. The 2H+ only forms labile O-2H bond. Reduction of double bonds by NADPH + H+ Like NAD+ dehydrogenases, NADP+ dehydrogenases also include A-specific and B-specific enzymes. NADPH + H+ is generated in the conversion of glucose-6phosphate into ribulose-5-phosphate (263). The oxidation of malate to pyruvate by malic enzyme also produces NADPH + H+. NADPH + H+ are used as the reduced agents in biosynthetic reactions. In the fatty acid synthesis process, NADPH transfers the hydrogen to the double bonds of the synthetic intermediates and forms the saturated C-H bonds. If NADPH is 2H-labeled, the newly synthesized fatty acids become 2H-labeled. Isotopic exchanges Isotopic exchanges occur during the incorporation of 2H into the molecules. A typical isotopic exchange is via keto-enol tautomerism. This refers to a chemical 52 equilibrium between a keto and an enol group. The interconversion of the two forms introduces 2H on C-H bonds adjacent to the carbonyl group. Another isotopic exchange is via some reversible transaminations. The isotopic equilibrium between alanine and pyruvate derives from transamination (260). Alanine is 2H labeled very fast by transamination in the presence of [2H]water. Pyruvate becomes 2H-labeled via alanine transamination. Splitting of C-C bonds The split of C-C bonds introduces hydrogen from the water solvent. A typical example is the aldol cleavage. The splitting of fructose 1,6 – bisphosphate into glyceraldehyde 3 – phosphate and dihydroxyacetone phosphate is catalyzed by aldolase. The new C-H bonds are formed in the two three carbon compounds. If the body water is 2H-enriched, then the two products are labeled by [2H]water (261). Another example is the cleavage of citrate to acetyl-CoA and cytosolic oxaloacetate by ATP citrate lyase. One 2H is introduced on C-2 of acetyl-CoA in the presence of [2H]water. 3.3.3 General protocols of application of [2H]water The use of [2H]water to trace the synthesis rate of polymers has been well developed (264-266). The protocols (see figure 3.3) are mature and safe both for rodents and humans. The animals first receive an intraperitoneal injection of normal saline made in 100% 2H-enriched water. The calculation of the injected amount is based on the body weight, body water content and the target of body water 2H-enrichment (body water 2H-enriched up to 5% for the rodents). Then the animal is provided 2H-enriched drinking water to compensate for the production 53 of unlabeled water from the oxidation of nutrients (267). Human subjects, normally ingest 2H2O in amounts calculated to enrich body fluid at expecting body water 2H- enrichment (up to 2%) (268). Then they drink some [2H]water daily for the duration of the experiments. The 2H-enrichment of body water is assyed by (i) isotope ratio mass spectrometry after reduction of water to H2, and a (ii) by GCMS of acetone after equilibration with water at high pH (268). 3.3.4 The pros and cons of using heavy water [2H]Water is one of the mostly used tools to measure the turnover rate of biomolecules in vivo. [2H]Water is a relatively inexpensive tracer. Compared to tritiated water, [2H]water is non toxic at low enrichment range. For humans, the safe enrichment ranges from 0.5% up to 2% (268); for rats, this working enrichment is up to 5%. As a result, [2H]water can be safely administrated to humans over long periods. The oral administration of [2H]water instead of intravenous infusion makes taking [2H]water an easy process. When [2H]water enters the body, it equilibrates rapidly with total body water. As a result, a homogenously labeled precursor pool is formed. The newly synthesized products contain deuterium in proportion to the enrichment of body water. This makes [2H]water a good tracer because of the stably-labeled homogenous water pool. Another significant advantage is that when using the heavy water method, one can simultaneously trace several different biosynthetic reactions (fatty acid synthesis, cholesterol synthesis, gluconeogenesis and DNA synthesis ) (254). 54 Figure 3.3: Protocol for using [2H]water to trace the rates of synthesis and degradation of biopolymers in vivo. Modified from Dufner D. et al. (254) Curr Opin Clin Nutr Metab Care 6: 511-517. 55 A potential problem is that deuterium has a relatively long biological half-life (2 days in rats, 15 days in humans). So if one tries to measure the degradation of biopolymers via the decay of deuterium, the biopolymers should have longer half life than body water. 3.3.5 Tracing the syntheses of biopolymers Lipid (Fatty acids) biosynthesis [2H]Water is used to measure lipid synthesis via two ways. Schoenheimer et al. (269) used [2H]water to synthesize lipids in some mice, and fed these 2H-labeled lipids to other mice. Then they measured the conversion of labeled lipids to different products. The rate of lipid turnover is calculated from the incorporation of 2H from 2H-enriched body water into the lipids. To prove that the incorporation only derives from the new synthesis, Hutman et al. (270) incubated adipose tissue from rats fasted for 3 days (depletion of glycogens) with tritiated water. This is a condition that should not have fatty acid synthesis. They found no labeling incorporation into fatty acids as expected. The labeling of fatty acids does not occur by isotopic exchange between water and C-H bonds of fatty acids. Lipid synthesis is evaluated either by the numbers of incorporated 2H or as fractional biosynthesis. The fractional biosynthesis is expressed as follows: (2Henrichment in the lipid) / (theoretical 2H-enrichment in the lipids). The maximum number of 2H atoms incorporated per molecule (N) is calculated based on a simple binomial distribution. The theoretical 2H enrichment is N x p, p is 2Henrichment in body water (271). 56 Jungas (272) quantified the total rate of fatty acid synthesis in incubations of rat adipose tissue. The incorporation of 2H from [2H]water into fatty acids confirmed that 23 of the hydrogen atoms of the palmitate were derived from 2H2O water. Wadke et al. (273) found that in rat liver perfused with 100% 2H2O, the number of deuterium atoms incorporated in [2H]water is 22 and 24 per molecule of newly synthesized palmitate and stearate, respectively. More recently, Lee et al. (271) measured the rates of fatty acid and cholesterol synthesis in rat liver and nervous tissues by using [2H]water. They found that the maximum total incorporation of 2H into liver palmitate, stearate and cholesterol is 22, 24 and 30, respectively. The lipids in the nervous system had lower labeling than in the liver. This shows that the rate of lipid synthesis varies between tissues. The [2H]water has also been safely used to evaluate human lipogenesis. When subjects ingested [2H]water, the 2H-enrichment of palmitate of plasma triglycerides (TG) plateaued at 0.6% under the condition of 0.3% 2H-enrichment of body water. The newly synthesized TG contributed about 8% to the plasma TG pools (274). Protein biosynthesis In 1941, Ussing (275) proposed the use of [2H]water to measure protein turnover in vivo. He proposed that free amino acids become 2H-labeled at α carbon via transamination. Free nonessential amino acids equilibrate quickly with 2H-labeled body water via intermediary metabolic pathways before they are incorporated into newly synthesized proteins. Once the protein is assembled, 2H is not able to enter the amino acid residues in the protein backbones. The measurement of the labeling of protein-bound amino acids yields the evaluation of protein turnover. 57 In 2004, Previs et al. (265) first practically used [2H]water to measure the rates of protein synthesis in humans. They chose alanine as the precursor of protein synthesis. Alanine turns over rapidly in vivo. The labeling of the α-hydrogens of alanine equilibrates quickly with body water. As a result, the rate of protein synthesis is determined by measuring the incorporation of 2H-labeled alanine into proteins. The general calculation of protein synthesis rate is: (2H-labeled proteinderived alanine (%)) / (2H-labeled-body water (%)) x 3.7 x time(h)). On average, 3.7 out of 4 carbon-bound hydrogens of alanine exchange with body water (255). Previs et al. (276) studied the influence of feeding on protein synthesis. They found that about 50% of the plasma albumin had been synthesized within 5 hr after feeding in rats. There was no change in the rates of cardiac protein synthesis between acute fasting or chronic food restriction. However, the protein synthesis rate decreases in the liver and skeletal muscle in response to the change of nutritional state. Hellerstein’s group also used glycine or glutamine labeled from [2H]water to quantify protein synthesis (268). DNA biosynthesis Overview Cell division and death are basic physiological processes. Cell division, defined by DNA replication, occurs during the S-phase of the cell cycle. In the presence of [2H]water, 2H is incorporated in DNA strands. The labeled DNA strands are distributed equally in daughter cells. The labeling of DNA strands reflects the fraction of newly synthesized cells formed via cell division. Deoxyribonucleotidetriphosphates are the immediate precursors of DNA synthesis. The deoxyribose 58 (dR) moiety of dNTPs becomes labeled by 2H from [2H]water via the de novo nucleotide synthesis pathway (266). The C-2H bonds in the dR moiety are very stable: there is no loss of labeling under physiological conditions. Not all the carbon bonds of the dR moiety of DNA become 2H- labeled. Mass spectrometry data show that up to six out of seven hydrogen atoms are labeled in the presence of [2H]water. The M1 dR labeling is a nearly linear sum of the 2Henrichment of each C-H bonds. The labeling of dR, isolated from DNA, is measured by GC-MS using different derivatives (277; 278). Calculation of the rate of DNA turnover The rate of DNA turnover is normally expressed as a fractional synthesis rate based on the precursor – product relationship. There are two ways to calculate fractional synthesis. If a fully turned-over tissue is available as the reference for comparison, the calculation of fractional rate is expressed as (dR enrichment of sample cell) / (dR enrichment of fully turned-over cells). In the rat, bone marrow cells turn over very fast and are used as reference cells (256) In humans, blood monocytes and granulocytes are normally chosen as reference cells (256).However, reference cells are not available in many cases. Hellerstein et al. (256) calculated the maximal dR labeling based on 2H-enrichment in body water. This value is used to substitute for that of fully turned-over cells. Thus the fractional synthesis is expressed as (dR enrichment of sample cells) / (maximal dR enrichment) when fully turned-over cells are not available. The application of [2H]water in normal and cancer cells 59 The [2H]water method is suitable for the measurement of the rate of DNA synthesis both in slow turning-over cells and in fast turning-over cells. Human monocytes and granulocytes turn over very fast: more than 20% of cells turn over within one day (266). Rodents’ colonocytes are fully turned over after two days as shown by 2H incorporation (279). In contrast, normal rat colon epithelial cells, mouse mammary epithelial cells and vascular smooth muscle cells have very slow turnover rates (266). Less than 3% of these cells turn over in one day. Cell proliferation is the driving force of carcinogenesis and a prognostic biomarker for cancer progression (280). Hellerstein’s group used [2H]water to trace the synthesis rate of different cell types. When rats were given dietary cholic acid, a cancer promoter, the DNA synthesis rates of colon epithelial cells showed dose-dependent increases in the colonic crypts. The fractional synthesis rate of DNA in the proliferative zone of the crypts increased from 44 % to 69% in proportion to the dietary cholic acid content of the diet. The injection of the carcinogen azoxymethane to rats increased DNA synthesis and the proliferation of colon epithelial cells in all fractions of the crypts (281). [2H]Water also allows to trace tumor cells over time. Breast tissue biopsies from women who have breast cancer and undergo mastectomy show that 2H-labeled breast epithelial cells remain in proliferation process after the cell apoptotic peak has occurred (282). To examine the proliferation kinetics of endothelial cells and tumor cells in the growing prostate cancer, Kim et al. (283) injected prostate cancer cell, PC-3 cells, into mice and used [2H]water to trace the proliferation of endothelial cells and tumor cells for up to six weeks. The data showed that an increase in 60 endothelial cell proliferation precedes that of the tumor cells in the early phase of tumor growth. This confirmed that the increase in endothelial cells corresponds to the growth of tumor cells (283). 61 CHAPTER 4: RESEARCH PROPOSAL 4.1 Project I: C4- and C5-ketogenesis in rat liver Overview Compared with the extensive investigation of C4-ketone body regulation, there is little information available on C5-ketone body metabolism. C5-ketone bodies refer to β-hydroxypentanoate (BHP) and β-ketopentanoate (BKP). Their clinical names are 3-hydroxyvalerate and 3-ketovalerate (113). C5-ketone bodies are derived from the partial oxidation of odd-chain fatty acids. Body fluids contain only traces of C5-ketone bodies because odd-chain fatty acids are absent from the diet of non-ruminant mammals. C5-ketone bodies are found in body fluids of patients with disorders of the anaplerotic pathway, propionyl-CoA → methylmalonyl-CoA → succinyl-CoA, such as deficiency in propionyl-CoA carboxylase and methylmalonyl-CoA mutase as well as biotin or vitamin B12 deficiency (105; 113; 114). Peripheral tissues can use C5-ketone bodies as energy substrates (104). My initial interest in C5-ketone body metabolism arose from an ongoing clinical trial of dietary triheptanoin for the treatment of patients who have long-chain fatty acids disorders (FOD) (106). Patients with FOD suffer from muscle weakness and rhabdomyolysis. The accumulation of long-chain acyl-CoAs and long-chain acyl-carnitines damages mitochondria and cell membranes. This leads to pathological leakage of CAC intermediates which carry acetyl groups as they are oxidized. As a consequence, the citric acid cycle does not operate optimally. The classical treatment for FOD uses the even-chain triglyceride (284). The catabolism of octanoate yields C4-ketone bodies in liver and provides the patients 62 with substitute substrates. However, the loss of CAC intermediates cannot be compensated via trioctanoin treatment. It was hypothesized that boosting anaplerosis would compensate for chronic cataplerosis and improve heart and muscle function. Since 2002, some patients with FOD are treated with dietary triheptanoin instead of trioctanoin (106). The catabolism of heptanoate produces anaplerotic propionyl-CoA and C5-ketone bodies. In peripherial tissues, C5ketone bodies are converted to propionyl-CoA, which is used for anaplerosis. The marked improvement of the patients’ conditions after switching from a trioctanoin- to a triheptanoin-based diet supports the hypothesis. Patients with FOD who ingest dietary triheptanoin accumulate both C4- and C5ketone bodies in their plasma. This suggested that acetyl-CoA groups derived from heptanoate can be used for the synthesis of C4-and C5-ketone bodies. Based on the above considerations, this project aims to investigate the following questions: 1) What is the mechanism of regulation of C5-ketogenesis in the perfused rat liver? Does the regulation reflect the metabolism of C5-ketone bodies in vivo? 2) Why do the patients with deficiency in propionyl-CoA carboxylase and methylmalonyl-CoA accumulate only low level of C5-ketone bodies? 3) What are the interrelations between C4- and C5-ketogenesis in rat livers perfused with octanoate and/or heptanoate? 4) What are the fates of acetyl groups of both fatty acids and of the propionylCoA moiety of heptanoate? 63 5) Does 3-Hydroxyl-3-ethylglutaryl-CoA (HEG-CoA) replace 3-Hydroxyl-3methylglutaryl-CoA (HMG-CoA) when C5-ketone boides are formed? In order to answer the above questions, my experimental strategies are designed with two types of perfusion experiments: i) perfuse single fatty acid alone, and ii) perfuse two fatty acids together. Experimental procedures Rat livers will be perfused with 4 mM glucose and i) increasing concentrations (0 to 1 mM) of [13C3]propionate, [1-13C]octanoate, [8-13C]octanoate or [5,6,713 C3]heptanoate, or ii) 1mM octanoate ([1-13C]octanoate or [8-13C]octanoate) + 0 – 1 mM heptanoate ( or vice versa) with different labeling patterns ([113 C3]heptanoate or [5,6,7-13C3]heptanoate). The concentrations and labeling pattern of C4- and C5-ketone bodies in the effluent perfusate will be assayed as their tert-butyldimethylsilyl derivatives by GC-MS. Labeling of glucose will be assayed on the pentaacetate derivative. The assay of the mass isotopomers distribution of acyl-CoA esters from frozen liver powder will be analyzed by liquid chromatography - mass spectrometry. Acyl-CoA esters will be identified and their mass isotopomer distribution will be calculated. Relative rates of anaplerosis from [13C3]propionyl-CoA precursors ([13C3]propionate, [5,6,7-13C3]heptanoate) will be calculated (18) as the ratio (m3 succinyl-CoA) / (m3 propionyl-CoA). In experiments with [1-13C]octanoate or 813 C]octanoate, calculation of the distribution of label between the two acetyl of C4-ketone bodies will be based on the enrichment of the whole BHB molecule and its fragments (164). 64 4.2 Project 2: Tracing the syntheses of adenine nucleotides, CoA and DNA in rat liver Overview [2H]Water has been extensively used to trace the syntheses of fatty acids (269; 272), sterol (264), glucose (285), amino acids, peptides (286), proteins (265) and nucleic acids (266; 287). The initial goal on this project was to measure the rate of CoA turnover by using [2H]water. Because CoA shares the same backbone of adenine-ribose nucleus with adenine nucleotides and DNA, later I expanded the goal of the present study is to sort out the mechanisms by which 2H from the aqueous medium becomes incorporated into C-H bonds during the biosyntheses of adenine nucleotides, CoA and DNA in rat liver. In addition, [13C]-labeled substrates will be used to complement the results from [2H]water. Another goal is to evaluate the kinetics of the sequential steps of tracer incorporation. This involves the interconnections between different pathways. Based on above, the following questions are investigated: 1) What is the labeling pattern of CoA and its fragments? 2) How do adenine nucleotides and DNA become labeled in vivo? 3) How do glycolysis, gluconeogenesis, pentose phosphate pathway and the three targeted pathways, interconnect? 4) Do the purine salvage pathways contribute to the syntheses of adenine nucleotides, CoA and DNA? Based on above questions, the following experiments are designed: 65 In vivo experiments: rats will receive an introperitoneal injection of normal saline made up in 100% 2H2O in amounts calculated to achieve a 2.5% 2H-enrichment of body water, assuming that total body water accounts for 66% of body weight. The rats will be provided 3.25% 2H-enriched drinking water to compensate for the producton of unlabeled water from the oxidation of foodstuffs and endogenous substrates (271). At different time (2h to 31 days) the rats will be anesthetized with isoflurane before freezing a liver lobe and sampling aortic blood. In vitro experiments: isolated rat livers will be perfused with recirculating bicarbonate buffer containing 4% dialyzed, fatty acid-free, bovine serum albumin, 4 mM glucose. In some experiments, (i) unlabeled glucose will be replaced by [13C6]glucose, (ii) 2 mM [13C5]ribose will be added to 4 mM unlabeled glucose, (iii) 4 mM glucose will be added to perfusate made up in 100% 2H2O. Livers will be quick-frozen at 2 h. One-half of the perfusion experiments will be conducted for 2 h. In other experiments, lobes of the livers will be tied off, cut out and quickfrozen at 30, 60, 90 and 120 min. The concentration and mass isotopmer distribution of glucose will be assayed by GC-MS of the permethyl and the pentaacetate derivatives, respectively. Lactate, formate and dR moiety of DNA of MID will be assayed as the pentaflurobenzyl derivative. 2H-enriched water will be assayed after equilibration with acetone in alkaline medium. LC-MS analysis will be used to assay the MID of CoA, glucose6-phosphate, ribose-5-phosphate, ATP, ADP, AMP, PEP and 3-phosphoglycerate. 66 4.3 Publications 4.3.1 Deng S., Zhang G.F, Kasumove T., Roe C.R., and Brunengraber H. Interrelations between C4-ketogenesis, C5-ketogenesis, and anaplerosis in the perfused rat liver. J Biol Chem 284: 27799-27807, 2009. 4.3.2 Deng S., Zhang G.F., Kombu R.S. Harris S.R. DeSantis D., Vasquez E.J., Puchowicz M.A., Anderson V.E., Brunengraber H. Tracing the syntheses of adenine nucleotides, CoA and DNA in rat liver. To be submitted to J Biol Chem. 67 This research was originally published in The Journal of Biological Chemistry. Interrelations between C4-ketogenesis, C5-ketogenesis, and Anaplerosis in the Perfused Rat Liver. The Journal of Biological Chemistry. 2009; (284): 2779927807. © The American Society for Biochemistry and Molecular Biology. 68 4.3.1 INTERRELATIONS BETWEEN C4-KETOGENESIS, C5-KETOGENESIS AND ANAPLEROSIS IN THE PERFUSED RAT LIVER Shuang Deng1, Guo-Fang Zhang1, Takhar Kasumov1, Charles R. Roe2, and Henri Brunengraber1 From the Department of Nutrition1, Case Western Reserve University, Cleveland OH 44106, and Institute of Metabolic Disease2, Baylor University Medical Center, Dallas TX 75226 Running Title: C4- and C5-ketogenesis in liver Address correspondence to: Henri Brunengraber, Department of Nutrition, Case Western Reserve Univ., School of Medicine, WG 48, 10900 Euclid Ave., Cleveland,OH,44106-4954. Tel.: 216. 368.6548; Fax: 216.368.6560; E-mail: [email protected] Abstract We investigated the interrelations between C4-ketogenesis (production of βhydroxybutyrate + acetoacetate), C5-ketogenesis (production of β- hydroxypentanoate + β-ketopentanoate) and anaplerosis in isolated rat livers perfused with 13 C-labeled octanoate, heptanoate or propionate. Mass isotopomer analysis of C4- and C5-ketone bodies and of related acyl-CoA esters reveal that C4- and C5-ketogenesis share the same pool of acetyl-CoA. Although the uptake of octanoate and heptanoate by the liver are similar, the rate of C5- 69 ketogenesis from heptanoate is much lower than the rate of C4-ketogenesis from octanoate. This results from the disposal of the propionyl moiety of heptanoate by anaplerosis of the citric acid cycle. C5-ketogenesis from propionate is virtually nil because acetoacyl-CoA thiolase does not favor the formation of βketopentanoyl-CoA from propionyl-CoA and acetyl-CoA. Anaplerosis and gluconeogenesis from heptanoate are inhibited by octanoate by competition. The data have implications for the design of diets for the treatment of long-chain fatty acid oxidation disorders, such as the triheptanoin-based diet. Introduction The regulation of the metabolism of C4-ketone bodies, i.e., β-hydroxybutyrate (BHB) and acetoacetate (AcAc) has been extensively investigated in vivo, in isolated livers, hepatocytes and subcellular preparations (for reviews, see (1-4)). In contrast, very little information is available on the metabolism of C5-ketone bodies, i.e., β-hydroxypentanoate (BHP) and β-ketopentanoate (BKP), which are known in the clinical literature as 3-hydroxyvalerate and 3-ketovalerate (5,6). The C5-ketone bodies are formed in liver from the partial oxidation of odd-chain fatty acids (Fig 4.1, central column). C5-Ketogenesis uses the same enzymes of the 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) cycle as C4-ketogenesis. The counterpart of HMG-CoA in C5-ketogenesis is 3-hydroxy-3-ethylglutaryl-CoA (HEG-CoA). We only found one report on the formation of [14C]HEG-CoA in liver extract incubated with propionyl-CoA and [1-14C]acetyl-CoA (7). Because odd-chain fatty acids are absent from the diet of non-ruminant mammals, body fluids contain only traces of C5-ketone bodies. However, C5- 70 ketone bodies and hydroxyethylglutarate are found in body fluids of patients with disorders of the anaplerotic pathway: propionyl-CoA ➔ methylmalonyl-CoA ➔ succinyl-CoA, such as deficiency in propionyl-CoA carboxylase, methylmalonylCoA mutase, as well as biotin or vitamin B12 deficiency (5,6,8). The formation of C5-ketone bodies in these pathological states involves either the conversion of propionyl-CoA to BKP-CoA via 3-ketoacyl-CoA thiolase (Fig 4.1, reaction 1), or the β-oxidation of odd-chain fatty acids synthesized in these patients (9) using propionyl-CoA as a primer (10). Like their C4 counterparts, the C5-ketone bodies are interconverted by mitochondrial BHB dehydrogenase (11). In peripheral tissues, C5-ketone bodies are converted to propionyl-CoA (which is anaplerotic) + acetyl-CoA via 3oxoacid-CoA transferase (12) and 3-ketoacyl-CoA thiolase. Peripheral tissues have a high capacity to utilize exogenous C5-ketone bodies (13), especially heart, kidney and brain which have high activities of 3-oxoacid-CoA transferase (14,15). Our interest in C5-ketone body metabolism arose from an ongoing clinical trial where patients with long-chain fatty acid oxidation disorders are treated with a diet containing triheptanoin (16,17), instead of the classical treatment with the even-chain triglyceride trioctanoin. These patients suffer from muscle weakness and rhabdomyolysis, manifested by the release of creatine kinase in plasma. It was hypothesized that the accumulation of long-chain acyl-CoAs and long-chain acylcarnitines results in membrane damage with release of large and small molecules from cells. The leakage of small molecules would deplete 71 intermediates of the citric acid cycle (CAC) which carry acetyl groups as they are oxidized. It was further hypothesized that boosting anaplerosis with a suitable substrate would compensate for the chronic cataplerosis and improve heart and muscle function. The catabolism of heptanoate yields propionyl-CoA which can be used for anaplerosis in most tissues, and C5-ketone bodies in liver. C5-ketone bodies are converted to propionyl-CoA which can be used for anaplerosis in peripheral tissues. The marked improvement of the patients’ condition after switching from trioctanoin to triheptanoin-based diet supported the hypothesis. After ingestion of meals containing triheptanoin as the only lipid component, both C5-ketone bodies and C4-ketone bodies accumulated in plasma of patients that have been diagnosed with disorders of long-chain fatty acid oxidation (16). This suggested that acetyl groups derived from heptanoate can be used for the synthesis of C4- and C5-ketone bodies. Alternatively, the accumulation of C4ketone bodies after triheptanoin ingestion might result from the inhibition of the utilization of C4-ketone bodies in peripheral tissues by C5-ketone bodies. The aim of the present study was to investigate the interaction between C4- and C5-ketogenesis in rat livers perfused with octanoate and/or heptanoate. To gain insight on the fates of the acetyl groups of both fatty acids, and on the fate of the propionyl-CoA moiety of heptanoate, we conducted the experiments with a series of 13 labeled substrates: [1-13C]octanoate, [8- 13 C]octanoate, [5,6,7- C 3 ]heptanoate, [1- 1 3 C]heptanoate and [ 13 C 3 ]propionate. The outcome of the propionyl-CoA moiety of [5,6,7-13C3]heptanoate and [13C3]propionate was traced by measurements of anaplerosis and glucose labeling by mass 72 isotopomer1 analysis (18). In previous studies on the metabolism of odd-chain fatty acids in liver or hepatocytes (19,20), ketone bodies were assayed with BHB dehydrogenase. This assay does not differentiate C4- from C5-ketone bodies. In the present study, we used gas chromatography-mass spectrometry to specifically assay C4- and C5-ketone bodies (13). EXPERIMENTAL PROCEDURES Materials- General chemicals were purchased from Sigma-Aldrich. [13C3]propionic, [2H5]propionic, [1-13C]octanoic, [8-13C]octanoic, [2H15]octanoic, [2H13]heptanoic, and [5,6,7-13C3]heptanoic acids, 2 H2O (99%), NaO2H, and 13 CO2 gas were obtained from Isotec. [1-13C]Heptanoic acid was prepared by reacting hexylmagnesium bromide with 13 CO2. The purity of the vacuum-distilled product was assessed by GC-MS and NMR. Internal standards of β-hydroxy-[2,2,3,4,4,4-2H6]butyrate and R,S-β-hydroxy-[2,2,3,4,4-2H5]pentanoate were prepared (13,21) by (i) incubating ethyl acetoacetate or ethyl β-ketopentanoate in 2H2O + NaO2H overnight, (ii) reacting with NaB2H4, (iii) acidification to destroy excess NaB2H4, and (iv) neutralization and lyophilization. β-Hydroxypentanoate was prepared by overnight hydrolysis of the ethyl ester with 1.1 equivalents of NaOH, followed by neutralization and lyophilization. Reagents for trimethylsilyl and tert- butyldimethylsilyl derivatization were purchased from Pierce. Liver perfusion experiments- Male Sprague-Dawley rats (130-140g) were fed ad libitum for 8-12 days with standard laboratory chow. Livers from overnight-fasted rats were perfused with non-recirculating bicarbonate buffer (30 ml/min) and 4mM glucose containing 0 to 1 mM of either a single fatty acid ([1- 73 13 C]octanoate, [8-13 C]octanoate, [5,6,7-13C3]heptanoate, [13C3]propionate), or (1mM of octanoate + 0 to 1 mM of heptanoate (or vice versa)) with different labeling patterns. At 14 and 18.5 min, samples of influent and effluent perfusate (collected over 1 min) were treated with NaB2H4 and frozen. This procedure stabilizes the unstable ketoacids by converting them to stable monodeuterated hydroxyacids (13,21). Other samples of perfusate were frozen without treatment. After 20 min, the livers were quick-frozen and kept in liquid nitrogen until analysis. Analytical Procedures In order to assay the uptake of fatty acids and the production of C4- and C5-ketone bodies, 0.1 ml samples of NaB2H4- treated perfusate (influent and effluent) were (i) spiked with internal standards (30 nmol [2H13] heptanoate, 30 nmol [2H15]octanoate, 50 nmol [2H5] propionate, 45 nmol βhydroxy-[2H6]butyrate and 34 nmol β-hydroxy-[2H5]pentanoate), (ii) acidified (to destroy excess NaB2H4), and (iii) deproteinized with 0.7 ml acetonitrile/methanol (7:3). Supernatants from samples from experiments with octanoate and/or heptanoate were dried with N2 and the residue treated to form the trimethylsilyl derivatives of the analytes. Supernatants from samples from experiments with propionate were dried with N2 and the residue treated to form the tertbutyldimethylsilyl derivatives of the analytes. The treatment of the samples with NaB2H4 prevents assaying the individual concentrations of the labeled C4-ketone bodies (BHB and AcAc) and C5-ketone bodies (BHP and BKP), because of overlapping of some mass isotopomers. Therefore the data of this assay yield total concentrations of C4- or C5-ketone bodies (13,21). 74 For the assay of the labeling pattern of individual C4- and C5-ketone bodies, 0.5 ml samples of effluent perfusate (not treated with NaB2H4) were incubated with 50 µmol methoxylamine-HCl (adjusted to pH 9) and incubated at 60°C for 40 min. After acidifying with HCl to pH = 1, the samples were extracted 3 times with 5 ml diethyl ether. The combined extracts were dried with N2, and the residue treated to form the tert-butyldimethylsilyl derivatives of the ketone bodies. GC-MS assay under electron ionization conditions yielded the mass isotopomer distribution of the total C4- and C5-ketone body molecules, and of the fragments corresponding to C-3+4 of C4-ketone bodies, and C-3+4+5 of C5-ketone bodies (13,21). Labeling of glucose was assayed on the penta-acetate derivative. For the assay of the mass isotopomer distribution of acyl-CoA esters, 250 mg of frozen liver powder was extracted with 4 ml of methanol/H2O (1:1) containing 5% acetic acid. After 1 min extraction at 0°C with a Polytron, and centrifugation at 8,000 g for 30 min at 4°C, the supernatant was run through a solid phase extraction ion exchange cartridge packed with 300 mg of 2-2(pyridyl)ethyl silica gel (Sigma-Aldrich). The cartridge was pre-activated with 3 ml of methanol followed by 3 ml of methanol/H2O (1:1) containing 5% acetic acid. After washing the cartridge with 3 ml of methanol/H2O (1:1) containing 5% acetic acid, the acylCoA esters were eluted out by (i) 3 ml of methanol/H2O (1:1) containing 50 mM ammonium formate, (ii) 3 ml methanol/H2O (3:1) containing 50 mM ammonium formate, and (iii) 3 ml methanol. The combined effluent was dried under N2 and the residue stored at -80ºC until LC-MS analysis. 75 LC-MS assays- After dissolving the acyl-CoAs in 100 µl of HPLC buffer A (5% acetonitrile in 100 mM ammonium formate, pH 5.0), 10 µl of solution was injected on a Thermo Electron Hypersil GOLD column (C18, 100 × 2.1 mm, 3 µm particle size) protected by a guard column (Hypersil Gold, C18, 10 × 2.1 mm , 3 µm particle size). Gradient elution at constant flow rate of 0.2 ml/min was: (i) 98% buffer A + 2% buffer B (5 mM ammonium formate in 95% acetonitrile) for 7 min, (ii) from 2% to 60% B from 7 to 25 min, (iii) from 60% to 90% B from 25 to 26 min, (iv) 90% B from 26 to 30 min, and (v) re-equilibration with initial buffer for 9 min before next injection. The order of acyl-CoA elution (min) was malonyl-CoA (2.2), methylmalonyl-CoA (2.7), succinyl-CoA (3.5), HMG-CoA (3.9), acetyl-CoA (6.7), AcAc-CoA (6.9), BHB-CoA (8.1), HEG-CoA (9.1), BKP-CoA (14.0), propionyl-CoA (14.2), BHP-CoA (14.4), pentanoyl-CoA (17.7), hexanoyl-CoA (19.5), heptanoyl-CoA (20.9), octanoyl-CoA (22.2). The liquid chromatograph was coupled to a 4000 QTrap mass spectrometer (Applied Biosystems, Foster City, CA) operated under positive electrospray ionization mode with the following parameters: the source temperature was set at 600ºC with gas 1 and gas 2 at 65 and 55 psi, respectively. The curtain gas was at 30 psi and the collision-activated dissociation gas pressure was held at high. The turbo ion-spray voltage, declustering potential, entrance potential, and collision cell exit potential were 4500, 70, 10, and 50 V, respectively. Multiple reaction monitoring mode was used for quantitation and isotope enrichment analysis. The analyst software (version 1.4.2, Applied Biosystems) was used for data collection and analysis. 76 Calculations- Correction of measured mass isotopomer distributions for natural enrichment was performed using the CORMAT software (22). Relative rates of anaplerosis from [13C3]propionyl-CoA precursors ([13C3]propionate, [5,6,713 C3]heptanoate) were calculated (18) as the ratio (m3 succinyl-CoA)/(m3 propionyl-CoA). These ratios refer to the contribution of the anaplerotic substrates to the catalytic intermediates of the CAC which carry acetyl units as they are oxidized. Note that, when label enters the CAC only via propionyl-CoA, M3 succinyl-CoA is only formed from the sequence: M3 propionyl-CoA ➔ M3 methylmalonyl-CoA ➔ M3 succinyl-CoA. (Recycling of label in the CAC cannot form M3 succinyl-CoA). In experiments with [1-13C]octanoate or [8-13C]octanoate, the distribution of label between the two acetyl of C4-ketone bodies was calculated using (i) the m1 and m2 enrichments of the whole BHB molecule, and (ii) the m1 enrichment of the C3+4 fragment of BHB. The m1 enrichment of the C-1+2 acetyl of BHB was calculated as: m1 of C-1+2 = [(2 m2 + m1) of C-1→4] - (m1 of C-3+4). Data presentation and Statistics- Herein, we present data from ∼70 liver perfusion experiments. For each of the conditions chosen, we ran 6 perfusions in the presence of selected unlabeled or 13 C-labeled substrate(s) with the concentration parameters being allowed to vary. The data points shown in the figures represent means of duplicate gas chromatography-mass spectrometry or liquid chromatography-mass spectrometry injections, which differed by < 2%. The statistical differences between some profiles were tested using a paired t test (Graph Pad Prism Software, version 3). 77 RESULTS AND DISCUSSION Relationship between the uptake of C8-, C7-, and C3-fatty acids and the formation of C4- and C5-ketone bodies. Fig 4.2A shows the uptake of octanoate and its conversion to C4-ketone bodies. Because 1 molecule of octanoate can yield up to two molecules of C4-ketone bodies, the yield of C4-ketogenesis from exogenous octanoate ranged from 80 to 90%. This calculation assumes that basal C4-ketogenesis, at zero octanoate concentration, was not inhibited by increasing concentrations of octanoate. Similar data were reported by McGarry and Foster (23). Fig. 4.2B shows the uptake of heptanoate and its conversion to both C5- and C4-ketone bodies. The uptake of heptanoate (Fig. 4.2B) was very similar to the uptake of octanoate (Fig. 4.2A). Because the oxidation of 1 molecule of heptanoate yields 1 molecule of propionyl-CoA and 2 molecules of acetyl-CoA, one calculates that (i) only about 40% of the propionyl moiety of heptanoate was converted to C5-ketone bodies, and (ii) about 75% of the acetyl moiety of heptanoate was converted to C5- and C4-ketone bodies. Thus, as outlined in Fig. 4.1, acetyl-CoA derived from heptanoate seems to be used to form both C5- and C4-ketone bodies. This will be confirmed by the labeling data presented below. The low yield of conversion of the propionyl moiety of heptanoate to C5-ketone bodies results from its diversion to anaplerosis and gluconeogenesis (Fig. 4.1) as will be shown below. Fig. 4.2C shows the uptake of propionate and the release of C5- and C4-ketone bodies. The yield of C5-ketogenesis from propionate was extremely low (about 0.1%). The much lower yield of C5-ketogenesis from propionate compared to 78 heptanoate (Fig. 4.2B) reflects the properties of 3-ketoacyl-CoA thiolase (Fig. 4.1, reaction 1), which had been described for the interconversion of AcAc-CoA and acetyl-CoA by this enzyme (24-27). Although the thiolase reaction is reversible in vitro, its kinetic properties prevent the formation of AcAc-CoA from acetyl-CoA. This explains why C4-ketogenesis cannot be fueled by acetyl-CoA derived from glucose metabolism. The virtually nil C5-ketogenesis from propionate demonstrates that, in the intact liver, thiolase does not allow the formation of BKP-CoA from propionyl-CoA + acetyl-CoA. In contrast, thiolase allows the cleavage of BKP-CoA derived from heptanoate to propionyl-CoA + acetyl-CoA. Fig. 4.2C also shows that propionate inhibits C4-ketogenesis from endogenous fatty acids, as reported by Brass and Beyerinck (20). To test the interaction between the uptakes of octanoate and heptanoate, as well as the formation of C4- and C5-ketone bodies, we perfused livers with 1 mM of one fatty acid and increasing concentrations of the second fatty acid, and viceversa (Figs. 4.3 and 4.4). Figs. 4.3A and 4.3B show that, starting with similar uptakes of 1 mM octanoate or heptanoate alone, the effects of octanoate on heptanoate metabolism are different from the effects of heptanoate on octanoate metabolism. The competition favors octanoate uptake over heptanoate uptake (Figs. 4.3A and 4.3B; p< 0.05 for both comparisons). Fig. 4.4A shows that, when increasing concentrations of heptanoate are added to a constant 1 mM octanoate, the production of C4-ketone bodies was not inhibited (slope was not significantly different from zero). Also, the production of C5-ketone bodies was much lower than in the presence of heptanoate alone (Fig. 4.2B). Fig. 4.4B 79 shows that, when increasing concentrations of octanoate were added to a constant 1 mM heptanoate, the production of C4-ketone bodies increased markedly, almost as much as in the presence of octanoate alone (Fig. 4.2A). Furthermore, the production of C5-ketone bodies from heptanoate decreased compared to what occurred in the presence of 1 mM heptanoate alone (Fig. 4.2B). Labeling of ketone bodies. Before presenting the labeling pattern of C4- and C5ketone bodies labeled from [13C]octanoate or/and [13C]heptanoate, we want to stress that the interpretation of the data must take into account (i) the concept of zonation of liver metabolism (28), and (ii) the factors that influence the distribution of label between the two acetyl moieties of C4-ketone bodies. First, Fig. 4.5 shows that at low influent concentrations of octanoate (up to 0.2 mM), almost no substrate left the liver in the effluent perfusate. In perfusions with increasing concentrations of heptanoate, the profile of effluent heptanoate concentrations (not shown) was identical to what was measured in perfusions with octanoate. Under these conditions, the pericentral cells of the liver lobule were in contact with much lower octanoate or heptanoate concentrations than the periportal cells. The zonation of propionate concentrations (Fig. 4.5, upper curve) was less pronounced than in perfusions with octanoate, but the profiles were not significantly different. Second, the distribution of label between the two acetyl moieties of C4-ketone bodies depends on whether label enters the HMGCoA cycle as acetyl-CoA or as the C-3+4 moiety of AcAc-CoA (Fig. 4.1). The latter is formed in one of the final steps of fatty acid β-oxidation. Hüth has shown 80 that, in the reversible reaction catalyzed by 3-ketoacyl-CoA thiolase (AcAc-CoA + CoA ↔ 2 acetyl-CoA (Fig. 4.1 (left side), Reaction 1), the C-3+4 moiety of AcAcCoA exchanges much more slowly with the free acetyl-CoA pool than its C-1+2 moiety (25). For livers perfused with increasing concentrations of [1-13C]octanoate or [813 C]octanoate, Figs. 4.6, A and B show the labeling of BHB, its acetyl moieties and of liver acetyl-CoA. We calculated the distribution of label between the two acetyl moieties of C4-ketone bodies from the electron ionization mass spectrum of the TBDMS derivative of BHB, which includes ions corresponding to carbons 1 to 4, and carbons 3 to 4 of BHB (21). The two acetyl moieties of BHB had very different labeling. In the presence of [1-13C]octanoate, most of the label of BHB was on the C-1+2 acetyl, with relatively little label on the C-3+4 acetyl (Fig. 4.6A). The opposite labeling pattern of BHB was observed in perfusions with [813 C]octanoate, where 90% of the BHB labeling was on the C-3+4 acetyl, the labeling of which plateaued at 37%. This results from the fact that the C-3+4 acetyl of BHB derives from the C-7+8 acetyl of octanoate via the C-3+4 acetyl of AcAc-CoA. Because the C-3+4 acetyl of AcAc-CoA exchanges poorly with the free acetyl-CoA pool, the two acetyl moieties of BHB have very unequal labeling. Katz (29) had suggested that the labeling of C-1+2 of BHB could be taken as a proxy, i.e., an indicator, of that of liver mitochondrial acetyl-CoA (29). Fig. 4.6A shows that, in the presence of [1-13C]octanoate, the enrichment of acetyl-CoA plateaued close to 25%, which is the maximal possible enrichment because [113 C]octanoate was labeled on only one acetyl moiety. At high [1-13C]octanoate 81 concentrations, the labeling of acetyl-CoA and of the C-1+2 acetyl of BHB were very close. However, at low [1-13C]octanoate concentrations (0.1 to 0.2 mM), the C-1+2 acetyl of BHB was much more labeled than acetyl-CoA. There are two possible explanations of this discrepancy: metabolic zonation (28) and/or metabolic channeling (166). First, in livers perfused with 0.1 to 0.2 mM [113 C]octanoate, the pericentral cells of the liver lobule were in contact with perfusate containing little or no labeled octanoate, as inferred from the very low concentration of octanoate in the effluent perfusate (Fig. 4.5). In the pericentral cells, acetyl-CoA was unlabeled or minimally labeled. Thus, when acetyl-CoA was assayed in a total liver extract, its enrichment was a composite of labeled periportal and unlabeled pericentral acetyl-CoA. Moreover, because ketogenesis predominates in the periportal cells, there were little unlabeled ketone bodies produced in the pericentral cells, thus little dilution of the ketone bodies in the total liver extract. Second, metabolic channeling transfers labeled acetyl-CoA derived from fatty acid oxidation directly to the HMG-CoA cycle without equilibration with the total pool of mitochondrial acetyl-CoA. We previously showed (31) that, in livers perfused with 0.2 mM [1-13C]octanoate, the labeling of the C1+2 moiety of BHB is greater than that of the acetyl moiety of citrate (a proxy of mitochondrial acetyl-CoA). In the perfusions with [8-13C]octanoate (Fig. 4.6B), the enrichment of the C-1+2 acetyl of BHB was greater than the almost nil enrichment of acetyl-CoA (p = 0.0005). This is a consequence of the poor equilibration of label between [413 C]AcAc-CoA derived from [8-13C]octanoate and free acetyl-CoA via thiolase. 82 Therefore, the labeling of the C1+2 acetyl of BHB cannot, in most case, be used as a proxy of the labeling of mitochondrial acetyl-CoA. C4-ketogenesis and C5-ketogenesis share a pool of acetyl-CoA. The labeling pattern of ketone bodies, HMG-CoA and HEG-CoA show that, when octanoate and heptanoate are used by the liver, acetyl-CoA derived from each substrate is available to both C4- and C5-ketogenesis. Consider the labeling of ketone bodies. First, in liver perfused with [1-13C]heptanoate alone (Fig. 4.7A, left side), BHB was M1 and M2 labeled. Therefore, labeled acetyl-CoA derived from [113 C]heptanoate was incorporated into C4-ketone bodies. As increasing concentrations of unlabeled octanoate were added to 1 mM [1-13C]heptanoate, the M1 and M2 enrichments of BHB decreased, as expected. Second, in livers perfused with 1 mM [5,6,7-13C3]heptanoate alone (left side of Fig. 4.7B), BHP was only M3 labeled, as expected. When increasing concentrations of [1- 13 C]octanoate were added to [5,6,7-13C3]heptanoate, BHP became up to 20% M4 labeled, while M3 labeling decreased from 90% to 70% (Fig. 4.7B). Thus, in this experiment, M4 BHP was formed from a M3 propionyl-CoA derived from [5,6,7- 13C3]heptanoate, and a M1 acetyl-CoA derived from [1-13C]octanoate. However, when increasing concentrations of [8-13C]octanoate were added to 1 mM [5,6,7-13C3]heptanoate (Fig. 4.7C), the M4 labeling of BHP was very low (up to 2%), while the M3 enrichment of BHP barely decreased from 90% (not shown). This is because [8-13C]octanoate does not substantially label acetylCoA, as mentioned above (Fig. 4.6B). Third, in perfusions with constant 1 mM [113 C]octanoate and increasing concentrations of unlabeled heptanoate, M1 BHP 83 did accumulate (Fig. 4.7D). This M1 BHP was formed from unlabeled propionyl (derived from heptanoate), and M1 acetyl-CoA (derived from [1-13C]octanoate). These three set of experiments show that C4- and C5-ketogenesis share the same acetyl-CoA pool (Fig. 4.1). Consider now the labeling patterns of HMG-CoA (Fig. 4.8A) and HEG-CoA (Fig. 8B). In a liver perfused only with [1-13C]heptanoate (Fig. 4.8, A and B, left sides), HMG-CoA was M1, M2, and M3 labeled, while HEG-CoA was M1 and M2 labeled. The M1 and M2 enrichments of HMG-CoA were not significantly different from the corresponding enrichments of HEG-CoA. This also indicates that the syntheses of HMG-CoA and HEG-CoA share the same pool of acetyl-CoA, in this case ([1-13C]acetyl-CoA derived from [1-13C]heptanoate). As increasing concentrations of unlabeled octanoate were added to the 1 mM [113 C]heptanoate, the enrichments of (i) the M1, M2, and M3 isotopomers of HMG- CoA, and (ii) M1 and M2 isotopomers of HEG-CoA decreased. This demonstrates that HMG-CoA synthesis can use acetyl-CoA derived from heptanoate oxidation, and that HEG-CoA synthesis can use acetyl-CoA derived from octanoate oxidation. This does confirm that acetyl-CoA derived from octanoate oxidation was used for C5-ketogenesis. Reversibility of the BHB-CoA dehydrogenase reaction. When [1-13C]octanoate undergoes β-oxidation, carbons 5 to 8 of octanoate (which will go to BHB-CoA and AcAc-CoA) are initially unlabeled. Although as predicted, hexanoyl-CoA and butyryl-CoA were unlabeled (not shown), BHB-CoA and AcAc-CoA were M1 and M2 labeled (Fig. 4.9). The labeling of AcAc-CoA results from the partial isotopic 84 equilibration of AcAc-CoA and acetyl-CoA via 3-ketoacyl-CoA thiolase (Fig. 4.1, Reaction 1). The M1 and M2 labeling of BHB-CoA (Fig. 4.9) shows that the BHB-CoA dehydrogenase reaction is reversible in the intact liver in spite of the high rate of β-oxidation. A similar equilibration occurs in the catabolism of [113 C]heptanoate. In one perfusion with 1 mM [1-13C]heptanoate, although pentanoyl-CoA was unlabeled, BHP-CoA and acetyl-CoA were 12.7% and 40%. M1 labeled, respectively (BKP-CoA was undetectable). Anaplerosis from heptanoate and propionate. Anaplerosis can be expressed as a relative or an absolute flux. Relative anaplerosis is the fractional contribution of an anaplerotic substrate to the fourcarbon component of CAC intermediates which carry acetyl groups as they are oxidized. For example, in Fig 4.10A, [13C3]propionate contributes up to 0.37 of the catalytic intermediates of the CAC. The remaining fraction (1 – 0.37 = 0.63) derives from recycling of catalytic intermediates. Absolute anaplerosis is a flux of an anaplerotic substrate into the CAC, expressed as μmol•(g dry wt)-1•min-1. In experiments with precursors of M3 propionyl-CoA ([5,6,7-13C3]heptanoate and [13C3]propionate), we calculated relative anaplerosis as the m3 enrichment ratio (succinyl-CoA)/(propionyl-CoA) (Fig. 4.10A).This ratio represents the contribution of the propionyl-CoA precursor to CAC catalytic intermediates which carry acetyl units as they are oxidized. Assuming that propionate and heptanoate in the liver are channeled only to anaplerosis and C5-ketogenesis, we calculated absolute anaplerosis from each propionyl-CoA precursor as (uptake of substrate minus C5-ketogenesis)/(fractional anaplerosis from this substrate). This rate, which is 85 up to 15 μmol⋅min−1⋅(g dry wt)−1 for [5,6,7-13C3]heptanoate (Fig. 4.10B), does not represent a flux of acetyl-CoA through the CAC. It does represent the rate of the sections of the CAC going from succinyl-CoA to oxaloacetate, the cataplerotic intermediate leading to PEP and glucose. Relative anaplerosis from [13C3]propionate increased faster with substrate concentration than relative anaplerosis from [5,6,7-13C3]heptanoate. The opposite occurred with absolute anaplerosis (compare Figs. 4.10A and 4.10B). This probably results in a faster CAC flux in the presence of [5,6,7-13C3]heptanoate (which supplies 2 acetyl-CoA) than in the presence of [13C3]propionate (which supplies no acetyl-CoA). Absolute anaplerosis from [5,6,7- 13C3]heptanoate was significantly decreased in the presence of octanoate (p <0.05), although the latter is not anaplerotic (Fig. 4.10B, top vs. bottom curve). This results from the inhibition of heptanoate uptake by octanoate (Figs. 4.2B and 4.3A). Thus, anaplerosis from an odd-chain fatty acid is modulated by the presence of an even-chain fatty acid. If all absolute anaplerosis from [5,6,7-13C3]heptanoate or [13C3]propionate (Fig. 4.10B) were used for gluconeogenesis, one calculates that the glucose in the effluent perfusate should be about 1.4 to 1.7% labeled in M2 + M3 isotopomers. This calculation takes into account the m3 enrichment of succinyl-CoA, the absolute anaplerosis and the supply of unlabeled glucose in the influent perfusate. In fact, glucose labeling from [5,6,7-13C3]heptanoate and [13C3]propionate plateaued at 0.8 to 1%. This dilution (by a factor of about 2) results from isotopic exchanges between CAC intermediates and related compounds, as shown by Hetenyi (32). 86 Quite striking is the absence of labeling of glucose from [5,6,7-13C3]heptanoate in the presence of unlabeled octanoate (Fig. 4.10C, lower curve, ■). This, in spite of the fact that anaplerosis from [5,6,7-13C3]heptanoate was not fully abolished by octanoate (Fig. 4.10B). This inhibition may result from the increase in the [NADH]/[NAD+] ratios induced by the rapid oxidation of octanoate. One can wonder whether zonation of liver metabolism influences calculated rates of relative anaplerosis, especially at low [5,6,7-13C3]heptanoate concentrations, when the pericentral hepatocytes are not in contact with the labeled substrate (Fig. 4.5). The pericentral cells must have pools of unlabeled propionyl-CoA, methylmalonyl-CoA and succinyl-CoA derived from aminoacid catabolism and recycling of succinyl-CoA in the CAC. Hence, in the extract of a whole liver perfused with a low concentration of [5,6,7-13C3]heptanoate, the m3 enrichments of propionyl-CoA and succinyl-CoA formed in periportal cells are diluted by unlabeled substrates formed in the pericentral cells. Moreover, the relative anaplerosis calculated at low [5,6,7-13C3]heptanoate concentration may either be over- or underestimated, depending on the relative sizes and enrichments of the propionyl-CoA and succinyl-CoA pools in the pericentral cells. Concluding remarks. measurements of In the substrate above fluxes investigations, and mass the association isotopomer analysis of of intermediates provides a wealth of information on the interrelation between C4ketogenesis, C5-ketogenesis and anaplerosis. Our data extend to C5-ketogenesis the concept that the mitochondrial 3-ketoacyl-CoA thiolase reaction (Fig. 4.1, Reaction 1) does not allow a net acyl-CoA condensation flux (33). This is shown 87 by the absence of C5-ketogenesis from propionate (Fig. 4.2C), and the absence of C4-ketogenesis from acetate (34) or from glucose. The absence of net acylCoA condensation does not prevent partial isotopic equilibration between acetylCoA and AcAc-CoA, as shown by (i) the incorporation of label from [113 C]octanoate into C4-ketone bodies (Fig. 4.6A), and C5-ketone bodies (in the presence of unlabeled heptanoate, Fig. 4.7D), and (ii) the incorporation of label from [1-14C]acetate into C4-ketone bodies (see Fig. 4.1 of (34)). Also, the absence of net condensation between propionyl-CoA derived from propionate and acetyl-CoA, resulting in only traces of C5-ketone body production (Fig. 4.2C), does not prevent incorporation of label from [13C3]propionate into HEG-CoA which was 90% M3 labeled (not shown). The absence of C5-ketogenesis from propionate or propionyl-CoA strongly suggests that the concentration of C5ketone bodies found in body fluids of patients with disorders of the propionyl-CoA pathway are formed via β-oxidation of odd-long-chain fatty acids synthesized from propionyl-CoA in these patients. This is similar to C5-ketogenesis from heptanoate (Fig. 4.1, middle column). Our data confirm Hüth et al. (25) finding that the rate of equilibration of the C3+4 acetyl moiety of AcAc-CoA with acetyl-CoA via AcAc-CoA thiolase is much smaller than the rate of equilibration of the C1+2 moiety. This is clearly illustrated by the difference in the enrichments of the C1+2 and C3+4 moieties of C4-ketone bodies in the presence of [1-13C]octanoate vs. [8-13C]octanoate (Fig. 4.6). Although the liver takes up octanoate or heptanoate at similar rates (Fig. 4.2, A and B), the flux of C4-ketogenesis is more rapid than that of C5-ketogenesis. This 88 results from the diversion of the propionyl moiety of heptanoate to anaplerosis of the CAC and gluconeogenesis (Figs. 4.1, 10). Also, in the presence of octanoate and heptanoate, the uptake of octanoate and C4-ketogenesis prevails over the uptake of heptanoate and C5-ketogenesis. The inhibition of anaplerosis and gluconeogenesis from heptanoate by octanoate (Fig. 4.10, B and C) has implications for the design of diets, which are both anaplerotic and gluconeogenic, for the treatment of some metabolic diseases such as disorders of long-chain fatty acid oxidation. Physicians may be tempted to progressively modify the patients’ diet to replace medium-even-chain triglycerides (which have been used since the 1980s to treat such patients (35)) by triheptanoin (16,17). This would not be advisable because octanoate inhibits heptanoate uptake (Fig 4.3B), C5-ketogenesis from heptanoate (Fig 4.4B) and anaplerosis from heptanoate (Figs 4.10A, 4.10B). REFERENCES 1. McGarry, J. D. and Foster, D. W. (1980) Annu. Rev. Biochem. 49, 395-420 2. Robinson, A. M. and Williamson, D. H. (1980) Physiol Rev. 60, 143-187 3. Balasse, E. O. and Féry, F. (1989) Diabetes Metab Rev. 5, 247-270 4. Fukao, T., Lopaschuk, G. D., and Mitchell, G. A. (2004) Prostaglandins Leukot. Essent. Fatty Acids 70, 243-251 5. Sweetman, L., Weyler, W., Nyhan, W. L., de Cespedes, C., Loria, A. R., and Estrada, Y. (1978) Biomed. Mass Spectrom. 5, 198-207 6. Kuhara, T., Inoue, Y., Shinka, T., Matsumoto, I., and Matsuo, M. (1983) Biomed. Mass Spectrom. 10, 629-632 7. Baker, F. C. and Schooley, D. A. (1981) Biochim. Biophys. Acta 664, 356372 8. Duran, M., Gompertz, D., Bruinvis, L., Ketting, D., and Wadman, S. K. (1978) Clin. Chim. Acta 82, 93-99 89 9. Hommes, F. A., Kuipers, J. R., Elema, J. D., Jansen, J. F., and Jonxis, J. H. (1968) Pediatr. Res. 2, 519-524 10. Wakil, S. J. (1989) Biochemistry 28, 4523-4530 11. Bergmeyer, H. U., Gawehn, K., Klotzsch, H., Krebs, H. A., and Williamson, D. H. (1967) Biochem. J. 102, 423-431 12. Jencks, W. P. (1973) In Boyer, P. D., editor. The Enzymes, Academic Press, New York 13. Leclerc, J., Des Rosiers C., Montgomery, J. A., Brunet, J., Ste-Marie, L., Reider, M. W., Fernandez, C. A., Powers, L., David, F., and Brunengraber, H. (1995) Am. J. Physiol 268, E446-E452 14. Williamson, D. H., Bates, M. W., Page, M. A., and Krebs, H. A. (1971) Biochem. J. 121, 41-47 15. Fukao, T., Song, X. Q., Mitchell, G. A., Yamaguchi, S., Sukegawa, K., Orii, T., and Kondo, N. (1997) Pediatr. Res. 42, 498-502 16. Roe, C. R., Sweetman, L., Roe, D. S., David, F., and Brunengraber, H. (2002) J. Clin. Invest 110, 259-269 17. Roe, C. R., Yang, B. Z., Brunengraber, H., Roe, D. S., Wallace, M., and Garritson, B. K. (2008) Neurology 71, 260-264 18. Kasumov, T., Cendrowski, A. V., David, F., Jobbins, K. A., Anderson, V. E., and Brunengraber, H. (2007) Arch. Biochem. Biophys. 463, 110-117 19. Krebs, H. A. and Hems, R. (1970) Biochem. J. 119, 525-533 20. Brass, E. P. and Beyerinck, R. A. (1988) Biochem. J. 250, 819-825 21. Des Rosiers C., Montgomery, J. A., Desrochers, S., Garneau, M., David, F., Mamer, O. A., and Brunengraber, H. (1988) Anal. Biochem. 173, 96-105 22. Fernandez, C. A., Des Rosiers, C., Previs, S. F., David, F., and Brunengraber, H. (1996) J. Mass Spectrom. 31, 255-262 23. McGarry, J. D. and Foster, D. W. (1971) J. Biol. Chem. 246, 1149-1159 24. Hüth, W., Dierich, C., von Oeynhausen, V., and Seubert, W. (1974) Biochem. Biophys. Res. Commun. 56, 1069-1077 25. Hüth, W., Dierich, C., von, Oeynhausen, V., and Seubert, W. (1973) Hoppe Seylers. Z. Physiol Chem. 354, 635-649 26. Hüth, W. and Alves, F. (1985) Biochim. Biophys. Acta 830, 274-281 27. Balzer, I. and Hüth, W. (1986) Biochim. Biophys. Acta 870, 350-356 90 28. Jungermann, K. and Kietzmann, T. (1996) Annu. Rev. Nutr. 16, 179-203 29. Katz, J. (1985) Am. J. Physiol 248, R391-R399 30. Srere, P. A. (1987) Annu. Rev. Biochem. 56, 89-124 31. Des Rosiers, C., David, F., Garneau, M., and Brunengraber, H. (1991) J Biol. Chem 266, 1574-1578 32. Hetenyi, G., Jr. (1982) Fed. Proc. 41, 104-109 33. Hüth, W. and Menke, R. (1982) Eur. J. Biochem. 128, 413-419 34. Endemann, G., Goetz, P. G., Tomera, J. F., Rand, W. M., Desrochers, S., and Brunengraber, H. (1987) Biochem Cell Biol. 65, 989-996 35. Bougnères, P. F., Saudubray, J. M., Marsac, C., Bernard, O., Odièvre, M., and Girard, J. (1981) J. Pediatr. 98, 742-746 FOOTNOTES This work was supported by the NIH (Road Map grant 5R33DK070291 and grant 5R01DK069752) and the Cleveland Mt. Sinai Health Care Foundation. 1 Mass isotopomers are designated as M1, M2…Mn, where n is the number of heavy atoms in the molecule. The mol percent enrichment of each isotopomer is designated as m1, m2…mn. The abbreviations used are: AcAc, acetoacetate; BHB, β-hydroxybutyrate; BKP, β-ketopentanoate BHP, (3-ketovalerate); β-hydroxypentanoate (3- hydroxyvalerate); CAC, citric acid cycle; HEG-CoA, β-hydroxy-β-ethylglutarylCoA; HMG-CoA, β-hydroxy-β-methylglutaryl-CoA; enrichment. 91 MPE, molar percent FIGURE LEGENDS Figure 4.1 Scheme of C4-ketogenesis and C5-ketogenesis in the liver. Numbers refer to the following enzymes: 3-ketoacyl-CoA thiolase (1), HMG-CoA synthase (2), HMG-CoA lyase (3), β-hydroxybutyrate dehydrogenase (4). The figure also shows the link between propionyl-CoA and the citric acid cycle (CAC) via anaplerosis. Figure 4.2 Comparison between the uptake of octanoate (A), heptanoate (B), or propionate (C) and the production of C4-ketone bodies (β-hydroxybutyrate + acetoacetate) and C5-ketone bodies (β-hydroxypentanoate + β-ketopentanoate). (fatty acid uptake, ●; C4-ketogenesis, ■; C5-ketogenesis, ▲). A, no C5-ketone bodies were detected in the presence of octanoate. A, B, C, n = 6 at zero concentration of influent fatty acid; n = 1 for the other concentrations. All liver perfusions reported in this manuscript were conducted for 20 min. All rates of substrate uptake and production (Figs 2 to 5) were assayed on samples of influent and effluent perfusate taken at 14 and 18.5 min (collecting the samples over 1 min). All reported values are the means of the 14 and 18.5 min measurements. Figure 4.3 Competition between octanoate and heptanoate for uptake by perfused rat livers. A, constant 1 mM octanoate + increasing heptanoate concentration in influent perfusate. B, constant 1 mM heptanoate + increasing octanoate concentration in influent perfusate. The vertical scale shows the uptake of octanoate (▲) and heptanoate (△). 92 Figure 4.4 Competition between C4-ketogenesis from octanoate and C5ketogenesis from heptanoate in perfused rat livers. A, constant 1 mM octanoate + increasing heptanoate concentration in influent perfusate. B, constant 1 mM heptanoate + increasing octanoate concentration in influent perfusate. The vertical scale shows the production of C4-ketone bodies (▲) and C5-ketone bodies (△). Figure 4.5 Profiles of concentrations of octanoate (●) and propionate (▲) in the effluent perfusate. The data refer to perfusions with increasing concentrations of a single fatty acid, and are plotted as a function of the influent concentration of each fatty acid. The dotted line is the theoretical identity of influent and effluent concentrations. Figure 4.6 Labeling pattern of effluent β-hydroxybutyrate (BHB) and tissue acetyl-CoA from livers perfused with increasing concentrations of [1- 13 C]octanoate (A) or [8-13C]octanoate (B). The figures show the molar percent enrichments (MPE) of the M1 (■) and M2 (□) mass isotopomers of BHB, the MPE of the C-1+2 (▲) and C-3+4 (△) acetyls of BHB, and the MPE of liver acetyl-CoA (●). The labeling patterns of ketone bodies (Figs 6, 7) were assayed in samples of effluent perfusate taken at 14 and 18.5 min (collecting the samples over 1 min). All reported values are the means of the 14 and 18.5 min measurements. Figure 4.7 Sharing of acetyl groups between C4- and C5-ketogenesis reflected by the mass isotopomer distribution of BHB and BHP. A, labeling pattern of BHB in perfusions with constant 1 mM [1-13C]heptanoate + increasing concentrations of unlabeled octanoate. B, labeling pattern of BHP in perfusions with constant 93 [5,6,7-13C3]heptanoate and increasing concentrations of [1-13C]octanoate. C, labeling pattern of BHP in perfusions with constant [5,6,7-13C3]heptanoate and increasing concentrations of [8-13C]octanoate. D, labeling pattern of BHP in perfusions with constant [1-13C]octanoate and increasing concentrations of unlabeled heptanoate. Figure 4.8 Mass isotopomer distribution of HMG-CoA (A) and HEG-CoA (B) in livers perfused with constant 1 mM [1-13C]heptanoate and increasing concentrations of unlabeled octanoate. Figure 4.9 Mass isotopomer distribution of BHB-CoA and AcAc-CoA in livers perfused with increasing concentrations of [1-13C]octanoate. Figure 4.10 Anaplerosis and glucose labeling from increasing concentrations of [13C3]propionate (♦) or [5,6,7-13C3]heptanoate (■,▲). The perfusions with increasing [5,6,7-13C3]heptanoate concentrations were conducted in the absence (▲) or presence (■) of constant 1 mM [1-13C]octanoate. A, relative anaplerosis expressed as the m3 enrichment ratio (succinyl-CoA)/(propionyl-CoA). absolute anaplerosis. C, M2 + M3 labeling of glucose in the effluent perfusate. 94 B, Figure 4.1 95 Figure 4.2 96 Figure 4.3 97 Figure 4.4 98 Figure 4.5 99 Figure 4.6 100 Figure 4.7 101 Figure 4.8 102 Figure 4.9 103 Figure 4.10 104 4.3.2 Tracing the syntheses of adenine nucleotides, CoA and DNA in liver Shuang Deng, Guo-Fang Zhang, Rajan S. Kombu, Stephanie R. Harris, David A. DeSantis, Edwin J. Vasquez, Michelle A. Puchowicz, Vernon E. Anderson, and Henri Brunengraber Depts of Nutrition and Biochemistry, Case Western Reserve University, Cleveland OH 44109 Running title: Syntheses of adenine nucleotides, CoA and DNA in liver Corresponding author: Henri Brunengraber, Department of Nutrition, Case Western Reserve University, 10900 Euclid Ave. WG-48; Cleveland OH 441064954. Tel: (216) 368-6548. Fax: (216) 368-6560. Email: [email protected] 105 Abstract The syntheses of the carbon skeletons of adenine nucleotides and coenzyme A were monitored in livers from overnight-fasted rats perfused with buffer containing either 4 mM [13C6]glucose, 4 mM unlabeled glucose + 2 mM [13C5]ribose, or with buffer made up in 0 to 100% deuterated water and containing 4 mM unlabeled glucose. With all labeled substrates, the mass isotopomer distribution of glucose and glycolytic intermediates reveals intense cycling and redistribution of label through glycolysis, gluconeogenesis, the citric acid cycle and the pentose phosphate pathway. This cycling affects the isotopomer distribution of ribose-5-phosphate, adenine nucleotides and CoA. In the presence of 2H-enriched water, most of the 2H found in adenine nucleotides and CoA is incorporated between ribose-5-P and AMP. Most of the turnover of adenine nucleotides and CoA is supported by salvage pathways. The fractional turnover rates of the adenine moiety of adenine nucleotides and of CoA are 7%/h and 33%/h, respectively. Our findings open the way to studies on the modulation of adenine nucleotides and CoA turnover in physiological and pathological conditions. 106 Introduction 2 H-enriched water has been used to measure the synthesis of biomolecule since the 1930s (1). In the course of biosyntheses, H+ from the aqueous medium become incorporated into C-H bonds by various mechanisms: hydration, reduction (2), splitting of C-C bonds and isotopic exchanges (3). If the aqueous medium is 2H-enriched, the product of the synthesis becomes 2H-enriched in some proportion to the net synthesis of the compound. This technique has been used to trace the syntheses of fatty acids (1,4), sterols (5,6), glucose (7), aminoacids (8), peptides (9,10), proteins (8,11-13) and nucleic acids (14,15). In most cases, it is difficult or impossible to convert the 2H-enrichment of the product into a rate of synthesis expressed in chemical units, e.g., μmol⋅h−1⋅kg−1. This is because it is often impossible to predict the number of 2 H atoms incorporated into a synthesis from the stoichiometry of the reactions of the synthesis. In favorable cases, empirical H/C incorporation ratios can be calculated by comparing the incorporation of labeled H (3H or 2H) and the incorporation of labeled C (14C or 13 C) into the product. For example, the H/C ratios for fatty acid and cholesterol synthesis from glucose were calculated from experiments where the products were synthesized in the presence of 3H- or 2Henriched water and [U-14C]glucose (4,16). The H/C ratios are expected to be different when lipogenesis is fueled from glucose or from acetate (17). In most cases, relative rates of synthesis are calculated by comparing the 2Henrichment of the product at a given time with the 2H-enrichment at infinite time (14,15). This technique has led to many studies on the syntheses of proteins (18) 107 and DNA (19), as well as to studies on the kinetics of cell proliferation in health and disease (14,15,20). The goal of the present study was to sort out some of the mechanisms by which 2 H from the aqueous medium becomes incorporated into C-H bonds during the biosyntheses of adenine nucleotides, CoA and DNA in liver (Fig 4.11). To achieve this goal, we used two experimental models with different labeling dynamics. The first model is the isolated rat liver perfused for 2 h with recirculating buffer enriched with 2H (0 to 100%) (16). To test whether 2H incorporation into adenine nucleotides and CoA reflects net synthesis vs isotopic exchanges, we also perfused rat livers with buffer made up in unlabeled water and containing [13C6]glucose or [13C5]ribose. We view the perfused rat liver as a closed system where the organ is exposed to an initial amount of substrate which is not replenished. This model allows for extensive equilibration of labeling patterns of metabolites. Also, because of the short duration of the experiments, metabolites salvaged from nucleic acids are not labeled. The second model is the live rat the body fluids of which are kept chronically enriched with 2H for up to 30 days. We view the live rat as an open system where unlabeled carbon substrates are constantly supplied by the diet. Although the 2H-enrichment of body fluids of the live rat is kept constant, the supply of carbon substrates prevents building blocks of biopolymers to reach the same degree of labeling as would occur in a closed system. However, because of the long duration of the experiments, metabolites salvaged from nucleic acids can be labeled. In the context of this report, the turnover of adenine nucleotides and CoA is the 108 turnover of the adenosine moiety of these metabolites (synthesized via de novo or/and salvage pathways). Experimental Procedures Materials.Sigma-Aldrich-Isotec supplied most chemicals, enzymes and the following isotopically labeled compounds: 2 H2O (99.8%), [13C6]glucose, [13C5]ribose. Perfused liver experiments. Livers from overnight-fasted male rats (200-250 g) were perfused (21) with recirculating bicarbonate buffer containing 4% dialyzed, fatty acid-free, bovine serum albumin and 4 mM glucose. In some experiments, (i) unlabeled glucose was replaced by [13C6]glucose, (ii) 2 mM [13C5]ribose was added to 4 mM unlabeled glucose, and (iii) 4 mM unlabeled glucose was added to perfusate made up in 100% 2H2O. One-half of the experiments were conducted for 2 h and the livers were quick-frozen. In other experiments, lobes of the livers were tied off, cut out and quick-frozen at 30, 60, 90 and 120 min. To test for interference of high 2H-enrichment of perfusate water, a series of perfusions was conducted with buffer made up in 0 to 100% 2H2O + 4 mM glucose. In vivo experiments. Nineteen rats (200 ± 10 g) received an intraperitoneal injection of normal saline made up in 99% 2H2O in amounts calculated to achieve a 2.5% 2H-enrichment of body water, assuming that total body water accounts for 66% of body weight. 109 The rats were fed regular chow and provided drinking water 3.25% enriched in 2 H to compensate for the production of unlabeled water from the oxidation of foodstuffs and endogenous substrates (6). One control rat was injected with unlabeled saline. At various times after 2H loading (2 h to 31 days) the rats were anesthetized with isoflurane before freezing a liver lobe and sampling aortic blood. The turnover of plasma and liver glutathione, labeled from body water was previously reported (9). Analytical Procedures The concentration and mass isotopomer distribution (MID) of glucose were assayed by GC-MS of the pentaacetate and permethyl derivatives, respectively. Lactate and formate MID were assayed as the pentafluorobenzyl derivative (22,23). The 2H-enrichment of water was assayed after isotopic equilibration with unlabeled acetone in alkaline medium (24). The enrichment of deoxyribose, isolated from DNA, was assayed as the pentaacetate derivative (15). LC-MS analysis was used to assay the MID of CoA (25), glucose-6-P, ribose-5P, ATP, ADP, AMP, PEP and 3-P-glycerate (26). Fragmentation of CoA allowed to calculate the labeling of following components: adenine, ribose, adenosine, panthetheine and cysteine (27). Enzymatic assays were used for the concentrations of CoA and adenine nucleotides. Calculations and statistics. Measured mass isotopomer distributions were corrected for natural enrichment as in (28). Statistical differences were assayed by t test using the Prism software. 110 Results In vivo experiments. The body water of two groups of rats (6 and 19 rats) was kept 2.5% 2H-enriched for up to 10 and 31 days, respectively (9). We assayed the M1 enrichment of liver CoA and its building blocks (Fig. 4.12, for the 31 day group), as well as the 2Henrichment of plasma formate (Fig. 4.12, lower curve). The data of the labeling patterns were fitted to monoexponential saturation curves (Table 4.1). The apparent fractional turnover rates (k in day-1) were different for the CoA components. Also, the apparent fractional turnover rates were lower in the 31 day experiment compared to the 10 day experiment. The number of 2H atoms incorporated into CoA and its components was calculated by dividing the extrapolated enrichment at infinite time by the 2H-enrichment of body water. This number of 2H atoms was greater in the 31-day than in the 10-day experiment, although no statistical significance on differences in 2H incorporation could be calculated. The data clearly show that the labeling kinetics of CoA and its components cannot be calculated from monoexponential saturated curves. We assayed the 2H-enrichment of deoxyribose from DNA isolated from the livers of the second groups of rats (body water 2.5% 2H-enriched for 10 days). Fig 4.13 shows that the labeling profile of dR-DNA was well fitted to a monoexponential saturation curve (k = 0.17 ± 0.02; R2 = 0.98). Dividing the extrapolated dR-DNA enrichment at infinite time (1.26%) by the 2H-enrichment of body water (2.5%) yielded an apparent 0.5 2H atom incorporated per dR-DNA residue. Hellerstein’s 111 group had reported that the number of 2H atoms incorporated per dR-DNA residue is 3.5 (14,15). Thus, although the monoexponential saturation curve yielded an excellent fitting of our data, this excellent fitting does not justify the use of monoexponential labeling kinetics. Rat livers perfused in 100% 2H2O buffer. Two series of livers were perfused with 4 mM unlabeled glucose in buffer made up in 100% 2H2O. In one series, livers were frozen at 120 min. In the 2nd series, samples of liver were taken every 30 min and quick frozen. The first series allowed following the MID of metabolites in the perfusate modified by a constant liver mass. The second series allowed following the MID of intracellular metabolites in livers the mass of which decreased every 30 min. In both series, the MID of perfusate glucose was assayed throughout the experiment. Fig 4.14 shows, for the series without biopsies, the MID of perfusate glucose characterized by the almost linear accumulation of M1 to M7 mass isotopomers. In the M7 mass isotopomers, all C-H bonds of glucose are labeled. The M4 to M7 isotopomers must be labeled in the two triose moieties of glucose (29). These mass isotopomers must be formed by a combination of glycolysis, citric acid cycle and gluconeogenesis. The M1 to M3 mass isotopomers could be labeled in one or both triose moieties of glucose. The most abundant mass isotopomer, M1, corresponds to a population of 7 positional isotopomers in which one of the 7 CH groups is 2H-labeled. The most abundant of the positional isotopomers is most likely [2-2H]glucose because 2H-labeling on C-2 of glucose-6-P occurs via both glycogenolysis and gluconeogenesis before glucose-6-P is hydrolyzed by 112 glucose-6-Pase (7,29). In support of this interpretation, Fig 4.15 shows the labeling patterns of glucose-6-P, ribose-5-P and PEP which show almost all possible deuterated mass isotopomers (except for M4 of ribose-5-P which was not detected). The MID of glucose-6-P (in plateau during the 2nd hour of the experiment) shows a clear precursor-to-product relationship with the MID of the large pool of perfusate glucose which becomes progressively labeled with time. The MID of ribose-5-P is fairly stable during the 2nd hour with a predominance of the M1 isotopomer. Fig 4.16 shows that the M1 labeling of the 3 adenine nucleotides plateaued at about 60% while that of CoA increased slowly over the 2 hr experiment. The data illustrate the rapid interconversion of the 3 adenine nucleotides, and the precursor-to-product relationship between AMP and CoA. Note that the total 2Hlabeling of AMP is much greater than that of its precursor ribose-5-P (see Discussion). We were unable to measure the enrichment of the very small pool of phosphoribosylpyrophosphate. As one follows the isotopomer patterns from glucose-6-P to ribose-5-P, to adenine nucleotides, one notes the increasingly dominance of the M1 isotopomers. The labeling of the deoxyribose moiety of DNA was not detected at the end of the 2 hr experiment. To test whether in livers perfused with 100% 2H2O, the syntheses of adenine nucleotides and CoA could be inhibited by the high 2H-enrichment, we conducted perfusions with buffer made up in 0 to 100% 2H2O + 4 mM unlabeled glucose. Fig 4.17 shows that the labeling of adenine nucleotides and of CoA increased almost linearly with the 2H-enrichment of perfusate water. Most of the label in CoA was 113 in the ribose moiety. Very low labeling was detected in the adenine moiety. Small fractions of CoA labeling were found on the pantetheine moiety (Fig 4.18). Because all labeled glucose isotopomers were released in the perfusate via glucose-6-P and glucose-6-phosphatase, we used 2 calculations to estimate a minimal flux through this enzyme in intact perfused livers. The first calculation is based on the accumulation of labeled glucose isotopomers in the perfusate: Flux1 = [(total mol fraction of M1 to M7 glucose isotopomers at 120 min)(total glucose in perfusate)]/[(liver dry weight)(120 min)]. This calculation does not include the release of unlabeled glucose from the unlabeled fraction of glucose6-P. The second calculation uses the precursor-to-product relationship between the M1 enrichments of glucose-6-P and glucose: Flux2 = [(mol fraction of M1 glucose at 120 min)(total glucose in perfusate)]/[(mol fraction of M1 G6P)(liver dry weight)(120 min)] The second calculation was conducted using the most abundant isotopomers of glucose and glucose-6-P, i.e., M1. The two calculated fluxes are 0.55 ± 0.01 and 0.60 ± 0.1 μmol⋅min−1⋅(g dry wt)−1, respectively (SE, n = 5). These are minimal fluxes because some labeled glucose molecules must have cycled more than once through the glucose ➔ glucose-6-P ➔ glucose cycle. These values are similar to those reported by Katz et al (30) who measured glucose-6-P dephosphorylation in hepatocytes incubated with [2-3H]glucose [26 μmol⋅hr−1⋅(100 mg protein)−1 which is equivalent to 0.43 μmol⋅min−1⋅(g dry wt)−1]. 114 Rat livers perfused with [13C6]glucose. Two series of livers were perfused with 4 mM [13C6]glucose in buffer made up in normal water. In one series, livers were frozen at 120 min. In the 2nd series, samples of liver were taken every 30 min and quick frozen. Fig 4.19 shows the isotopomer distribution of perfusate glucose. Because the enrichment of commercial [13C6]glucose is 99% for each carbon, the M6 and M5 enrichments of perfusate glucose at zero time were 95 and 3%, respectively as expected. The M6 enrichment of glucose decreased from 95 to 78% over 2 h. During the same period, the proportion of unlabeled glucose (M) in the perfusate increased from almost zero to 8%. This reflects the dilution of labeled perfusate glucose by unlabeled glucose derived from glycogenolysis. In parallel glucose became slightly enriched with M1 to M4 isotopomers. These variations in isotopomer distribution of glucose reflect the cycling between perfusate glucose and glycolytic, gluconeogenic, pentose phosphate pathway and citric acid cycle intermediates. This interpretation is supported by the MIDs of glucose-6-P, ribose-5-P and glycerate-3-P (Fig 4.20). The total proportion of labeled mass isotopomers of glucose-6-P (M1 to M6) is about 50% during the 2nd hour of the experiment. Thus, about one-half of the glucose-6-P derived from unlabeled glycogen. The presence of M1 to M5 mass isotopomers of glucose-6-P results from the loss of label from [13C6]glucose in (i) the citric acid cycle, and (ii) the pyruvate ➔ oxaloacetate ➔ PEP ➔ pyruvate cycle, before labeled triose units are recombined into glucose-6-P. Indeed, the MID of glycerate-3-P shows similar proportions of the M1 to M3 mass isotopomers (Fig 4.20C). 115 During the last 30 min of the perfusions, the labeling pattern of ribose-5-P (Fig 4.20) was fairly stable, with a total sum of labeled mass isotopomers (M1 to M5) of about 22%. This labeled ribose-5-P is the precursor for the synthesis of adenine nucleotides. At 120 min, the total labeling of AMP and ATP (Fig 4.21A, 4.21B) was about 23% of the total labeling of ribose-5-P. Because ATP is the precursor of CoA synthesis, the total labeling of CoA (Fig 4.21C) at 120 min was lower (3%) than the total labeling of ATP, as expected from the precursor-toproduct relationship. Rat livers perfused with unlabeled glucose + [13C5]ribose. One series of livers were perfused with 4 mM unlabeled glucose + 2 mM [13C5]ribose in buffer made up in normal water. Samples of liver were taken every 30 min and quick frozen. Fig 4.22 shows the mass isotopomer distribution of perfusate glucose which becomes progressively labeled with all possible mass isotopomers (M1 to M6). Fig 4.23B shows the isotopomer distribution of ribose-5-P, the first metabolite labeled from [13C5]ribose. The main isotopomer is M5 the enrichment of which stabilizes at about 33% during the 2nd hour of the perfusion. The M1 to M4 isotopomers, which account for about 10% of all ribose-5-P, derive most likely from the reversible reactions of the non-oxidative branch of the pentose phosphate pathway. The total percentage of the labeled isotopomers of ribose-5P is about 45%. Thus, slightly more than half of ribose-5-P was unlabeled. 116 The two trioses, glycerate-3-P and PEP are M1 to M3 labeled, with M3 being the main mass isotopomer. Glucose-6-P shows M1 to M3 and M6 mass isotopomers. Clearly, the mass isotopomer distribution of glucose-6-P results from the combination of labeled triose units. The labeling pattern of glucose-6-P explains the accumulation of the M1 to M6 isotopomers of glucose. Discussion In vivo experiments When a metabolite becomes labeled with a time profile suggesting a saturation curve, it is tempting to fit the label vs time data to a monoexponential saturation curve. This is justified when the metabolite becomes labeled in a single net synthetic process (not by isotopic exchange) from a precursor with constant isotopic enrichment. During the synthesis of complex molecules made of different building blocks, e.g., proteins, adenine nucleotides, CoA or DNA, each building block can become labeled at single or multiple sites. Our data show that when liver CoA becomes labeled from 2H-enriched body water, each of the building blocks of CoA becomes labeled with different kinetics (Fig 4.22, Table 4.1). Also, the computed kinetics parameters change with the duration of the experiment (Table 4.1). In addition, when conducting long-term in vivo experiments with 2Henriched body water, one must realize that the experimental model is open. Although the 2H-enrichment of body water can easily be kept constant by labeling drinking water, the constant supply of unlabeled substrates from the diet dilutes the labeling of intermediates and impacts on the kinetics. Lastly, when the 117 synthesis of the complex molecule uses a combination of de novo synthesis and salvage pathways, the incorporation of label into the product via some of the salvage pathways can be delayed until the intermediates of the salvage pathways become labeled from the degradation of the labeled polymer that accumulated in the early phase of the experiments. Thus, kinetic parameters of complex molecules should be interpreted with caution. This was recognized by Hellerstein who pioneered the use of 2 H-enriched water to monitor DNA synthesis and cell turnover (14,15). Hellerstein proposed to calculate fractional cell division by the 2 H labeling ratio (deoxyribose in DNA of cells of interest)/(deoxyribose in DNA of fully-turnovered reference cells). This ratio provides a useful yardstick for estimating cell turnover under physiological and pathological conditions. Of particular interest is the use of this ratio to monitor the effectiveness of the treatment of malignancies (20,31). Liver perfusion experiments. We recently found that, in rat livers perfused with buffer made in 100% 2H2O, CoA was substantially labeled after 2 hours. Because CoA, adenine nucleotides and nucleic acids share the same early steps of synthesis via de novo and salvage pathways, we decided to examine in detail the dynamics of adenine nucleotides and CoA labeling from 2 H-enriched water and from relevant [13C]substrates (glucose and ribose). We selected the isolated liver as a closed system with a limited pool of substrates. In this model, we followed the labeling patterns of the precursors of adenine nucleotides and CoA synthesis. This led to estimates of fractional turnover rates of these compounds. 118 The time profiles of the mass isotopomer distribution of perfusate glucose, labeled from any of 3 different isotopic substrates (2H2O, [13C6]glucose or [13C5]ribose) provide evidence of constant glycolysis and gluconeogenesis. This, in spite of the near constancy of the glucose concentration in the perfusate (4 mM at zero time and 3.7 mM at 120 min). The presence of all possible labeled glucose mass isotopomers (M1 to M7 from 2 H2O and M1 to M6 from [13C6]glucose or [13C5]ribose) demonstrates that the labeling pattern of trioses is modified by reactions of the citric acid cycle and of the substrate cycle pyruvate ➔ oxaloacetate ➔ PEP ➔ pyruvate. For example, in livers perfused with [13C6]glucose, trioses which must be initially M3, become M1 + M2 + M3 labeled via citric acid cycle and pyruvate cycle reactions (Fig 4.20). In citric acid cycle intermediates, exchanges of 13 C for 12 C result from (i) reversibility of decarboxylating reactions (32) and (ii) randomization of the labeling of oxaloacetate via the rapidly reversible reactions catalyzed by malate dehydrogenase and fumarase (33). Recombination of two trioses with M to M3 mass isotopomers yields glucose molecules that are M to M6. Although the release of unlabeled (M) glucose is not visible from the mass isotopomer distribution of perfusate glucose (Fig 4.19), it is inferred from the fraction of glucose-6-P that is unlabeled (about 55%, Fig 4.19). A similar rationale can be formulated for the mass isotopomer distribution of glucose (i) in livers perfused in 100% 2H2O buffer, or (ii) in livers perfused with regular buffer + 4 mM unlabeled glucose + 2 mM [13C5]ribose. 119 The re-distribution of label [13C6]glucose or [13C5]ribose administered in vivo or added to in vitro preparations had been described previously. The mass isotopomer distribution of glucose labeled from highly 2H-enriched water has not been previously described to our best review of the literature. We followed the mass isotopomer distribution of glucose and related compounds to assess whether the MID of ribose-5-P would be sufficiently stable to be used to calculate the turnover of adenine nucleotides and of CoA. Our data show that the labeling pattern of ribose-5-P became fairly constant after 30 min of perfusion under conditions when label reaches ribose-5-P from 2 H2O, [13C6]glucose or [13C5]ribose (Figs 4.15, 4.20, 4.23). In perfusions conducted with [13C6]glucose, the comparison of the MIDs of glucose-6-P and ribose-5-P (Figs 4.20A and 4.20B) provides information on the conditions of operation of the pentose phosphate pathway in these livers. The M6 enrichment of glucose-6-P (30 - 35% after 90 min) is much higher that the M5 enrichment of ribose-5-P (4 - 4.5%). If all ribose-5-P had been formed in the oxidative branch of the pentose phosphate pathway, the M5 enrichment of ribose-5-P should be close to the M6 enrichment of glucose-6-P. This is because the removal of C-1 of [13C6]glucose-6-P would result in the formation of a M5 pentose-P. This was not the case. Therefore, in these livers, most of the ribose5-P was formed in the reversal of the non-oxidative branch of the pentose phosphate pathway. The reversal of this branch involves multiple combinations between intermediates with 3, 4, 5, 6 and 7 carbons. The probability that these multiple combinations will yield M5 ribose-5-P is low. This explains the low M5 120 enrichment of ribose-5-P. In these livers from overnight-fasted rats perfused with a low glucose concentration (4 mM), rates of fatty acid synthesis are low: about 15% of rates measured in livers from fed rats perfused with a high glucose concentration (21). Therefore, in the livers used in the present study, the requirement for NADPH production via the pentose phosphate pathway was low. This explains why the MID of ribose-5-P is compatible with it being formed mostly by the reversal of the non-oxidative branch of the pentose phosphate pathway. In livers perfused with 100% 2H2O buffer, the MIDs of ribose-5-P and of AMP (Figs 4.15, 4.16) were not in an usual precursor-to-product relationship where the labeling of the product would be lower than that of the precursor. In this case, the much higher M1 labeling of AMP compared to ribose-5-P shows that one 2H atom from the buffer was incorporated between ribose-5-P and AMP. Multiple reaction monitoring of the mass spectrum of AMP revealed that most of the 2Hlabeling was in the ribose moiety. We were unable to detect PRPP and measure its labeling. To interpret the difference in the MIDs of ribose-5-P and AMP, one must consider the different sources of the adenosine nucleus of AMP. Note that the 3 adenine nucleotides had almost identical labeling patterns, reflecting their rapid interconversion via ADP re-phosphorylation and the adenylate kinase reaction. The relevant sources of AMP in short-term experiments where DNA and RNA are unlabeled are: (i) de novo synthesis with construction of the adenine moiety, (ii) salvage of adenine from RNA and DNA breakdown followed by reaction with PRPP catalyzed by adenine phosphoribosyl transferase, and (iii) salvage of nucleoside (adenine-ribose) from the breakdown of RNA. 121 The de novo synthesis of AMP with construction of the adenine moiety involves multiple steps of 2H incorporation. First, one 2H atom is incorporated at the inversion of configuration between α-PRPP and 5-phospho-β-D-ribosylamine. Second, two 2H are incorporated via two reactions involving N10-formyl H4 folate derived from formate. Thus, in a liver perfused with 100% 2H2O buffer, the de novo synthesis of AMP with construction of the adenine moiety should yield AMP molecules labeled on the ribose moiety and the adenine moiety. However, in our experiments, the labeling of AMP showed only small proportions of mass isotopomers heavier than M1. The synthesis of AMP via the salvage of adenine from RNA and DNA breakdown followed by reaction with PRPP catalyzed by APRT should yield only M1 AMP when the perfusion is conducted in 100% 2H2O buffer. This is because of the inversion of configuration of C-1 of the ribose moiety of α-PRPP when it is converted to adenosine. Lastly, the synthesis of AMP by phosphorylation of adenosine (adenine-ribose) should yield unlabeled AMP. This is because, in short-term experiments, adenosine derived from RNA breakdown is not labeled. Because the M1 enrichment of AMP remains stable at about 60% during the 2nd hour of the experiment, about 40% of the AMP produced was unlabeled, and presumably was formed via phosphorylation of salvaged adenosine. The 60% M1 AMP was made from ribose-5-P which was about 15% M1 labeled, probably mostly via reaction of PRPP with adenine. It is not clear whether the 15% M1 enrichment of ribose-5-P is a component of the 60% M1 enrichment of AMP. This is because we do not know the distribution of 2H-labeling between the carbons of 122 ribose-5-P. Because the M2/M5 abundance ratio is equally low in ribose-5-P and in AMP, it is likely that very little if any AMP was synthesized with building up the adenine nucleus during the 2 h of the experiment. In perfusions with 2 mM [13C5]ribose, the main isotopomer of ribose-5-P is M5 (about 32% during the 2nd hour (Fig 4.23). One would expect that in the presence of 2 mM [13C5]ribose, most ribose-5-P would derive from the phosphorylation of [13C5]ribose by ribokinase. In fact, about 60% of ribose-5-P was unlabeled. This, and the dominance of the M5 isotopomer of ribose-5-P compared with the multiple mass isotopomer distribution of glucose-6-P and of gluconeogenic intermediates (PEP, glycerate-3-P) suggests that little label reached ribose-5-P via the two branches of the pentose phosphate pathway. This suggests that most unlabeled ribose-5-P arises by processes that would not be fed back by a high concentration of ribose-5-P. A likely source of unlabeled ribose-5-P is the nucleoside phosphorylases which form nucleobases and ribose-1-P. The latter is converted to ribose-5-P by phosphopentomutase (34). The action of nucleosidase on nucleosides derived from RNA degradation releases free unlabeled ribose which, after phosphorylation, somewhat dilutes the M5 enrichment of exogenous ribose-5-P. Overall, our data suggest that, in perfusions with [13C5]ribose, the bulk of ribose-5-P arises from the salvage pathways of RNA degradation via nucleoside phosphorylases and nucleosidases. This is also likely in the absence of exogenous ribose since in the presence of 2H2O or [13C6]glucose, most ribose-5-P is unlabeled. 123 In perfusions in 100% 2H2O buffer, the stability of the M1 enrichment of adenine nucleotides (60%, Fig 4.16 A-C) and the fairly linear increase in M1 labeling of CoA (0.56%/min from 60 to 120 min, Fig 4.16 D) allowed calculating the fractional turnover rate of CoA of 0.93%/min or 56%/h. Because free CoA (the actual analyte) exchanges probably rapidly with all CoA esters, the fractional turnover rate of 56%/h probably applies to the whole CoA pool (free and esterified). In perfusions with 4 mM unlabeled glucose + 2 mM [13C5]ribose, the stability of the M5 enrichment of ribose-5-P (33%, Fig 4.23) and the fairly linear increase in M5 labeling of AMP (2.2%/h, Fig 4.24) allowed calculating a fractional turnover rate of AMP of 6.7%/h). This fractional turnover rate applies to the three adenine nucleotides which are in isotopic equilibrium (Fig 4.24). In conclusion, our study revealed the rapid turnover of the nucleus of adenine nucleotides and of CoA in rat liver. It appears that most of these turnover are fueled by salvage pathways that recycle purine bases and nucleosides. Our findings open the way to studies on the modulation of adenine nucleotides and CoA turnover in physiological and pathological conditions. 124 Abbreviations: GC-MS, gas chromatography-mass spectrometry; LC-MS, liquid chromatography-mass spectrometry; MID, mass isotopomer distribution Footnote. 1. Mass isotopomers are designated as M, M1, M2,...Mn where n is the number of heavy atoms in the molecule. In the context of this paper, mass isotopomers are refered to as “isotopomers”. The isotopic enrichment of each isotopomer is expressed as mol percent. Acknowledgments This work was supported by the NIH (Roadmap grant R33DK070291 and grant R01ES013925.). We thank the Case Mouse Metabolic Phenotyping Center for help with the in vivo experiments. Reference List 1. Rittenberg, D. and Schoenheimer, R. (1937) J. Biol. Chem. 117, 485-490 2. Levy, L. M. and Betts, G. F. (1989) Biochim. Biophys. Acta 997, 331-333 3. Babu, U. M. and Johnston, R. B. (1974) Biochem. Biophys. Res. Commun. 58, 460-466 125 4. Jungas, R. L. (1968) Biochemistry 7, 3708-3717 5. Wong, W. W., Hachey, D. L., Feste, A., Leggitt, J., Clarke, L. L., Pond, W G., and Klein, P. D. (1991) J Lipid Res. 32, 1049-1056 6. Lee, W. N., Bassilian, S., Ajie, H. O., Schoeller, D. A., Edmond, J., Bergner, E. A., and Byerley, L. O. (1994) Am. J Physiol 266, E699-E708 7. Landau, B. R., Wahren, J., Chandramouli, V., Schumann, W. C., Ekberg, K., and Kalhan, S. C. (1996) J Clin Invest 98, 378-385 8. Previs, S. F., Fatica, R., Chandramouli, V., Alexander, J. C., Brunengraber, H., and Landau, B. R. (2004) Quantifying rates of protein synthesis in humans by use of 2H2O: application to patients with end-stage renal disease. 9. Kombu, R. S., Zhang, G. F., Abbas, R., Mieyal, J. J., Anderson, V. E., Kelleher, J. K., Sanabria, J. R., and Brunengraber, H. (2009) Am. J Physiol Endocrinol. Metab 297, E260-E269 10. Wang, B., Sun, G., Anderson, D. R., Jia, M., Previs, S., and Anderson, V. E. (2007) Isotopologue distributions of peptide product ions by tandem mass spectrometry: quantitation of low levels of deuterium incorporation. 11. Busch, R., Kim, Y. K., Neese, R. A., Schade-Serin, V., Collins, M., Awada, M., Gardner, J. L., Beysen, C., Marino, M. E., Misell, L. M., and Hellerstein, M. K. (2006) Biochim. Biophys. Acta 1760, 730-744 12. Xiao, G. G., Garg, M., Lim, S., Wong, D., Go, V. L., and Lee, W. N. (2008) J Appl. Physiol 104, 828-836 13. Dufner, D. A., Bederman, I. R., Brunengraber, D. Z., Rachdaoui, N., IsmailBeigi, F., Siegfried, B. A., Kimball, S. R., and Previs, S. F. (2005) Am. J Physiol Endocrinol. Metab 288, E1277-E1283 14. Neese, R. A., Misell, L. M., Turner, S., Chu, A., Kim, J., Cesar, D., Hoh, R., Antelo, F., Strawford, A., McCune, J. M., Christiansen, M., and Hellerstein, M. K. (2002) Proc Natl Acad Sci U S A 99, 15345-15350 15. Voogt, J. N., Awada, M., Murphy, E. J., Hayes, G. M., Busch, R., and Hellerstein, M. K. (2007) Nat. Protoc. 2, 3058-3062 16. Wadke, M., Brunengraber, H., Lowenstein, J. M., Dolhun, J. J., and Arsenault, G. P. (1973) Biochemistry 12, 2619-2624 17. Endemann, G., Goetz, P. G., Tomera, J. F., Rand, W. M., Desrochers, S., and Brunengraber, H. (1987) Biochem Cell Biol. 65, 989-996 126 18. Yuan, C. L., Sharma, N., Gilge, D. A., Stanley, W. C., Li, Y., Hatzoglou, M., and Previs, S. F. (2008) Am. J Physiol Endocrinol. Metab 295, E216-E222 19. Collins, M. L., Eng, S., Hoh, R., and Hellerstein, M. K. (2003) J Appl. Physiol 94, 2203-2211 20. Mohri, H., Perelson, A. S., Tung, K., Ribeiro, R. M., Ramratnam, B., Markowitz, M., Kost, R., Hurley, A., Weinberger, L., Cesar, D., Hellerstein, M. K., and Ho, D. D. (2001) J Exp. Med. 194, 1277-1287 21. Brunengraber, H., Boutry, M., and Lowenstein, J. M. (1973) Fatty acid and 3-beta-hydroxysterol synthesis in the perfused rat liver. 22. Hazey, J. W., Yang, D., Powers, L., Previs, S. F., David, F., Beaulieu, A. D., Puchowicz, M. A., Potter, J. L., Palmquist, D. L., and Brunengraber, H. (1997) Anal Biochem 248, 158-167 23. Tomcik, K., Ibarra, R. A., Sadhukhan, S., Han, Y., Tochtrop, G. P., and Zhang, G. F. (2011) Anal Biochem 410, 110-117 24. Yang, D., Diraison, F., Beylot, M., Brunengraber, D. Z., Samols, M. A., Anderson, V. E., and Brunengraber, H. (1998) Anal Biochem 258, 315-321 25. Zhang, G. F., Kombu, R. S., Kasumov, T., Han, Y., Sadhukhan, S., Zhang, J., Sayre, L. M., Ray, D., Gibson, K. M., Anderson, V. A., Tochtrop, G. P., and Brunengraber, H. (2009) J Biol. Chem 284, 33521-33534 26. Yang, W. C., Sedlak, M., Regnier, F. E., Mosier, N., Ho, N., and Adamec, J. (2008) Anal. Chem 80, 9508-9516 27. Dalluge, J. J., Gort, S., Hobson, R., Selifonova, O., Amore, F., and Gokarn, R. (2002) Anal. Bioanal. Chem. 374, 835-840 28. Fernandez, C. A., Des Rosiers, C., Previs, S. F., David, F., and Brunengraber, H. (1996) J Mass Spectrom. 31, 255-262 29. Chandramouli, V., Ekberg, K., Schumann, W. C., Wahren, J., and Landau, B. R. (1999) Am. J Physiol 277, E717-E723 30. Katz, J., Wals, P. A., and Rognstad, R. (1978) J Biol Chem 253, 4530-4536 31. Kim, S. J., Turner, S., Killion, S., and Hellerstein, M. K. (2005) Biochem. Biophys. Res. Commun. 331, 203-209 32. Yang, L., Kasumov, T., Kombu, R. S., Zhu, S. H., Cendrowski, A. V., David, F., Anderson, V. E., Kelleher, J. K., and Brunengraber, H. (2008) Metabolomic and mass isotopomer analysis of liver gluconeogenesis and citric acid cycle: II. Heterogeneity of metabolite labeling pattern. 127 33. Magnusson, I., Schumann, W. C., Bartsch, G. E., Chandramouli, V., Kumaran, K., Wahren, J., and Landau, B. R. (1991) J. Biol. Chem. 266, 69756984 34. Tozzi, M. G., Camici, M., Mascia, L., Sgarrella, F., and Ipata, P. L. (2006) FEBS J 273, 1089-1101 128 Table 4.1. Apparent kinetics of the labeling of CoA and its components from 2Henriched body water in rats over 10 and 31 days 2H ( 10 d) 2H ( 31 d) k (10 d) k (31 d) Adenine 0.24 ± 0.1 0.19 ± 0.03 1.1 1.2 Ribose 0.46 ± 0.08 0.41 ± 0.07 2.7 3.7 Nucleotide 0.79 ± 0.18 0.32 ± 0.04 3.8 4.9 Pantetheine 0.43 ± 0.06 0.41 ± 0.06 2.7 3.1 β-Alanine cysteamine 0.72 ± 0.23 0.33 ± 0.05 1.5 2 Whole CoA 0.45 ± 0.06 0.23 ± 0.04 6.6 8.5 E (t) = E inf (1- e-kt), k: rate constant (day-1), number of 2H = Einf % /2.5 % 129 Figure legends Figure 4.11. Sites of labeling of nucleotides, CoA and DNA from [2H]water. Figure 4.12. In vivo labeling of liver CoA from [2H]water over 31 days. Figure 4.13. In vivo labeling of liver dR-DNA [2H]water over 10 days Figure 4.14 Mass isotopomer distribution of liver perfusate glucose in 100% 2H2O buffer. Figure 4.15. Mass isotopomer distribution of glucose-6-P, ribose-5-P and PEP in livers perfused with 4 mM unlabeled glucose in 100% 2H2O buffer. Figure 4.16. M1 enrichment of AMP, ADP, ATP and CoA in livers perfused with 4 mM unlabeled glucose in 100% 2H2O buffer. Figure 4.17. M1 enrichment of AMP, ADP and ATP in livers perfused with 4 mM unlabeled glucose in buffer enriched 0 to 100% with 2H2O. Figure 4.18. M1 enrichment of CoA and its components in livers perfused with 4 mM unlabeled glucose in buffer enriched 0 to 100% with 2H2O. Figure 4.19. Mass isotopomer distribution of perfusate glucose in liver perfusion experiments starting with 4 mM [13C6]glucose. Figure 4.20. Mass isotopomer distribution of glucose-6-P, ribose-5-P and glycerate-3-P from livers perfused with 4 mM [13C6]glucose. 130 Figure 4.21. Mass isotopomer distribution of AMP, ATP and CoA in livers perfused with 4 mM [13C6]glucose. Figure 4.22. Mass isotopomer distribution of perfusate glucose in liver perfusion experiments starting with 4 mM unlableled glucose + 2 mM [13C5]ribose. Figure 4.23. Mass isotopomer distribution of glucose-6-P, ribose-5-P, PEP and glycerate-3-P from livers perfused with 4 mM unlableled glucose + 2 mM [13C5]ribose. Figure 4.24. Mass isotopomer distribution of AMP, ADP, ATP and CoA in livers perfused with 4 mM unlableled glucose + 2 mM [13C5]ribose. 131 Figure 4.11 132 Figure 4.12 2 Figure 4.13 134 Figure 4.14 135 Figure 4.15 136 Figure 4.16 A B AMP 70 ADP 70 60 50 M1 40 M2 30 M3 20 M4 10 M5 Mass Isotopomer Distribution (%) Mass Isotopomer Distribution (%) 60 0 M1 M2 M3 M4 M5 50 40 30 20 10 0 0 30 60 90 120 0 30 Time (min) Mass Isotopomer Distribution (%) D ATP 70 90 120 Time (min) CoA 70 60 M1 M3 M4 M5 50 40 30 20 10 Mass Isotopomer Distribution (%) C 60 0 M1 M3 M4 M5 60 50 40 30 20 10 0 0 30 60 Time (min) 90 0 120 137 30 60 Time (min) 90 120 Figure 4.17 80 A 70 AMP 60 Mass Isotopomer Distribution (%) 50 40 M1 30 M2 20 M3 10 M4 0 0 80 20 B 70 40 60 80 100 ADP 60 50 M1 40 M3 30 M4 20 M5 10 0 0 80 20 60 80 100 ATP C 70 40 60 50 40 M1 30 M3 20 M4 10 0 0 20 40 60 2H-enrichment 80 100 (%) 138 Figure 4.18 Mass Isotopomer Distribution (%) 50 45 40 M1 whole CoA 35 M1 nucleotide 30 25 M1 ribose 20 15 10 M1 adenine M1 pantetheine 5 β-alanine+ cysteamine 0 0 20 40 60 2H-enrichment of perfusate (%) 139 80 100 Figure 4.19 100 Mass Isotopomer Distribution (%) 90 80 70 60 50 M1 40 M3 M2 M4 30 M5 20 M6 M0 10 0 0 15 30 45 60 Time (min) 140 75 90 105 120 Figure 4.20 141 Figure 4.21 142 Figure 4.22 143 Figure 4.23 G6P labeling R5P labeling M1 20 M2 10 M3 0 0 30 60 90 120 MID ( %) MID (%) 30 M6 50 40 30 20 10 0 M1 M2 M3 M4 M5 0 30 Time (min) M1 20 M2 10 M3 0 90 30 MID ( %) MID (%) 30 60 120 Glycerate-3-P labeling 40 30 90 Time (min) PEP labeling 0 60 20 M1 10 M2 0 120 0 Time (min) 30 60 Time (min) 144 90 120 M3 Figure 4.24 5 Mass Isotopomer Distribution (%) 6 AMP labeling 4 M3 3 M4 2 M5 1 Mass Isotopomer Distribution (%) 6 ADP labeling 4 M3 M4 2 M5 0 0 0 30 60 90 0 120 30 90 120 Time (min) Time (min) 6 60 ATP labeling CoA labeling Mass Isotopomer Distribution (%) 6 4 M2 4 M3 M3 M4 M4 2 2 M5 M5 0 0 0 30 60 Time (min) 90 120 0 30 60 Time (min) 145 90 120 CHAPTER 5: IMPLICATIONS AND FUTURE DIRECTIONS 5.1 Project 1: C4- and C5-ketogenesis in rat liver 5.1.1 Results and discussion First, I studied the relationship between the uptake of C8, C7 and C3 fatty acids and the formation of C4- and C5-ketone bodies. The uptake of octanoate (Fig. 4.2A) was very similar to the uptake of heptanoate (Fig.4.2B). Octanoate catabolism only yields C4-ketone bodies. The yield of C4-ketone bodies from exogenous octanoate ranged from 80 to 90%. Acetyl-CoA derived from heptanoate is used to form both C5- and C4-ketone bodies. Only 40% of the propionyl moiety of heptanoate was converted to C5-ketone bodies. This results from the diversion of propionyl-CoA to anaplerosis and gluconeogenesis (Fig.4.1). Propionate is taken up by rat liver (Fig. 4.2C). However the virtually nil C5-ketogenesis from propionate demonstrates that, in the intact liver, thiolase does not allow the formation of BKP-CoA from propionyl-CoA + acetyl-CoA (Fig.4.1). I also perfused livers with two fatty acids to test the interaction between the uptakes of octanoate and heptanoate as well as the formation of C4- and C5ketone bodies. The data show that the competition favors octanoate uptake over heptanoate uptake. The rate of C5-ketogenesis from heptanoate is much lower than the rate of C4-ketogenesis from octanoate (Figs 4.3 and 4.4). Second, I assayed the labeling pattern of ketone bodies from livers perfused with increasing concentrations of [1-13C]octanoate (Fig.4.6A), or [8-13C]octanoate (Fig.4.6B). In the presence of [1-13C]octanoate, most of the labeling of BHB was on the C-1+2 acetyl, with relatively little label on the C-3+4 acetyl. The opposite 146 labeling was observed in perfusions with [8-13C]octanoate. This results from the fact that the C-3+4 acetyl of BHB derives from the C-7+8 acetyl of octanoate via the C-3+4 acetyl of AcAc-CoA. Third, the data shows that C4-ketogenesis and C5-ketogenesis share a pool of acetyl-CoA. The labeling patterns of ketone bodies, HMG-CoA and HEG-CoA show that when octanoate and heptanoate are used by the liver, acetyl-CoA derived from each substrate is available to both C4- and C5-ketogenesis. Fourth, I demonstrated the reversibility of the BHB-CoA dehydrogenase reaction in the intact liver. Initially unlabeled BHB-CoA and AcAc-CoA derived from βoxidation of [1-13C]octanoate become M1- and M2-labeled. This labeling results from the partial isotopic equilibration of AcAc-CoA and acetyl-CoA via 3-ketoacylCoA thiolase (Fig. 4.1, reaction 1). The M1 and M2 labeling of BHB-CoA (Fig. 4.9) show that the BHB-CoA dehydrogenase and the thiolase reactions are reversible in the intact liver despite the high rate of β-oxidation. Fifth, the data showed that heptanoate and propionate are anaplerotic substrates. Relative anaplerosis from [13C3]propionate increased faster with substrate concentration than relative anaplerosis from [5,6,7-13C3]heptanote (Fig.4.10A). This is because propionyl-moeity from heptanoate also goes to C5ketogenesis. The opposite occurred with absolute anaplerosis (Fig.4.10B). This probably results in a faster CAC flux in the presence of [5,6,7-13C3]heptanote (which supplies 2 acetyl-CoA) than in the presence of [13C3]propionate (which supplies no acetyl-CoA). Absolute anaplerosis from [5,6,7-13C3]heptanoate was significantly decreased in the presence of octanoate (Fig. 4.10B). This results 147 from the inhibition of heptanoate uptake by octanoate (Fig. 4.2B and 4.3A). Quite striking is the inhibition of labeling of glucose from [5,6,7-13C3]heptanote by unlabeled octanoate (Fig. 4.10C). This may results from the increase in the [NADH]/[NAD+] ratios induced by the rapid oxidation of octanoate, thus inhibiting gluconeogenesis. Concluding remarks overall, my data explored the interrelation between C4- ketogenesis, C5-ketogenesis, and anaplerosis. In the presence of octanoate and heptanoate, the uptake of octanoate and C4-ketogenesis prevail over the uptake of heptanoate and C5-ketogenesis. The virtual absence of C5-ketogenesis from propionate demonstrates that the mitochondrial 3-ketoacyl-CoA thiolase does not allow a net acyl-CoA condensation flux. These findings have clinical implications: i) the concentration of C5-ketone bodies in body fluids of patients with disorders of the propionyl-CoA pathway are formed via β-oxidation of odd-long-chain fatty acids synthesized from propionyl-CoA, and ii) the inhibition of anaplerosis and gluconeogenesis from heptanoate by octanoate has implications for the design of diets for the treatment of some metabolic diseases such as disorders of longchain fatty acid oxidation. It would not be advisable to progressively modify the patients’ diet to replace trioctanoin by triheptanoin because octanoate inhibits heptanoate uptake (Fig. 4.3B), C5-ketogenesis from heptanoate(Fig. 4.4B), and anaplerosis from heptanoate (Fig 4.10 A and B). 5.1.1 Future directions The present study shows that odd-chain fatty acids are anaplerotic substrates and even-chain fatty acids inhibit the uptake of odd-chain fatty acids in isolated 148 rat liver. Based on this study, I expect that odd-chain fatty acids could be used alone for the dietary treatment of patients with FODs. The decompensated patients with FODs have severe clinical symptoms under stress such as fasting, fever, infection or trauma. Those stresses stimulate catecholamine secretion and lipolysis. They also inhibit insulin secretion. This causes the patients’ shock or death. The traditional acute treatments for the decompensated patients involves infusing glucose and insulin to provide energy substrates. This treatment is not always effective. The use of triheptanoin is a good addition to the treatment of patients with FODs. Several knockout mice models with FODs have been developed. These models include inherited deficiencies in VLCAD (288; 289), LCAD (290), SCAD (291) and so on. I would choose VLCAD-/- mice as the animal model. Put the mice under stress conditions by fasting or cold exposure. The following treatment will be used to evaluate the recovery of VLCAD-/- mice from stress conditions: i) infusion of triheptanoin, ii) dietary treatment with triheptanoin alone, iii) dietary treatment with trioctanoin alone, iv) mix of triheptanoin and trioctanoin, V) possibly treatment with insulin and/or high glucose diet. I hypothesize that the administration of triheptanoin alone will most improve VLCAD -/- mice conditions under stress. Tissues including the liver, heart, muscle and brain will be isolated from mice for the analyses. C4- and C5ketone bodies, glucose will be analyzed by GC-MS. Free CoA and acyl-CoA esters will be analyzed by HPLC-MS. 149 5.2 Project 2: Tracing the syntheses of adenine nucleotides, CoA and DNA in rat liver 5.2.1 Results and discussion First, when rats were perfused with 100% 2 H2O buffer, [13C6]glucose, or [13C5]ribose, the changes of the labeling pattern of glycolytic intermediates and ribose-5-P provided evidence of constant glycolysis, gluconeogenesis and CAC operation. The presence of all possible labeled glucose mass isotopomers (M1 to M7 from 2H2O and M1 to M6 from [13C6]glucose or [13C5]ribose) demonstrates that the labeling pattern of trioses is modified by reactions of citric acid cycle and of the substrate cycle pyruvate → oxaloacetate → PEP → pyruvate (Figs 4.14 and 4.22). Second, in perfusions conducted with 4 mM [13C6]glucose, the comparison of the MIDs of glucose-6-P and ribose-5-P (Fig 4.20) provides information on the conditions of operation of the pentose phosphate pathway in these livers. The M6 enrichment of glucose-6-P (30-35% after 90 min) is much higher than the M5 enrichment of ribose-5-P (4-4.5%). This is because most of the ribose-5-P in these livers was formed in the reversal of the non-oxidative branch of the pentose phosphate pathway. The low enrichment of ribose-5-P resulted from the multiple combinations between intermediates with 3,4,5,6 and 7 carbons, with low probability to yield M5 ribose-5-P. These fasted rat livers had low fatty acid synthesis rates and the requirement for NADPH production via the oxidative branch of the pentose phosphate pathway was low. 150 Third, in livers perfused with 100% 2H2O buffer, the much higher M1 labeling of AMP compared to ribose-5-P shows that one 2H atom from the buffer was incorporated between ribose-5-P and AMP in the ribose moiety (Figs 4.15 and 4.16). ATP was labeled mainly from salvage pathways because it’s labeling shows only small proportions of mass isotopomers heavier than M1. The synthesis of M1 AMP via the salvage of adenine from RNA and DNA breakdown involves probably the inversion of configuration of C-1 of the ribose moiety of αPRPP when it is converted to adenosine by adenine phosphoribosyl transferase. This leads to the incorporation of 2H+ from the buffer on C-1 of the ribose moiety of AMP. Fourth, my data allow to calculate the fractional synthesis rates of adenine nucleotides and CoA. In perfusions in 100% 2H2O buffer, the fractional turnover rate of CoA is 0.56% / min or 33% / h. This rate probably applies to the whole CoA pool (free and esterified). In perfusions with 4 mM unlabeled glucose + 2 mM [13C5]ribose, the fractional turnover rate of AMP is 7%/h. This rate applies to the three adenine nucleotides which are in isotopic equilibrium (Fig 4.24) Concluding remarks: 1. My data show that during a short 2hr liver perfusion period, the rates of de novo synthesis of the adenine nucleotides and CoA in rat livers are very low. The measurements of the de novo synthesis rates need longer-term experiment. The adenine nucleotides and CoA are mainly synthesized from salvage pathways in rat livers perfused for 2hr. 151 2. In the fasted liver, glycolysis, gluconeogenesis, citric acid cycle and the pentose phosphate pathway are constantly cycling and changing the labeling patterns of their intermediates. 3. The non-oxidative branch of the pentose phosphate pathway provides more ribose-5-P than the oxidative branch in the fasted rat liver. 4. [2H]water is a good tracer that can be used in different time-scale experiments (in vivo for a long-term experiment, perfused isolated organ for a short-term experiment) to diagnose variations in ATP and DNA metabolism. 5.2.2 Future directions This project provides a useful model and method to measure the synthesis of adenine nucleotides, CoA and DNA in rat livers. Future work should include the following: 1. Using NMR, identify the rates of 2H incorporation into the ribose moiety of adenine nucleotides, CoA and DNA during long-term experiments. I hypothesize that the incorporation of 2H at different carbon positions (C-2-5) reflect the rate of de novo synthesis; 2H on C-1 reflects both of the de novo synthesis and the purine salvage pathways. 2. Perfusion of different isolated rat organs with 2H2O buffer during short-term experiments will evaluate the purine salvage pathways. 152 3. Clinical applications in patients with cancer or disorders of purine metabolism monitor the rates of synthesis of DNA labeling from [2H]water as an index of the rate of cell division (before and after chemotherapy). 153 Reference List 1. McGarry JD and Foster DW. Regulation of hepatic fatty acid oxidation and ketone body production. Annu Rev Biochem 49: 395-420, 1980. 2. Robinson AM and Williamson DH. Physiological roles of ketone bodies as substrates and signals in mammalian tissues. Physiol Rev 60: 143-187, 1980. 3. Balasse EO and Fery F. Ketone body production and disposal: effects of fasting, diabetes, and exercise. Diabetes Metab Rev 5: 247-270, 1989. 4. Pederson KJ. The ketonic decomposition of beta-carboxylic acids. J Am Chem Soc 51: 2098-2107, 1929. 5. Wildenhoff KE. Diurnal variations in the concentrations of blood acetoacetate, 3-hydroxybutyrate and glucose in normal persons. Acta Med Scand 191: 303-306, 1972. 6. Wildenhoff KE, Johansen JP, Karstoft H, Yde H and Sorensen NS. Diurnal variations in the concentrations of blood acetoacetate and 3hydroxybutyrate. The ketone body peak around midnight and its relationship to free fatty acids, glycerol, insulin, growth hormone and glucose in serum and plasma. Acta Med Scand 195: 25-28, 1974. 7. Bates MW, Krebs HA and Williamson DH. Turnover rates of ketone bodies in normal, starved and alloxan-diabetic rats. Biochem J 110: 655661, 1968. 8. Hawkins RA, Williamson DH and Krebs HA. Ketone-body utilization by adult and suckling rat brain in vivo. Biochem J 122: 13-18, 1971. 154 9. Owen OE, Felig P, Morgan AP, Wahren J and Cahill GF, Jr. Liver and kidney metabolism during prolonged starvation. J Clin Invest 48: 574-583, 1969. 10. Owen OE and Reichard GA, Jr. Human forearm metabolism during progressive starvation. J Clin Invest 50: 1536-1545, 1971. 11. Reichard GA, Jr., Owen OE, Haff AC, Paul P and Bortz WM. Ketonebody production and oxidation in fasting obese humans. J Clin Invest 53: 508-515, 1974. 12. Bates MW. Kinetics of ketone body metabolism in fasted and diabetic rats. Am J Physiol 221: 984-991, 1971. 13. Genuth SM and Castro J. Effect of oral alanine on blood betahydroxybutyrate and plasma glucose, insulin, free fatty acids, and growth hormone in normal and diabetic subjects. Metabolism 23: 375-386, 1974. 14. Fritz IB. Factors influencing the rates of long-chain fatty acid oxidation and synthesis in mammalian systems. Physiol Rev 41: 52-129, 1961. 15. Hanson PG, Johnson RE and Zaharko DS. Correlation between ketone body and free fatty acid concentrations in the plasma during early starvation in man. Metabolism 14: 1037-1040, 1965. 16. Ontko JA and Zilversmit DB. Correlation between concentrations of circulating free fatty acids and ketone bodies. Proc Soc Exp Biol Med 121: 319-321, 1966. 17. Eaton S. Control of mitochondrial beta-oxidation flux. Prog Lipid Res 41: 197-239, 2002. 155 18. Shepherd D, Yates DW and Garland PB. The relationship between the rates of conversion of palmitate into citrate or acetoacetate and the acetylcoenzyme A content of rat-liver mitochondria. Biochem J 97: 38C-40C, 1965. 19. McGarry JD, Mannaerts GP and Foster DW. A possible role for malonylCoA in the regulation of hepatic fatty acid oxidation and ketogenesis. J Clin Invest 60: 265-270, 1977. 20. McGarry JD, Leatherman GF and Foster DW. Carnitine palmitoyltransferase I. The site of inhibition of hepatic fatty acid oxidation by malonyl-CoA. J Biol Chem 253: 4128-4136, 1978. 21. MacKay EM. The significance of ketosis. J Clin Endocrionol 3: 101-110, 1943. 22. Endemann G, Goetz PG, Edmond J and Brunengraber H. Lipogenesis from ketone bodies in the isolated perfused rat liver. Evidence for the cytosolic activation of acetoacetate. J Biol Chem 257: 3434-3440, 1982. 23. Williamson DH, Bates MW, Page MA and Krebs HA. Activities of enzymes involved in acetoacetate utilization in adult mammalian tissues. Biochem J 121: 41-47, 1971. 24. Owen OE, Morgan AP, Kemp HG, Sullivan JM, Herrera MG and Cahill GF, Jr. Brain metabolism during fasting. J Clin Invest 46: 1589-1595, 1967. 156 25. Cremer JE and Heath DF. The estimation of rates of utilization of glucose and ketone bodies in the brain of the suckling rat using compartmental analysis of isotopic data. Biochem J 142: 527-544, 1974. 26. Edmond J. Ketone bodies as precursors of sterols and fatty acids in the developing rat. J Biol Chem 249: 72-80, 1974. 27. Webber RJ and Edmond J. Utilization of L(+)-3-hydroxybutyrate, D(-)-3hydroxybutyrate, acetoacetate, and glucose for respiration and lipid synthesis in the 18-day-old rat. J Biol Chem 252: 5222-5226, 1977. 28. Palaiologos G and Felig P. Effects of ketone bodies on amino acid metabolism in isolated rat diaphragm. Biochem J 154: 709-716, 1976. 29. Robinson AM and Williamson DH. Utlization of D-3-hydroxy[314C]butyrate for lipogenesis in vivo in lactating rat mammary gland. Biochem J 176: 635-638, 1978. 30. Jocken JW and Blaak EE. Catecholamine-induced lipolysis in adipose tissue and skeletal muscle in obesity. Physiol Behav 94: 219-230, 2008. 31. Fonseca-Alaniz MH, Takada J, onso-Vale MI and Lima FB. Adipose tissue as an endocrine organ: from theory to practice. J Pediatr (Rio J ) 83: S192-S203, 2007. 32. Votruba SB and Jensen MD. Regional fat deposition as a factor in FFA metabolism. Annu Rev Nutr 27: 149-163, 2007. 33. Coppack SW, Jensen MD and Miles JM. In vivo regulation of lipolysis in humans. J Lipid Res 35: 177-193, 1994. 157 34. Kather H, Wieland E, Scheurer A, Vogel G, Wildenberg U and Joost C. Influences of variation in total energy intake and dietary composition on regulation of fat cell lipolysis in ideal-weight subjects. J Clin Invest 80: 566-572, 1987. 35. Moro C, Polak J, Hejnova J, Klimcakova E, Crampes F, Stich V, Lafontan M and Berlan M. Atrial natriuretic peptide stimulates lipid mobilization during repeated bouts of endurance exercise. Am J Physiol Endocrinol Metab 290: E864-E869, 2006. 36. Reynisdottir S, Wahrenberg H, Carlstrom K, Rossner S and Arner P. Catecholamine resistance in fat cells of women with upper-body obesity due to decreased expression of beta 2-adrenoceptors. Diabetologia 37: 428-435, 1994. 37. Stralfors P and Honnor RC. Insulin-induced dephosphorylation of hormone-sensitive lipase. Correlation with lipolysis and cAMP-dependent protein kinase activity. Eur J Biochem 182: 379-385, 1989. 38. Holm C, Kirchgessner TG, Svenson KL, Fredrikson G, Nilsson S, Miller CG, Shively JE, Heinzmann C, Sparkes RS, Mohandas T and . Hormone-sensitive lipase: sequence, expression, and chromosomal localization to 19 cent-q13.3. Science 241: 1503-1506, 1988. 39. Li Z, Sumida M, Birchbauer A, Schotz MC and Reue K. Isolation and characterization of the gene for mouse hormone-sensitive lipase. Genomics 24: 259-265, 1994. 158 40. Contreras JA, Karlsson M, Osterlund T, Laurell H, Svensson A and Holm C. Hormone-sensitive lipase is structurally related to acetylcholinesterase, bile salt-stimulated lipase, and several fungal lipases. Building of a three-dimensional model for the catalytic domain of hormone-sensitive lipase. J Biol Chem 271: 31426-31430, 1996. 41. Anthonsen MW, Ronnstrand L, Wernstedt C, Degerman E and Holm C. Identification of novel phosphorylation sites in hormone-sensitive lipase that are phosphorylated in response to isoproterenol and govern activation properties in vitro. J Biol Chem 273: 215-221, 1998. 42. Holm C, Belfrage P and Fredrikson G. Immunological evidence for the presence of hormone-sensitive lipase in rat tissues other than adipose tissue. Biochem Biophys Res Commun 148: 99-105, 1987. 43. Khoo JC, Reue K, Steinber D and Schotz MC. Expression of hormonesensitive lipase mRNA in macrophages. J Lipid Res 34: 1969-1974, 1993. 44. Mulder H, Holst LS, Svensson H, Degerman E, Sundler F, Ahren B, Rorsman P and Holm C. Hormone-sensitive lipase, the rate-limiting enzyme in triglyceride hydrolysis, is expressed and active in beta-cells. Diabetes 48: 228-232, 1999. 45. Large V, Reynisdottir S, Langin D, Fredby K, Klannemark M, Holm C and Arner P. Decreased expression and function of adipocyte hormonesensitive lipase in subcutaneous fat cells of obese subjects. J Lipid Res 40: 2059-2066, 1999. 159 46. Shen WJ, Liang Y, Hong R, Patel S, Natu V, Sridhar K, Jenkins A, Bernlohr DA and Kraemer FB. Characterization of the functional interaction of adipocyte lipid-binding protein with hormone-sensitive lipase. J Biol Chem 276: 49443-49448, 2001. 47. Bezaire V and Langin D. Regulation of adipose tissue lipolysis revisited. Proc Nutr Soc 68: 350-360, 2009. 48. Langin D, Dicker A, Tavernier G, Hoffstedt J, Mairal A, Ryden M, Arner E, Sicard A, Jenkins CM, Viguerie N, van H, V, Gross RW, Holm C and Arner P. Adipocyte lipases and defect of lipolysis in human obesity. Diabetes 54: 3190-3197, 2005. 49. Haemmerle G, Lass A, Zimmermann R, Gorkiewicz G, Meyer C, Rozman J, Heldmaier G, Maier R, Theussl C, Eder S, Kratky D, Wagner EF, Klingenspor M, Hoefler G and Zechner R. Defective lipolysis and altered energy metabolism in mice lacking adipose triglyceride lipase. Science 312: 734-737, 2006. 50. Zimmermann R, Strauss JG, Haemmerle G, Schoiswohl G, BirnerGruenberger R, Riederer M, Lass A, Neuberger G, Eisenhaber F, Hermetter A and Zechner R. Fat mobilization in adipose tissue is promoted by adipose triglyceride lipase. Science 306: 1383-1386, 2004. 51. Kim JY, Tillison K, Lee JH, Rearick DA and Smas CM. The adipose tissue triglyceride lipase ATGL/PNPLA2 is downregulated by insulin and TNF-alpha in 3T3-L1 adipocytes and is a target for transactivation by PPARgamma. Am J Physiol Endocrinol Metab 291: E115-E127, 2006. 160 52. Fredrikson G, Tornqvist H and Belfrage P. Hormone-sensitive lipase and monoacylglycerol lipase are both required for complete degradation of adipocyte triacylglycerol. Biochim Biophys Acta 876: 288-293, 1986. 53. Blaak EE, van Baak MA, Kemerink GJ, Pakbiers MT, Heidendal GA and Saris WH. Beta-adrenergic stimulation of energy expenditure and forearm skeletal muscle metabolism in lean and obese men. Am J Physiol 267: E306-E315, 1994. 54. Fukao T, Lopaschuk GD and Mitchell GA. Pathways and control of ketone body metabolism: on the fringe of lipid biochemistry. Prostaglandins Leukot Essent Fatty Acids 70: 243-251, 2004. 55. Greenberg AS, Shen WJ, Muliro K, Patel S, Souza SC, Roth RA and Kraemer FB. Stimulation of lipolysis and hormone-sensitive lipase via the extracellular signal-regulated kinase pathway. J Biol Chem 276: 4545645461, 2001. 56. Greenberg AS, Egan JJ, Wek SA, Garty NB, Blanchette-Mackie EJ and Londos C. Perilipin, a major hormonally regulated adipocyte-specific phosphoprotein associated with the periphery of lipid storage droplets. J Biol Chem 266: 11341-11346, 1991. 57. Londos C, Brasaemle DL, Schultz CJ, Segrest JP and Kimmel AR. Perilipins, ADRP, and other proteins that associate with intracellular neutral lipid droplets in animal cells. Semin Cell Dev Biol 10: 51-58, 1999. 161 58. Moore HP, Silver RB, Mottillo EP, Bernlohr DA and Granneman JG. Perilipin targets a novel pool of lipid droplets for lipolytic attack by hormone-sensitive lipase. J Biol Chem 280: 43109-43120, 2005. 59. Granneman JG, Moore HP, Granneman RL, Greenberg AS, Obin MS and Zhu Z. Analysis of lipolytic protein trafficking and interactions in adipocytes. J Biol Chem 282: 5726-5735, 2007. 60. Schweiger M, Schreiber R, Haemmerle G, Lass A, Fledelius C, Jacobsen P, Tornqvist H, Zechner R and Zimmermann R. Adipose triglyceride lipase and hormone-sensitive lipase are the major enzymes in adipose tissue triacylglycerol catabolism. J Biol Chem 281: 40236-40241, 2006. 61. Mersmann HJ. Comparison of plasma free-fatty-acid and blood-glycerol concentrations with measurement of lipolysis in porcine adipose tissue in vitro. J Anim Sci 63: 757-769, 1986. 62. Vaughan M. The production and release of glycerol by adipose tissue incubated in vitro. J Biol Chem 237: 3354-3358, 1962. 63. Gu L, Zhang GF, Kombu RS, Allen F, Kutz G, Brewer WU, Roe CR and Brunengraber H. Parenteral and Enteral Metabolism of Anaplerotic Triheptanoin in Normal Rats. II. Effects on lipolysis, glucose production and liver acyl-CoA profile. Am J Physiol Endocrinol Metab 2009. 64. Mittendorfer B, Liem O, Patterson BW, Miles JM and Klein S. What does the measurement of whole-body fatty acid rate of appearance in 162 plasma by using a fatty acid tracer really mean? Diabetes 52: 1641-1648, 2003. 65. Horton TJ, Dow S, Armstrong M and Donahoo WT. Greater systemic lipolysis in women compared with men during moderate-dose infusion of epinephrine and/or norepinephrine. J Appl Physiol 107: 200-210, 2009. 66. Coppack SW, Frayn KN, Humphreys SM, Whyte PL and Hockaday TD. Arteriovenous differences across human adipose and forearm tissues after overnight fast. Metabolism 39: 384-390, 1990. 67. Spector AA. Fatty acid binding to plasma albumin. J Lipid Res 16: 165179, 1975. 68. Scowro and Chernick SS. Hormonal control of protein and fat metabolism in the pancreatectomized rat. Recent Prog Horm Res 16: 497545, 1960. 69. Meier JM, McGarry JD, Faloona GR, Unger RH and Foster DW. Studies of the development of diabetic ketosis in the rat. J Lipid Res 13: 228-233, 1972. 70. Alberti KG, Hockaday TD and Turner RC. Small doses of intramuscular insulin in the treatment of diabetic "coma". Lancet 2: 515-522, 1973. 71. Mayes PA and Felts JM. Regulation of fat metabolism of the liver. Nature 215: 716-718, 1967. 72. Hamilton JA and Kamp F. How are free fatty acids transported in membranes? Is it by proteins or by free diffusion through the lipids? Diabetes 48: 2255-2269, 1999. 163 73. Luxon BA. Inhibition of binding to fatty acid binding protein reduces the intracellular transport of fatty acids. Am J Physiol 271: G113-G120, 1996. 74. Norum KR, Farstad M and Bremer J. The submitochondrial distribution of acid:CoA ligase (AMP) and palmityl-CoA:carnitine palmityltransferase in rat liver mitochondria. Biochem Biophys Res Commun 22: 797-804, 1966. 75. Shindo Y and Hashimoto T. Acyl-Coenzyme A synthetase and fatty acid oxidation in rat liver peroxisomes. J Biochem 84: 1177-1181, 1978. 76. Kornberg A and Pricer WE, Jr. Enzymatic synthesis of the coenzyme A derivatives of long chain fatty acids. J Biol Chem 204: 329-343, 1953. 77. Gossett RE, Schroeder F, Gunn JM and Kier AB. Expression of fatty acyl-CoA binding proteins in colon cells: response to butyrate and transformation. Lipids 32: 577-585, 1997. 78. Cook GA and Park EA. Expression and regulation of carnitine palmitoyltransferase-Ialpha and -Ibeta genes. Am J Med Sci 318: 43-48, 1999. 79. Saggerson D. Malonyl-CoA, a key signaling molecule in mammalian cells. Annu Rev Nutr 28: 253-272, 2008. 80. Guynn RW, Veloso D and Veech RL. The concentration of malonylcoenzyme A and the control of fatty acid synthesis in vivo. J Biol Chem 247: 7325-7331, 1972. 81. Hardie DG. Regulation of fatty acid and cholesterol metabolism by the AMP-activated protein kinase. Biochim Biophys Acta 1123: 231-238, 1992. 164 82. Park H, Kaushik VK, Constant S, Prentki M, Przybytkowski E, Ruderman NB and Saha AK. Coordinate regulation of malonyl-CoA decarboxylase, sn-glycerol-3-phosphate acyltransferase, and acetyl-CoA carboxylase by AMP-activated protein kinase in rat tissues in response to exercise. J Biol Chem 277: 32571-32577, 2002. 83. Habinowski SA, Hirshman M, Sakamoto K, Kemp BE, Gould SJ, Goodyear LJ and Witters LA. Malonyl-CoA decarboxylase is not a substrate of AMP-activated protein kinase in rat fast-twitch skeletal muscle or an islet cell line. Arch Biochem Biophys 396: 71-79, 2001. 84. Lopaschuk GD and Stanley WC. Malonyl-CoA decarboxylase inhibition as a novel approach to treat ischemic heart disease. Cardiovasc Drugs Ther 20: 433-439, 2006. 85. Cook GA. Differences in the sensitivity of carnitine palmitoyltransferase to inhibition by malonyl-CoA are due to differences in Ki values. J Biol Chem 259: 12030-12033, 1984. 86. Grantham BD and Zammit VA. Restoration of the properties of carnitine palmitoyltransferase I in liver mitochondria during re-feeding of starved rats. Biochem J 239: 485-488, 1986. 87. Faye A, Borthwick K, Esnous C, Price NT, Gobin S, Jackson VN, Zammit VA, Girard J and Prip-Buus C. Demonstration of N- and Cterminal domain intramolecular interactions in rat liver carnitine palmitoyltransferase 1 that determine its degree of malonyl-CoA sensitivity. Biochem J 387: 67-76, 2005. 165 88. McGarry JD, Robles-Valdes C and Foster DW. Role of carnitine in hepatic ketogenesis. Proc Natl Acad Sci U S A 72: 4385-4388, 1975. 89. Louet JF, Le MC, Pegorier JP, Decaux JF and Girard J. Regulation of liver carnitine palmitoyltransferase I gene expression by hormones and fatty acids. Biochem Soc Trans 29: 310-316, 2001. 90. Park EA, Mynatt RL, Cook GA and Kashfi K. Insulin regulates enzyme activity, malonyl-CoA sensitivity and mRNA abundance of hepatic carnitine palmitoyltransferase-I. Biochem J 310 ( Pt 3): 853-858, 1995. 91. Jackson S, Bartlett K, Land J, Moxon ER, Pollitt RJ, Leonard JV and Turnbull DM. Long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency. Pediatr Res 29: 406-411, 1991. 92. Jackson S, Kler RS, Bartlett K, Briggs H, Bindoff LA, Pourfarzam M, Gardner-Medwin D and Turnbull DM. Combined enzyme defect of mitochondrial fatty acid oxidation. J Clin Invest 90: 1219-1225, 1992. 93. Kinman RP, Kasumov T, Jobbins KA, Thomas KR, Adams JE, Brunengraber LN, Kutz G, Brewer WU, Roe CR and Brunengraber H. Parenteral and enteral metabolism of anaplerotic triheptanoin in normal rats. Am J Physiol Endocrinol Metab 291: E860-E866, 2006. 94. Ibdah JA, Paul H, Zhao Y, Binford S, Salleng K, Cline M, Matern D, Bennett MJ, Rinaldo P and Strauss AW. Lack of mitochondrial trifunctional protein in mice causes neonatal hypoglycemia and sudden death. J Clin Invest 107: 1403-1409, 2001. 166 95. Lehninger AL. A quantitative study of the products of fatty acid oxidation in liver suspensions. J Biol Chem 164: 291-306, 2000. 96. Williamson JR, Scholz R and Browning ET. Control mechanisms of gluconeogenesis and ketogenesis. II. Interactions between fatty acid oxidation and the citric acid cycle in perfused rat liver. J Biol Chem 244: 4617-4627, 1969. 97. Clinkenbeard KD, Reed WD, Mooney RA and Lane MD. Intracellular localization of the 3-hydroxy-3-methylglutaryl coenzme A cycle enzymes in liver. Separate cytoplasmic and mitochondrial 3-hydroxy-3-methylglutaryl coenzyme A generating systems for cholesterogenesis and ketogenesis. J Biol Chem 250: 3108-3116, 1975. 98. Rudney H. The biosynthesis of beta-hydroxy-beta-methylglutaric acid. J Biol Chem 227: 363-377, 1957. 99. Reed WD, Clinkenbeard D and Lane MD. Molecular and catalytic properties of mitochondrial (ketogenic) 3-hydroxy-3-methylglutaryl coenzyme A synthase of liver. J Biol Chem 250: 3117-3123, 1975. 100. Casals N, Roca N, Guerrero M, Gll-Gomez G, Ayte J and Ciudad C.J.and Hegardt F.G. Regulation of the expression of mitochondrial 3hydroxy-3-methylglutaryl-CoA synthase gene. Biochem J 283: 261-264, 1992. 101. Lowe DM and Tubbs PK. Succinylation and inactivation of 3-hydroxy-3methylglutaryl-CoA synthase by succinyl-CoA and its possible relevance to the control of ketogenesis. Biochem J 232: 37-42, 1985. 167 102. Siess EA, Fahimi FM and Wieland OH. Decrease by glucagon in hepatic succinyl-CoA. Biochem Biophys Res Commun 95: 205-211, 1980. 103. Quant PA, Robin D, Robin P, Ferre P, Brand MD and Girard J. Control of hepatic mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase during the foetal/neonatal transition, suckling and weaning in the rat. Eur J Biochem 195: 449-454, 1991. 104. Leclerc J, Des Rosiers C., Montgomery JA, Brunet J, Ste-Marie L, Reider MW, Fernandez CA, Powers L, David F and Brunengraber H. Metabolism of R-beta-hydroxypentanoate and of beta-ketopentanoate in conscious dogs. Am J Physiol 268: E446-E452, 1995. 105. Sweetman L, Weyler W, Nyhan WL, de CC, Loria AR and Estrada Y. Abnormal metabolites of isoleucine in a patient with propionyl-CoA carboxylase deficiency. Biomed Mass Spectrom 5: 198-207, 1978. 106. Roe CR, Sweetman L, Roe DS, David F and Brunengraber H. Treatment of cardiomyopathy and rhabdomyolysis in long-chain fat oxidation disorders using an anaplerotic odd-chain triglyceride. J Clin Invest 110: 259-269, 2002. 107. Diedrich M and Henschel K.P. The natural occurrence of unusual fatty acids. 1. Odd numbered fatty acids. Nahrung 34: 935-943, 1990. 108. Vlaeminck B, Fievez V, Tamminga S, Dewhurst RJ, van VA, De BD and Demeyer D. Milk odd- and branched-chain fatty acids in relation to the rumen fermentation pattern. J Dairy Sci 89: 3954-3964, 2006. 168 109. Vlaeminck B, Dufour C, van Vuuren AM, Cabrita AR, Dewhurst RJ, Demeyer D and Fievez V. Use of odd and branched-chain fatty acids in rumen contents and milk as a potential microbial marker. J Dairy Sci 88: 1031-1042, 2005. 110. Keneda T. Iso- and anteiso-fatty acids in bacteria: biosynthesis, function, and taxonomic significance. Microbiol rev 55: 288-302, 91 A.D. 111. Baker FC and Schooley DA. Biosynthesis of 3-hydroxy-3-methylglutarylCoA, 3-hydroxy-3-ethylglutaryl-CoA, mevalonate and homomevalonate by insect corpus allatum and mammalian hepatic tissues. Biochim Biophys Acta 664: 356-372, 1981. 112. Bergmeyer HU, Gawehn K, Klotzsch H, Krebs HA and Williamson DH. Purification and properties of crystalline 3-hydroxybutyrate dehydrogenase from Rhodopseudomonas spheroides. Biochem J 102: 423-431, 1967. 113. Kuhara T, Inoue Y, Shinka T, Matsumoto I and Matsuo M. Identification of 3-hydroxy-3-ethylglutaric acid in urine of patients with propionic acidaemia. Biomed Mass Spectrom 10: 629-632, 1983. 114. Duran M, Gompertz D, Bruinvis L, Ketting D and Wadman SK. The variability of metabolite excretion in propionicacidaemia. Clin Chim Acta 82: 93-99, 1978. 115. Hommes FA, Kuipers JR, Elema JD, Jansen JF and Jonxis JH. Propionicacidemia, a new inborn error of metabolism. Pediatr Res 2: 519524, 1968. 169 116. Green DE, Dewan JG and Leloir LF. The beta-hydroxybutyric dehydrogenase of animal tissues. Biochem J 31: 934-949, 1937. 117. Fenselau A and Wallis K. Comparative studies on 3-oxo acid coenzyme A transferase from various rat tissues. Biochem J 142: 619-627, 1974. 118. Middleton B. The oxoacyl-coenzyme A thiolases of animal tissues. Biochem J 132: 717-730, 1973. 119. Buckley BM and Williamson DH. Acetoacetate and brain lipogenesis: developmental pattern of acetoacetyl-coenzyme A synthetase in the soluble fraction of rat brain. Biochem J 132: 653-656, 1973. 120. Tildon JT and Sevdalian DA. CoA transferase in the brain and other mammalian tissues. Arch Biochem Biophys 148: 382-390, 1972. 121. Lincoln BC, Des Rosiers C and Brunengraber H. Metabolism of S-3hydroxybutyrate in the perfused rat liver. Arch Biochem Biophys 259: 149156, 1987. 122. Seccombe DW, Harding PG and Possmayer F. Fetal utilization of maternally derived ketone bodies for lipogenesis in the rat. Biochim Biophys Acta 488: 402-416, 1977. 123. Paterson P, Sheath J, Taft P and Wood C. Maternal and foetal ketone concentrations in plasma and urine. Lancet 1: 862-865, 1967. 124. Cheng KK and Yang MM. Study of pregnancy ketosis in the rat. Q J Exp Physiol Cogn Med Sci 55: 83-92, 1970. 170 125. Shambaugh GE, Mrozak SC and Freinkel N. Fetal fuels. I. Utilization of ketones by isolated tissues at various stages of maturation and maternal nutrition during late gestation. Metabolism 26: 623-635, 1977. 126. Shambaugh GE, III, Koehler RR and Yokoo H. Fetal fuels. III: Ketone utilization by fetal hepatocyte. Am J Physiol 235: E330-E337, 1978. 127. Siesjo BK. In: Brain energy metabolism. New York: Wiley 70: 101-125, 1978. 128. Sokoloff L. Metabolism of ketone bodies by the brain. Annu Rev Med 24: 271-280, 1973. 129. Vannucci SJ and Simpson IA. Developmental switch in brain nutrient transporter expression in the rat. Am J Physiol Endocrinol Metab 285: E1127-E1134, 2003. 130. Nebeling LC and Lerner E. Implementing a ketogenic diet based on medium-chain triglyceride oil in pediatric patients with cancer. J Am Diet Assoc 95: 693-697, 1995. 131. Nehlig A and Pereira d, V. Glucose and ketone body utilization by the brain of neonatal rats. Prog Neurobiol 40: 163-221, 1993. 132. Veech RL, Chance B, Kashiwaya Y, Lardy HA and Cahill GF, Jr. Ketone bodies, potential therapeutic uses. IUBMB Life 51: 241-247, 2001. 133. Enerson BE and Drewes LR. Molecular features, regulation, and function of monocarboxylate transporters: implications for drug delivery. J Pharm Sci 92: 1531-1544, 2003. 171 134. Gerhart DZ, Enerson BE, Zhdankina OY, Leino RL and Drewes LR. Expression of monocarboxylate transporter MCT1 by brain endothelium and glia in adult and suckling rats. Am J Physiol 273: E207-E213, 1997. 135. Leino RL, Gerhart DZ, Duelli R, Enerson BE and Drewes LR. Dietinduced ketosis increases monocarboxylate transporter (MCT1) levels in rat brain. Neurochem Int 38: 519-527, 2001. 136. Puchowicz MA, Xu K, Sun X, Ivy A, Emancipator D and LaManna JC. Diet-induced ketosis increases capillary density without altered blood flow in rat brain. Am J Physiol Endocrinol Metab 292: E1607-E1615, 2007. 137. Dahlquist G, Persson U and Persson B. The activity of D- hydroxybutyrate dehydrogenase in fetal, infant and adult rat brain and the influence of starvation. Biol Neonate 20: 40-50, 1972. 138. Daniel PM, Love ER, Moorhouse SR and Pratt OE. The transport of ketone bodies into the brain of the rat (in vivo). J Neurol Sci 34: 1-13, 1977. 139. Yeh YY, Streuli VL and Zee P. Ketone bodies serve as important precursors of brain lipids in the developing rat. Lipids 12: 957-964, 1977. 140. Cremer JE, Teal HM and Cunningham VJ. Inhibition, by 2-oxo acids that accumulate in maple-syrup-urine disease, of lactate, pyruvate, and 3hydroxybutyrate transport across the blood-brain barrier. J Neurochem 39: 674-677, 1982. 141. Schroeder H, Bomont L and Nehlig A. Influence of early chronic phenobarbital treatment on cerebral arteriovenous differences of glucose 172 and ketone bodies in the developing rat. Int J Dev Neurosci 9: 453-461, 1991. 142. Dysza HA, Czajka DM and Miller SA. Influence of artifical diet on weight gain and body composition of the neonatal rat. J Nutr 84: 100-106, 1964. 143. Lopes-Cardozo M and Klein W. Ketone-body utilization and lipid synthesis by developing rat brain-a comparison between in vivo and in vitro experiments. Neurochem Int 6: 459-466, 1984. 144. Yeh YY and Sheehan PM. Preferential utilization of ketone bodies in the brain and lung of newborn rats. Fed Proc 44: 2352-2358, 1985. 145. Hawkins RA and Williamson DH. Measurements of substrate uptake by mammary gland of the rat. Biochem J 129: 1171-1173, 1972. 146. Bernard L, Leroux C and Chilliard Y. Expression and nutritional regulation of lipogenic genes in the ruminant lactating mammary gland. Adv Exp Med Biol 606: 67-108, 2008. 147. Williamson DH, McKeown SR and Ilic V. Interactions of glucose, acetoacetate and insulin in mammary-gland slices of lactating rats. Biochem J 150: 145-152, 1975. 148. Bartley JC. Modulation by ketone bodies of the rate of fatty acid synthesis in mammary gland slices from lactating rats. Lipids 11: 774-777, 1976. 149. Angielski S and Lukowicz J. The role of the kidney in the removal of ketone bodies under different acid-base status of the rat. Am J Clin Nutr 31: 1635-1641, 1978. 173 150. Sapir DG and Owen OE. Renal conservation of ketone bodies during starvation. Metabolism 24: 23-33, 1975. 151. Randle PJ, Newsholme EA and Garland PB. Regulation of glucose uptake by muscle. 8. Effects of fatty acids, ketone bodies and pyruvate, and of alloxan-diabetes and starvation, on the uptake and metabolic fate of glucose in rat heart and diaphragm muscles. Biochem J 93: 652-665, 1964. 152. Hall LM. Preferential oxidation of acetoacetate by the perfused heart. Biochem Biophys Res Commun 6: 177-179, 1961. 153. Sherwin RS, Hendler RG and Felig P. Effect of diabetes mellitus and insulin on the turnover and metabolic response to ketones in man. Diabetes 25: 776-784, 1976. 154. Garber AJ, Menzel PH, Boden G and Owen OE. Hepatic ketogenesis and gluconeogenesis in humans. J Clin Invest 54: 981-989, 1974. 155. Keller U, Sonnenberg GE and Stauffacher W. Validation of a tracer technique to determine nonsteady-state ketone body turnover rates in man. Am J Physiol 240: E253-E262, 1981. 156. Bougneres PF, Balasse EO, Ferre P and Bier DM. Determination of ketone body kinetics using a D-(-)-3-hydroxy[4,4,4-2H3]butyrate tracer. J Lipid Res 27: 215-220, 1986. 157. Balasse EO. Kinetics of ketone body metabolism in fasting humans. Metabolism 28: 41-50, 1979. 174 158. McGarry JD, Guest MJ and Foster DW. Ketone body metabolism in the ketosis of starvation and alloxan diabetes. J Biol Chem 245: 4382-4390, 1970. 159. Barton RN. Isotopic study of ketone body kinetics: invalidity of calculations based upon specific radioactivity of total ketone bodies. Metabolism 29: 392-396, 1980. 160. Wolfe BM, Havel JR, Marliss EB, Kane JP, Seymour J and Ahuja SP. Effects of a 3-day fast and of ethanol on splanchnic metabolism of FFA, amino acids, and carbohydrates in healthy young men. J Clin Invest 57: 329-340, 1976. 161. Reed WD, Baab PJ, Hawkins RL and Ozand PT. A double-isotope method for the measurement of ketone-body turnover in the rat. Effect of L-alanine. Biochem J 219: 15-24, 1984. 162. Miles JM, Schwenk WF, McClean KL and Haymond MW. A dualisotope technique for determination of in vivo ketone body kinetics. Am J Physiol 251: E185-E191, 1986. 163. Fink G, Desrochers S, Des Rosiers C, Garneau M, David F, Daloze T, Landau BR and Brunengraber H. Pseudoketogenesis in the perfused rat heart. J Biol Chem 263: 18036-18042, 1988. 164. Des Rosiers C, Montgomery JA, Desrochers S, Garneau M, David F, Mamer OA and Brunengraber H. Interference of 3-hydroxyisobutyrate with measurements of ketone body concentration and isotopic enrichment 175 by gas chromatography-mass spectrometry. Anal Biochem 173: 96-105, 1988. 165. Des Rosiers C, Montgomery JA, Garneau M, David F, Mamer OA, Daloze P, Toffolo G, Cobelli C, Landau BR and Brunengraber H. Pseudoketogenesis in hepatectomized dogs. Am J Physiol 258: E519E528, 1990. 166. Brunengraber H and Roe CR. Anaplerotic molecules: current and future. J Inherit Metab Dis 29: 327-331, 2006. 167. Owen OE, Kalhan SC and Hanson RW. The key role of anaplerosis and cataplerosis for citric acid cycle function. J Biol Chem 277: 30409-30412, 2002. 168. Ballard FJ, Hanson RW and Leveille GA. Phosphoenolpyruvate carboxykinase and the synthesis of glyceride-glycerol from pyruvate in adipose tissue. J Biol Chem 242: 2746-2750, 1967. 169. Brunengraber H, Boutry M and Lowenstein JM. Fatty acid and 3- hydroxysterol synthesis in the perfused rat liver. Including measurements on the production of lactate, pyruvate, -hydroxy-butyrate, and acetoacetate by the fed liver. J Biol Chem 248: 2656-2669, 1973. 170. Hassel B. Pyruvate carboxylation in neurons. J Neurosci Res 66: 755762, 2001. 171. Bing RJ. The metabolism of the heart. Trans Am Coll Cardiol 5: 8-14, 1955. 176 172. Taegtmeyer H, Hems R and Krebs HA. Utilization of energy-providing substrates in the isolated working rat heart. Biochem J 186: 701-711, 1980. 173. Gibala MJ, Young ME and Taegtmeyer H. Anaplerosis of the citric acid cycle: role in energy metabolism of heart and skeletal muscle. Acta Physiol Scand 168: 657-665, 2000. 174. Boucher A, Lu D, Burgess SC, Telemaque-Potts S, Jensen MV, Mulder H, Wang MY, Unger RH, Sherry AD and Newgard CB. Biochemical mechanism of lipid-induced impairment of glucose-stimulated insulin secretion and reversal with a malate analogue. J Biol Chem 279: 27263-27271, 2004. 175. Zoppi CC, Silveira LR, Oliveira CA, Boschero AC, Curi R and Carneiro EM. Insulin release, peripheral insulin resistance and muscle function in protein malnutrition: a role of tricarboxylic acid cycle anaplerosis. Br J Nutr 103: 1237-1250, 2010. 176. Utter MF and Keech DB. Formation of oxaloacetate from pyruvate and carbon dioxide. J Biol Chem 235: C17-C18, 1960. 177. Mackall JC and Lane MD. Role of pyruvate carboxylase in fatty acid synthesis: alterations during preadipocyte differentiation. Biochem Biophys Res Commun 79: 720-725, 1977. 178. Cooper AJ and Plum F. Biochemistry and physiology of brain ammonia. Physiol Rev 67: 440-519, 1987. 177 179. MacDonald MJ. Feasibility of a mitochondrial pyruvate malate shuttle in pancreatic islets. Further implication of cytosolic NADPH in insulin secretion. J Biol Chem 270: 20051-20058, 1995. 180. Hasan NM, Longacre MJ, Stoker SW, Boonsaen T, Jitrapakdee S, Kendrick MA, Wallace JC and MacDonald MJ. Impaired anaplerosis and insulin secretion in insulinoma cells caused by small interfering RNAmediated suppression of pyruvate carboxylase. J Biol Chem 283: 2804828059, 2008. 181. Russell RR, III and Taegtmeyer H. Pyruvate carboxylation prevents the decline in contractile function of rat hearts oxidizing acetoacetate. Am J Physiol 261: H1756-H1762, 1991. 182. Pound KM, Sorokina N, Ballal K, Berkich DA, Fasano M, Lanoue KF, Taegtmeyer H, O'Donnell JM and Lewandowski ED. Substrate-enzyme competition attenuates upregulated anaplerotic flux through malic enzyme in hypertrophied rat heart and restores triacylglyceride content: attenuating upregulated anaplerosis in hypertrophy. Circ Res 104: 805-812, 2009. 183. Panchal AR, Comte B, Huang H, Kerwin T, Darvish A, Des Rosiers C, Brunengraber H and Stanley WC. Partitioning of pyruvate between oxidation and anaplerosis in swine hearts. Am J Physiol Heart Circ Physiol 279: H2390-H2398, 2000. 184. Xu J, Han J, Long YS, Epstein PN and Liu YQ. The role of pyruvate carboxylase in insulin secretion and proliferation in rat pancreatic beta cells. Diabetologia 51: 2022-2030, 2008. 178 185. Bunger R, Swindall B, Brodie D, Zdunek D, Stiegler H and Walter G. Pyruvate attenuation of hypoxia damage in isolated working guinea-pig heart. J Mol Cell Cardiol 18: 423-438, 1986. 186. Stanley WC, Kivilo KM, Panchal AR, Hallowell PH, Bomont C, Kasumov T and Brunengraber H. Post-ischemic treatment with dipyruvyl-acetyl-glycerol decreases myocardial infarct size in the pig. Cardiovasc Drugs Ther 17: 209-216, 2003. 187. Fransson U, Rosengren AH, Schuit FC, Renstrom E and Mulder H. Anaplerosis via pyruvate carboxylase is required for the fuel-induced rise in the ATP:ADP ratio in rat pancreatic islets. Diabetologia 49: 1578-1586, 2006. 188. Constantin-Teodosiu D, Simpson EJ and Greenhaff PL. The importance of pyruvate availability to PDC activation and anaplerosis in human skeletal muscle. Am J Physiol 276: E472-E478, 1999. 189. Ahmed A, Maxwell DL, Taylor PM and Rennie MJ. Glutamine transport in human skeletal muscle. Am J Physiol 264: E993-1000, 1993. 190. Bruce M, Constantin-Teodosiu D, Greenhaff PL, Boobis LH, Williams C and Bowtell JL. Glutamine supplementation promotes anaplerosis but not oxidative energy delivery in human skeletal muscle. Am J Physiol Endocrinol Metab 280: E669-E675, 2001. 191. Rennie MJ, Bowtell JL, Bruce M and Khogali SE. Interaction between glutamine availability and metabolism of glycogen, tricarboxylic acid cycle intermediates and glutathione. J Nutr 131: 2488S-2490S, 2001. 179 192. Kasumov T, Cendrowski AV, David F, Jobbins KA, Anderson VE and Brunengraber H. Mass isotopomer study of anaplerosis from propionate in the perfused rat heart. Arch Biochem Biophys 463: 110-117, 2007. 193. Sherry AD, Malloy CR, Roby RE, Rajagopal A and Jeffrey FM. Propionate metabolism in the rat heart by 13C n.m.r. spectroscopy. Biochem J 254: 593-598, 1988. 194. Martini WZ, Stanley WC, Huang H, Rosiers CD, Hoppel CL and Brunengraber H. Quantitative assessment of anaplerosis from propionate in pig heart in vivo. Am J Physiol Endocrinol Metab 284: E351-E356, 2003. 195. Comte B, Vincent G, Bouchard B and and Des Rosiers C. Probing the origin of acetyl-CoA and oxaloacetate entering the citric acid cycle from the 13C labeling of citrate released by perfused rat hearts. J Biol Chem 272: 26117-26124, 1997. 196. Roe DS, Vianey-Saban C, Sharma S, Zabot MT and Roe CR. Oxidation of unsaturated fatty acids by human fibroblasts with very-long-chain acylCoA dehydrogenase deficiency: aspects of substrate specificity and correlation with clinical phenotype. Clin Chim Acta 312: 55-67, 2001. 197. Mochel F, DeLonlay P, Touati G, Brunengraber H, Kinman RP, Rabier D, Roe CR and Saudubray JM. Pyruvate carboxylase deficiency: clinical and biochemical response to anaplerotic diet therapy. Mol Genet Metab 84: 305-312, 2005. 180 198. Tozzi MG, Camici M, Mascia L, Sgarrella F and Ipata PL. Pentose phosphates in nucleoside interconversion and catabolism. FEBS J 273: 1089-1101, 2006. 199. Sonne JC, Lin I and Buchanan JM. Biosynthesis of the purines. IX. Precursors of the nitrogen atoms of the purine ring. J Biol Chem 220: 369378, 1956. 200. Hartman SC and Buchanan JM. The biosynthesis of the purines. Ergeb Physiol 50: 75-121, 1959. 201. Chen S, Turner S, Tsang E, Stark J, Turner H, Mahsut A, Keifer K, Goldfinger M and Hellerstein MK. Measurement of pancreatic islet cell proliferation by heavy water labeling. Am J Physiol Endocrinol Metab 293: E1459-E1464, 2007. 202. Tullson PC, John-Alder HB, Hood DA and Terjung RL. De novo synthesis of adenine nucleotides in different skeletal muscle fiber types. Am J Physiol 255: C271-C277, 1988. 203. Dow JW, Nigdikar S and Bowditch J. Adenine nucleotide synthesis de novo in mature rat cardiac myocytes. Biochim Biophys Acta 847: 223-227, 1985. 204. Zimmer HG, Steinkopff G and Gerlach E. [Studies on regulation of denovo synthesis of adenine nucleotides in the heart]. Verh Dtsch Ges Kreislaufforsch 40: 348-352, 1974. 205. Zimmer HG and Gerlach E. Stimulation of myocardial adenine nucleotide biosynthesis by pentoses and pentitols. Pflugers Arch 376: 223-227, 1978. 181 206. Smellie RM, Thomson RY and Davidson JN. The nucleic acid metabolism of animal cells in vitro. I. The incorporation of 14C-formate. Biochim Biophys Acta 29: 59-74, 1958. 207. Scott JL. Human leukocyte metabolism in vitro. I. Incorporation of adenine-8-C-14 and formate-C-14 into the nucleic acids of leukemic leukocytes. J Clin Invest 41: 67-79, 1962. 208. Holmsen H and Rozenberg MC. Adenine nucleotide metabolism of blood platelets. 3. Adenine phosphoribosyl transferase and nucleotide formation from exogenous adenine. Biochim Biophys Acta 157: 266-279, 1968. 209. Wyngaarden JB. The metabolic basis of inherited disease. New York: McGraw 1: 1-7, 1966. 210. Manfredi JP and Holmes EW. Purine salvage pathways in myocardium. Annu Rev Physiol 47: 691-705, 1985. 211. Kim YA, King MT, Teague WE, Jr., Rufo GA, Jr., Veech RL and Passonneau JV. Regulation of the purine salvage pathway in rat liver. Am J Physiol 262: E344-E352, 1992. 212. Murray AW. The biological significance of purine salvage. Annu Rev Biochem 40: 811-826, 1971. 213. Namm DH. Myocardial nucleotide synthesis from purine bases and nucleosides. Comparison of the rates of formation of purine nucleotides from various precursors and identification of the enzymatic routes for nucleotide formation in the isolated rat heart. Circ Res 33: 686-695, 1973. 182 214. Kelley WN, Rosenbloom FM and Seegmiller JE. The effects of azathioprine (imuran) on purine synthesis in clinical disorders of purine metabolism. J Clin Invest 46: 1518-1529, 1967. 215. Lesch M and Nyhan WL. A familial disorder of uric acid metabolism and central nervous system function. Am J Med 36: 561-570, 1964. 216. Rosenbloom FM, Kelley WN, Miller J, Henderson JF and Seegmiller JE. Inherited disorder of purine metabolism. Correlation between central nervous system dysfunction and biochemical defects. JAMA 202: 175177, 1967. 217. Lipmann F. Enzymatic acetylation and the coenzyme of acetylation. Biol Bull 91: 239, 1946. 218. Leonardi R, Zhang YM, Rock CO and Jackowski S. Coenzyme A: back in action. Prog Lipid Res 44: 125-153, 2005. 219. Spry C, Kirk K and Saliba KJ. Coenzyme A biosynthesis: an antimicrobial drug target. FEMS Microbiol Rev 32: 56-106, 2008. 220. Tahiliani AG and Neely JR. Mitochondrial synthesis of coenzyme A is on the external surface. J Mol Cell Cardiol 19: 1161-1167, 1987. 221. Basu SS, Mesaros C, Gelhaus SL and Blair IA. Stable isotope labeling by essential nutrients in cell culture for preparation of labeled coenzyme A and its thioesters. Anal Chem 83: 1363-1369, 2011. 222. Reibel DK, Wyse BW, Berkich DA, Palko WM and Neely JR. Effects of diabetes and fasting on pantothenic acid metabolism in rats. Am J Physiol 240: E597-E601, 1981. 183 223. Horie S, Isobe M and Suga T. Changes in CoA pools in hepatic peroxisomes of the rat under various conditions. J Biochem 99: 13451352, 1986. 224. Lopaschuk GD and Neely JR. Stimulation of myocardial coenzyme A degradation by fatty acids. Am J Physiol 253: H41-H46, 1987. 225. Snell EE and Mitchell HK. Growth inhibition by N-(dihydroxydimethylbutyryl)taurine and its reversal by pantothenic aicd. J Biol Chem 141: 121-128, 1941. 226. McIlwain H and Hawking F. Chemotherapy of blocking bacterial nutrients Antistreptococcal activity of pantoyltaurine. Lancet 241: 449-451, 1943. 227. Reichard P. Interactions between deoxyribonucleotide and DNA synthesis. Annu Rev Biochem 57: 349-374, 1988. 228. Skoog L. An enzymatic method for the determination of dCTP and dGTP in picomole amounts. Eur J Biochem 17: 202-208, 1970. 229. Walters RA, Tobey RA and Ratliff RL. Cell-cycle-dependent variations of deoxyribonucleoside triphosphate pools in Chinese hamster cells. Biochim Biophys Acta 319: 336-347, 1973. 230. Skoog KL, Nordenskjold BA and Bjursell KG. Deoxyribonucleosidetriphosphate pools and DNA synthesis in synchronized hamster cells. Eur J Biochem 33: 428-432, 1973. 231. Newman CN and Miller JH. Mechanism of UV-induced deoxynucleoside triphosphate pool imbalance in CHO-K1 cells. Mutat Res 145: 95-101, 1985. 184 232. Das SK and Berger NA. Alterations in deoxynucleoside triphosphate metabolism in DNA damaged cells: identification and consequences of poly(ADP-ribose) polymerase dependent and independent processes. Biochem Biophys Res Commun 137: 1153-1158, 1986. 233. Cohen SS and Barner HD. STUDIES ON UNBALANCED GROWTH IN ESCHERICHIA COLI. Proc Natl Acad Sci U S A 40: 885-893, 1954. 234. Ayusawa D, Koyama H, Shimizu K, Kaneda S, Takeishi K and Seno T. Induction, by thymidylate stress, of genetic recombination as evidenced by deletion of a transferred genetic marker in mouse FM3A cells. Mol Cell Biol 6: 3463-3469, 1986. 235. Martin DW, Jr. and Gelfand EW. Biochemistry of diseases of immunodevelopment. Annu Rev Biochem 50: 845-877, 1981. 236. Janssen AJ, Trijbels FJ, Sengers RC, Wintjes LT, Ruitenbeek W, Smeitink JA, Morava E, van Engelen BG, van den Heuvel LP and Rodenburg RJ. Measurement of the energy-generating capacity of human muscle mitochondria: diagnostic procedure and application to human pathology. Clin Chem 52: 860-871, 2006. 237. Hara KY and Mori H. An efficient method for quantitative determination of cellular ATP synthetic activity. J Biomol Screen 11: 310-317, 2006. 238. Lemasters JJ and Hackenbrock CR. Continuous measurement and rapid kinetics of ATP synthesis in rat liver mitochondria, mitoplasts and inner membrane vesicles determined by firefly-luciferase luminescence. Eur J Biochem 67: 1-10, 1976. 185 239. Drew B and Leeuwenburgh C. Method for measuring ATP production in isolated mitochondria: ATP production in brain and liver mitochondria of Fischer-344 rats with age and caloric restriction. Am J Physiol Regul Integr Comp Physiol 285: R1259-R1267, 2003. 240. Szendroedi J, Schmid AI, Chmelik M, Toth C, Brehm A, Krssak M, Nowotny P, Wolzt M, Waldhausl W and Roden M. Muscle mitochondrial ATP synthesis and glucose transport/phosphorylation in type 2 diabetes. PLoS Med 4: e154, 2007. 241. Walter G, Vandenborne K, McCully KK and Leigh JS. Noninvasive measurement of phosphocreatine recovery kinetics in single human muscles. Am J Physiol 272: C525-C534, 1997. 242. Pedersen BL, Arendrup H, Secher NH and Quistorff B. Metabolism of perfused pig intercostal muscles evaluated by 31P-magnetic resonance spectroscopy. Exp Physiol 91: 755-763, 2006. 243. Reibel DK, Wyse BW, Berkich DA and Neely JR. Regulation of coenzyme A synthesis in heart muscle: effects of diabetes and fasting. Am J Physiol 240: H606-H611, 1981. 244. Robishaw JD, Berkich D and Neely JR. Rate-limiting step and control of coenzyme A synthesis in cardiac muscle. J Biol Chem 257: 10967-10972, 1982. 245. Robishaw JD and Neely JR. Pantothenate kinase and control of CoA synthesis in heart. Am J Physiol 246: H532-H541, 1984. 186 246. Beinlich CJ, Robishaw JD and Neely JR. Metabolism of pantothenic acid in hearts of diabetic rats. J Mol Cell Cardiol 21: 641-649, 1989. 247. Taupin P. BrdU immunohistochemistry for studying adult neurogenesis: paradigms, pitfalls, limitations, and validation. Brain Res Rev 53: 198-214, 2007. 248. Taupin P. Protocols for studying adult neurogenesis: insights and recent developments. Regen Med 2: 51-62, 2007. 249. Gratzner HG. Monoclonal antibody to 5-bromo- and 5-iododeoxyuridine: A new reagent for detection of DNA replication. Science 218: 474-475, 1982. 250. Nagao T, Kuwagata M and Saito Y. Effects of prenatal exposure to 5bromo-2'-deoxyuridine on the developing brain and reproductive function in male mouse offspring. Reprod Toxicol 12: 477-487, 1998. 251. Asher E, Payne CM and Bernstein C. Evaluation of cell death in EBVtransformed lymphocytes using agarose gel electrophoresis, light microscopy and electron microscopy. II. Induction of non-classic apoptosis ("para-apoptosis") by tritiated thymidine. Leuk Lymphoma 19: 107-119, 1995. 252. Rocha B, Penit C, Baron C, Vasseur F, Dautigny N and Freitas AA. Accumulation of bromodeoxyuridine-labeled cells in central and peripheral lymphoid organs: minimal estimates of production and turnover rates of mature lymphocytes. Eur J Immunol 20: 1697-1708, 1990. 253. Schoenheimer R and Rittenberg D. Deuterium as an indicator in the study of intermediary metabolism. Science 82: 156-157, 1935. 187 254. Dufner D and Previs SF. Measuring in vivo metabolism using heavy water. Curr Opin Clin Nutr Metab Care 6: 511-517, 2003. 255. Dufner DA, Bederman IR, Brunengraber DZ, Rachdaoui N, IsmailBeigi F, Siegfried BA, Kimball SR and Previs SF. Using 2H2O to study the influence of feeding on protein synthesis: effect of isotope equilibration in vivo vs. in cell culture. Am J Physiol Endocrinol Metab 288: E1277E1283, 2005. 256. Busch R, Neese RA, Awada M, Hayes GM and Hellerstein MK. Measurement of cell proliferation by heavy water labeling. Nat Protoc 2: 3045-3057, 2007. 257. Cook PF, Blanchard JS and Cleland WW. Primary and secondary deuterium isotope effects on equilibrium constants for enzyme-catalyzed reactions. Biochemistry 19: 4853-4858, 1980. 258. Billeter SR, Webb SP, Agarwal PK, Iordanov T and Hammes-Schiffer S. Hydride transfer in liver alcohol dehydrogenase: quantum dynamics, kinetic isotope effects, and role of enzyme motion. J Am Chem Soc 123: 11262-11272, 2001. 259. Levy LM and Betts GF. Stereospecificity of C4 nicotinamide hydrogen transfer of the NADP-dependent glyceraldehyde-3-phosphate dehydrogenase. Biochim Biophys Acta 997: 331-333, 1989. 260. Babu UM and Johnston RB. D2O-alanine exchange reactions catalyzed by alanine racemase and glutamic pyruvic transminase. Biochem Biophys Res Commun 58: 460-466, 1974. 188 261. Bock G, Schumann WC, Basu R, Burgess SC, Yan Z, Chandramouli V, Rizza RA and Landau BR. Evidence that processes other than gluconeogenesis may influence the ratio of deuterium on the fifth and third carbons of glucose: implications for the use of 2H2O to measure gluconeogenesis in humans. Diabetes 57: 50-55, 2008. 262. Belenky P, Bogan KL and Brenner C. NAD+ metabolism in health and disease. Trends Biochem Sci 32: 12-19, 2007. 263. Lee WN, Boros LG, Puigjaner J, Bassilian S, Lim S and Cascante M. Mass isotopomer study of the nonoxidative pathways of the pentose cycle with [1,2-13C2]glucose. Am J Physiol 274: E843-E851, 1998. 264. Brunengraber H, Sabine JR, Boutry M and Lowenstein JM. 3- Hydroxysterol synthesis by the liver. Arch Biochem Biophys 150: 392-396, 1972. 265. Previs SF, Fatica R, Chandramouli V, Alexander JC, Brunengraber H and Landau BR. Quantifying rates of protein synthesis in humans by use of 2H2O: application to patients with end-stage renal disease. Am J Physiol Endocrinol Metab 286: E665-E672, 2004. 266. Neese RA, Misell LM, Turner S, Chu A, Kim J, Cesar D, Hoh R, Antelo F, Strawford A, McCune JM, Christiansen M and Hellerstein MK. Measurement in vivo of proliferation rates of slow turnover cells by 2H2O labeling of the deoxyribose moiety of DNA. Proc Natl Acad Sci U S A 99: 15345-15350, 2002. 189 267. Varady KA, Hudak CS and Hellerstein MK. Modified alternate-day fasting and cardioprotection: relation to adipose tissue dynamics and dietary fat intake. Metabolism 58: 803-811, 2009. 268. Busch R, Kim YK, Neese RA, Schade-Serin V, Collins M, Awada M, Gardner JL, Beysen C, Marino ME, Misell LM and Hellerstein MK. Measurement of protein turnover rates by heavy water labeling of nonessential amino acids. Biochim Biophys Acta 1760: 730-744, 2006. 269. Schoenheimer R. The Investigation of Intermediary Metabolism with the Aid of Heavy Hydrogen: Harvey Lecture, January 21, 1937. Bull N Y Acad Med 13: 272-295, 1937. 270. GUTMAN A and SHAFRIR E. Metabolic influences on enzymes of glycogen synthesis and breakdown in adipose tissue. Am J Physiol 207: 1215-1220, 1964. 271. Lee WN, Bassilian S, Ajie HO, Schoeller DA, Edmond J, Bergner EA and Byerley LO. In vivo measurement of fatty acids and cholesterol synthesis using D2O and mass isotopomer analysis. Am J Physiol 266: E699-E708, 1994. 272. Jungas RL. Fatty acid synthesis in adipose tissue incubated in tritiated water. Biochemistry 7: 3708-3717, 1968. 273. Wadke M, Brunengraber H, Lowenstein JM, Dolhun JJ and Arsenault GP. Fatty acid synthesis by liver perfused with deuterated and tritiated water. Biochemistry 12: 2619-2624, 1973. 190 274. Diraison F, Pachiaudi C and Beylot M. Measuring lipogenesis and cholesterol synthesis in humans with deuterated water: use of simple gas chromatographic/mass spectrometric techniques. J Mass Spectrom 32: 81-86, 1997. 275. Ussing HH. The rate of protein renewal in mice and rats studied by means of heavy hydrogen. Acta Physiol Scand 2: 209-221, 1941. 276. Yuan CL, Sharma N, Gilge DA, Stanley WC, Li Y, Hatzoglou M and Previs SF. Preserved protein synthesis in the heart in response to acute fasting and chronic food restriction despite reductions in liver and skeletal muscle. Am J Physiol Endocrinol Metab 295: E216-E222, 2008. 277. Neese RA, Siler SQ, Cesar D, Antelo F, Lee D, Misell L, Patel K, Tehrani S, Shah P and Hellerstein MK. Advances in the stable isotopemass spectrometric measurement of DNA synthesis and cell proliferation. Anal Biochem 298: 189-195, 2001. 278. McCune JM, Hanley MB, Cesar D, Halvorsen R, Hoh R, Schmidt D, Wieder E, Deeks S, Siler S, Neese R and Hellerstein M. Factors influencing T-cell turnover in HIV-1-seropositive patients. J Clin Invest 105: R1-R8, 2000. 279. Kim SJ, Cheung S and Hellerstein MK. Isolation of nuclei from labelretaining cells and measurement of their turnover rates in rat colon. Am J Physiol Cell Physiol 286: C1464-C1473, 2004. 280. Hayes GM, Busch R, Voogt J, Siah IM, Gee TA, Hellerstein MK, Chiorazzi N, Rai KR and Murphy EJ. Isolation of malignant B cells from 191 patients with chronic lymphocytic leukemia (CLL) for analysis of cell proliferation: validation of a simplified method suitable for multi-center clinical studies. Leuk Res 34: 809-815, 2010. 281. Kim SJ, Turner S, Killion S and Hellerstein MK. In vivo measurement of DNA synthesis rates of colon epithelial cells in carcinogenesis. Biochem Biophys Res Commun 331: 203-209, 2005. 282. Turner SM, Linfoot PA, Neese RA and Hellerstein MK. Sources of plasma glucose and liver glycogen in fasted ob/ob mice. Acta Diabetol 42: 187-193, 2005. 283. Kim J, Choi YL, Vallentin A, Hunrichs BS, Hellerstein MK, Peehl DM and Mochly-Rosen D. Centrosomal PKCbetaII and pericentrin are critical for human prostate cancer growth and angiogenesis. Cancer Res 68: 6831-6839, 2008. 284. Gillingham MB, Connor WE, Matern D, Rinaldo P, Burlingame T, Meeuws K and Harding CO. Optimal dietary therapy of long-chain 3hydroxyacyl-CoA dehydrogenase deficiency. Mol Genet Metab 79: 114123, 2003. 285. Landau BR, Wahren J, Chandramouli V, Schumann WC, Ekberg K and Kalhan SC. Contributions of gluconeogenesis to glucose production in the fasted state. J Clin Invest 98: 378-385, 1996. 286. Wang B, Sun G, Anderson DR, Jia M, Previs S and Anderson VE. Isotopologue distributions of peptide product ions by tandem mass 192 spectrometry: quantitation of low levels of deuterium incorporation. Anal Biochem 367: 40-48, 2007. 287. Voogt JN, Awada M, Murphy EJ, Hayes GM, Busch R and Hellerstein MK. Measurement of very low rates of cell proliferation by heavy water labeling of DNA and gas chromatography/pyrolysis/isotope ratio-mass spectrometric analysis. Nat Protoc 2: 3058-3062, 2007. 288. Exil VJ, Roberts RL, Sims H, McLaughlin JE, Malkin RA, Gardner CD, Ni G, Rottman JN and Strauss AW. Very-long-chain acyl-coenzyme a dehydrogenase deficiency in mice. Circ Res 93: 448-455, 2003. 289. Cox KB, Hamm DA, Millington DS, Matern D, Vockley J, Rinaldo P, Pinkert CA, Rhead WJ, Lindsey JR and Wood PA. Gestational, pathologic and biochemical differences between very long-chain acyl-CoA dehydrogenase deficiency and long-chain acyl-CoA dehydrogenase deficiency in the mouse. Hum Mol Genet 10: 2069-2077, 2001. 290. Kurtz DM, Rinaldo P, Rhead WJ, Tian L, Millington DS, Vockley J, Hamm DA, Brix AE, Lindsey JR, Pinkert CA, O'Brien WE and Wood PA. Targeted disruption of mouse long-chain acyl-CoA dehydrogenase gene reveals crucial roles for fatty acid oxidation. Proc Natl Acad Sci U S A 95: 15592-15597, 1998. 291. Kelly CL and Wood PA. Cloning and characterization of the mouse shortchain acyl-CoA dehydrogenase gene. Mamm Genome 7: 262-264, 1996. 193