* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hematopoietic Function Hematopoietic Function
Survey
Document related concepts
Transcript
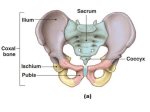
U N I T Hematopoietic Function F rom ancient times, the importance of blood as a determinant of health was recognized. Its life-affecting powers are well described in the written treatises of Greek physician Galen (AD 130–200). Galen, who reigned as the foremost medical authority for nearly 1500 years, believed that an individual stayed healthy as long as four body fluids—blood, phlegm, yellow bile, and black bile—remained in the right proportion. He also believed that the four humors determined one’s basic temperament. Whether an individual was sanguine, sluggish and dull, quick to anger, or melancholy was determined by the degree to which one or another of the humors predominated. The most desirable personality type was achieved when blood was thought to predominate, yielding a warm and cheerful person. The workings of blood were traced by Galen from its creation, which he believed took place in the liver, throughout the body. He came to believe that disease manifested itself if any one of the fluids was in excess or deficient and was carried in the blood. The theory led to bloodletting—the drawing of blood from the vein of a sick person so the disease could flow out with the blood. For many centuries, bloodletting was the standard treatment for a myriad of ills. IV CHAPTER 14 Hematopoietic System Kathryn J. Gaspard COMPOSITION OF BLOOD AND FORMATION OF BLOOD CELLS Plasma Plasma Proteins Blood Cells Erythrocytes Leukocytes Thrombocytes Hematopoiesis Blood Cell Precursors Regulation of Hematopoiesis DIAGNOSTIC TESTS Blood Count Erythrocyte Sedimentation Rate Bone Marrow Aspiration and Biopsy When blood is removed from the circulatory system, it clots. The clot contains the blood cells and fibrin strands formed from the conversion of the plasma protein fibrinogen. It is surrounded by a yellow liquid called serum. Blood that is kept from clotting by the addition of an anticoagulant (e.g., heparin, citrate) and then centrifuged separates into layers (Fig. 14-1). The lower layer (approximately 42% to 47% of the whole-blood volume) contains the erythrocytes, or red blood cells, and is referred to as the hematocrit. The intermediate layer (approximately 1%) containing the leukocytes is white or gray and is called the buffy layer. Above the leukocytes is a thin layer of platelets that is not discernible to the naked eye. The translucent, yellowish fluid that forms on the top of the cells is the plasma, which comprises approximately 55% of the total volume. PLASMA B lood consists of blood cells (i.e., red blood cells, thrombocytes or platelets, and white blood cells) and the plasma in which the cells are suspended. Blood cells have a relatively short life span and must be continually replaced. The generation of blood cells takes place in the hematopoietic (from the Greek haima “blood” and poiesis “making”) system. The hematopoietic system encompasses all of the blood cells and their precursors, the bone marrow where blood cells have their origin, and the lymphoid tissues where some blood cells circulate as they develop and mature. The plasma component of blood carries the cells that transport gases, aid in body defenses, and prevent blood loss. It transports nutrients that are absorbed from the gastrointestinal tract to body cells and delivers the waste products from cellular metabolism to the kidney for elimination; it transports hormones and permits the exchange of chemical messengers; it facilitates the exchange of body heat; and it participates in electrolyte and acid-base balance and the osmotic regulation of body fluids. Plasma is 90% to 91% water by weight, 6.5% to 8% proteins by weight, and 2% other small molecular substances (Table 14-1). PLASMA PROTEINS Composition of Blood and Formation of Blood Cells After completing this section of the chapter, you should be able to meet the following objectives: ✦ Describe the composition of plasma ✦ Name the formed elements of blood and cite their function and life span ✦ Trace the process of hematopoiesis from stem cell to mature blood cell The plasma proteins are the most abundant solutes in plasma. Most proteins are formed in the liver and serve a variety of functions. The major types are albumin, globulins, and fibrinogen. Albumin is the most abundant and makes up approximately 54% of the plasma proteins. It does not diffuse through the vascular endothelium and therefore contributes to plasma osmotic pressure and the maintenance of blood volume (see Chapter 33). Albumin also serves as a carrier for certain substances and acts as a blood buffer. The globulins comprise approximately 38% of plasma proteins. There are three types of globulins: the 3 4 UNIT IV Hematopoietic Function not divide and thus must be continually renewed by the process of hematopoiesis in the bone marrow. Erythrocytes The erythrocytes, or red blood cells, are the most numerous of the formed elements. They are small, biconcave disks with a large surface area and can easily deform in small capillaries. They contain the oxygen-carrying protein, hemoglobin, that functions in the transport of oxygen. The erythrocytes are derived from the myeloid or bone marrow stem cell and live approximately 120 days in the circulation (see Chapter 16). Plasma (55% of whole blood) Buffy coat leukocytes and platelets (<1% of whole blood) Formed elements Erythrocytes (45% of whole blood) Leukocytes The leukocytes, or white blood cells, constitute only 1% of the total blood volume. They originate in the bone marrow and circulate throughout the lymphoid tissues of the body. There they function in the inflammatory and immune processes. They include the granulocytes, the lymphocytes, and the monocytes (Fig. 14-2). Granulocytes. The granulocytes are all phagocytic cells FIGURE 14-1 Layering of blood components in an anticoagulated and centrifuged blood sample. alpha globulins that transport bilirubin and steroids, the beta globulins that transport iron and copper, and the gamma globulins that constitute the antibodies of the immune system. Fibrinogen makes up approximately 7% of the plasma proteins and is converted to fibrin in the clotting process. The remaining 1% of circulating proteins includes hormones, enzymes, complement, and carriers for lipids. BLOOD CELLS The blood cells include the erythrocytes or red blood cells, the leukocytes or white blood cells, and platelets (Table 14-2). The blood cells, or formed elements, are not all true cells, and most survive for only a few days in the circulation or tissues as a result of their function. They do COMPOSITION OF THE BLOOD ➤ Blood is a liquid that fills the vascular compartment and serves to transport dissolved materials and blood cells throughout the body. ➤ The most abundant of the blood cells, the erythrocytes or red blood cells, function in oxygen and carbon dioxide transport. ➤ The leukocytes, or white blood cells, serve various roles in immunity and inflammation. ➤ Platelets are small cell fragments that are involved in blood clotting. and are identifiable because of their cytoplasmic granules. These white blood cells are spherical and have distinctive multilobar nuclei. The granulocytes are divided into three types (neutrophils, eosinophils, and basophils) according to the staining properties of the granules. Functionally, all granulocytes are phagocytes. Neutrophils. The neutrophils, which constitute 55% to 65% of the total number of white blood cells, have granules that are neutral and hence do not stain with an acidic or a basic dye. Because these white cells have nuclei that are divided into three to five lobes, they are often called polymorphonuclear leukocytes. The neutrophils are primarily responsible for maintaining normal host defenses against invading bacteria and fungi, cell remains, and a variety of foreign substances. The cytoplasm of mature neutrophils contains fine granules. These granules contain degrading enzymes that are used in destroying foreign substances and correspond to lysosomes found in other cells (see Chapter 4). Enzymes and oxidizing agents associated with these granules are capable of degrading a variety of natural and synthetic substances, including complex polysaccharides, proteins, and lipids. These enzymes are important in maintaining normal host defenses and in mediating inflammation. The neutrophils have their origin in the myeloblasts that are found in the bone marrow (Fig. 14-3). The myeloblasts are the committed precursors of the granulocyte pathway and do not normally appear in the peripheral circulation. When they are present, it suggests a disorder of blood cell proliferation and differentiation. The myeloblasts differentiate into promyelocytes and then myelocytes. Usually, a cell is not called a myelocyte until it has at least 12 granules. The myelocytes mature to become metamyelocytes (Greek meta, “beyond”), at which point they lose their capacity for mitosis. Subsequent development of the neutrophil involves reduction in size, with transformation from an indented to an oval to a horseshoe-shaped nucleus (i.e., band cell) and then to a mature cell with a CHAPTER 14 TABLE 14-1 Plasma Water Proteins Albumin Globulins Fibrinogen Other substances 5 Plasma Components Percentage of Plasma Volume Description 90–91 6.5–8 54% Plasma proteins 38% Plasma proteins 7% Plasma proteins Hormones, enzymes, carbohydrates, fats, amino acids, gases, electrolytes, excretory products 1–2 segmented nucleus. These mature neutrophils are often referred to as segs because of their segmented nucleus. Development from stem cell to mature neutrophil takes approximately 2 weeks. It is at this point that the neutrophil enters the bloodstream. After release from the marrow, the neutrophils spend only approximately 4 to 8 hours in the circulation before moving into the tissues. Their survival in the tissues lasts approximately 4 to 5 days. They die in the tissues in discharging their phagocytic function or they die of senescence. The pool of circulating neutrophils (i.e., those that appear in the blood count) is in closely maintained equilibrium with a similar-sized pool of cells marginating along the walls of small blood vessels. These are the neutrophils that respond to chemotactic factors and migrate into the tissues toward the offending agent. Epinephrine, exercise, stress, and corticosteroid drug therapy can cause rapid increases in the circulating neutrophil count by shifting cells from the marginating to the circulating pool. Endotoxins or microbes have the opposite effect, producing a transient decrease in neutrophils by attracting neutrophils into the tissues. Eosinophils. The cytoplasmic granules of the eosinophils stain red with the acidic dye eosin. These leukocytes con- TABLE 14-2 Hematopoietic System stitute 1% to 3% of the total number of white blood cells and increase in number during allergic reactions and parasitic infections. In allergic reactions, it is thought that they release enzymes or chemical mediators that detoxify the agents associated with allergic reactions. In parasitic infections, the eosinophils use surface markers to attach themselves to the parasite and then release hydolytic enzymes that kill it. Basophils. The granules of the basophils stain blue with a basic dye. These cells constitute only approximately 0.3% to 0.5% of the white blood cells. The granules in the basophils contain heparin, an anticoagulant, and histamine, a vasodilator. The basophils share properties of mast cells and are thought to be involved in allergic and stress responses. Lymphocytes. The lymphocytes constitute 20% to 30% of the white blood cell count. They originate in the bone marrow from lymphoid stem cells. They have no identifiable granules in the cytoplasm and are also called agranulocytes. The lymphocytes play an important role in the immune response. They move between blood and lymph tissue, where they may be stored for hours or years. Their function in the lymph nodes or spleen is to defend against Blood Cell Counts Blood Cells Number of Cells/L Red blood cell count White blood cell count Differential count Granulocytes Neutrophils Segs Bands Eosinophils Basophils Lymphocytes Monocytes Platelet count 4.2–5.4 × 106, 3.6–5.0 × 106 * 4.40–11.3 × 103 150–400 × 103 *First value is for men and the second for women. Percentage of White Blood Cells 47–63 0–4 0–3 0–2 24–40 4–9 6 UNIT IV Hematopoietic Function Granules (lysosomes) Promyelocyte Myelocyte Granulocyte Myeloblast Loss of capacity for mitosis Metamyelocyte Lymphocyte Lysosome Band cell Phagocytic vacuole Segmented neutrophil Lysosome Enters blood Monocyte/Macrophage FIGURE 14-2 White blood cells. Enters tissues (1-2 days) FIGURE 14-3 Development of neutrophils. (Adapted from Cormack D. H. [1993]. Ham’s histology [9th ed.]. Philadelphia: J. B. Lippincott) microorganisms in the immune response (see Chapter 19). There are two types of lymphocytes: B lymphocytes and T lymphocytes. The B lymphocytes differentiate to form antibody-producing plasma cells and are involved in humoral-mediated immunity. The T lymphocytes activate other cells of the immune system and are involved in cell-mediated immunity. inert foreign bodies, such as talc or surgical sutures. Immune granulomas are caused by insoluble particles that are capable of inciting a cell-mediated immune response. The tubercle that forms in primary tuberculosis infections is an example of an immune granuloma (see Chapter 30). Monocytes and Macrophages. Monocytes are the largest Thrombocytes, or platelets, are circulating cell fragments of the large megakaryocytes that are derived from the myeloid stem cell. They function to form a platelet plug to control bleeding after injury to a vessel wall (see Chapter 15). Their cytoplasmic granules release mediators required for hemostasis. Thrombocytes have no nucleus, cannot replicate, and, if not used, last approximately 8 to 9 days in the circulation before they are removed by the phagocytic cells of the spleen. of the white blood cells and constitute approximately 3% to 8% of the total leukocyte count. The life span of the circulating monocyte is approximately 1 to 3 days, three to four times longer than that of the granulocytes. These cells survive for months to years in the tissues. The monocytes, which are phagocytic cells, are often referred to as macrophages when they enter the tissues. The monocytes engulf larger and greater quantities of foreign material than the neutrophils. These leukocytes play an important role in chronic inflammation and are also involved in the immune response by activating lymphocytes and by presenting antigen to T cells. When the monocyte leaves the vascular system and enters the tissues, it functions as a macrophage with specific activity. The macrophages are known as histiocytes in loose connective tissue, microglial cells in the brain, and Kupffer cells in the liver. Some macrophages function in the alveoli. Granulomatous inflammation is a distinctive pattern of chronic inflammation in which the macrophages form a capsule around insoluble materials that cannot be digested. Foreign-body granulomas are incited by relatively Thrombocytes HEMATOPOIESIS The generation of blood cells begins in the endothelial cells of the developing blood vessels during the fifth week of gestation and then continues in the liver and spleen. After birth, this function is gradually taken over by the bone marrow. The marrow is a network of connective tissue containing immature blood cells. At sites where the marrow is hematopoietically active, it produces so many erythrocytes that it is red, hence the name red bone marrow. Fat cells are also present in bone marrow, but they are in- CHAPTER 14 Hematopoietic System Blood Cell Precursors HEMATOPOIESIS ➤ Blood cells originate from pluripotent stem cells in the bone marrow. ➤ The proliferation, differentiation, and functional abilities of the various blood cells are controlled by hormone-like growth factors called cytokines. active in terms of blood cell generation. Marrow made up predominantly of fat cells is called yellow bone marrow. During active skeletal growth, red marrow is gradually replaced by yellow marrow in most of the long bones. In adults, red marrow is largely restricted to the flat bones of the pelvis, ribs, and sternum. As a person ages, the cellularity of the marrow declines. When the demand for red cell replacement increases, as in hemolytic anemia, there can be resubstitution of red marrow for yellow marrow. Some hematopoiesis may also be generated in the spleen and the liver. The blood-forming population of bone marrow is made up of three types of cells: self-renewing stem cells, differentiated progenitor (parent) cells, and functional mature blood cells. All of the blood cell precursors of the erythrocyte (i.e., red cell), myelocyte (i.e., granulocyte or monocyte), lymphocyte (i.e., T lymphocyte and B lymphocyte), and megakaryocyte (i.e., platelet) series are derived from a small population of primitive cells called the pluripotent stem cells (Fig. 14-4). Their lifelong potential for proliferation and self-renewal makes them an indispensable and lifesaving source of reserve cells for the entire hematopoietic system. Several levels of differentiation lead to the development of committed unipotential cells, which are the progenitors for each of the blood cell types. These cells are referred to as colony-forming units or burst-forming units. These progenitor cells lose their capacity for self-renewal but retain the potential to differentiate in response to lineage-specific growth factors. They develop into the precursor cells that give rise to mature erythrocytes, myelocytes, megakaryocytes, or lymphocytes. Disorders of hematopoietic stem cells include aplastic anemia and the leukemias. Today, potential cures for these (committed stem cells) Pluripotent stem cell Myeloid stem cell Lymphoid stem cell T cell progenitor B cell progenitor Megakaryocyte CFU Granulocyte CFU Monocyte CFU Erythrocyte CFU thymus Monoblast B cell (mature cells) Megakaryocyte T cell 7 Reticulocyte Plasma cell Monocyte Eosinophil Neutrophil Basophil Platelets Erythrocyte FIGURE 14-4 Major maturational stages of blood cells. CFU, colony forming units. 8 UNIT IV Hematopoietic Function and many other disorders require hematopoietic stem cell transplantation. Stem cell transplants correct bone marrow failure, immune deficiencies, hematologic defects and malignancies, and inherited errors of metabolism. Sources of the stem cells include bone marrow, peripheral blood, and umbilical cord blood, all of which replenish the recipient with a normal population of pluripotent stem cells. Bone marrow and peripheral blood transplants may be derived from the patient (autologous) or from a histocompatible donor (allogeneic). Autologous transplants are often used to replenish stem cells after high-dose chemotherapy or irradiation. Peripheral blood stem cells are harvested from the blood after the administration of a cytokine growth factor that increases the quantity and migration of the cells from the bone marrow. Umbilical cord blood from HLA-matched donors is a transplant option for children and carries less risk for graft-versus-host disease. Methods of collecting, propagating, and preserving stem cells are still being investigated. Regulation of Hematopoiesis Under normal conditions, the numbers and total mass for each type of circulating blood cell remain relatively constant. The blood cells are produced in different numbers according to needs and regulatory factors. This regulation of blood cells is thought to be at least partially controlled by hormone-like growth factors called cytokines. The cytokines are a family of glycoproteins that stimulate the proliferation, differentiation, and functional activation of the various blood cell precursors in bone marrow. Many cytokines are produced by bone marrow stromal cells that include macrophages, endothelial cells, fibroblasts, and lymphocytes and act locally in the bone marrow by binding to cell surface receptors. Other cytokines are produced in the liver and kidney. Some cytokines are colony-stimulating factors (CSFs) that were named for their ability to promote growth of blood cell colonies in culture. Major growth factors that act on committed progenitor cells include: erythropoietin (EPO), which stimulates red blood cell production; granulocyte-monocyte colony-stimulating factor (GM-CSF), which stimulates progenitors for granulocytes, monocytes, erythrocytes, and megakaryocytes; granulocyte colonystimulating factor (G-CSF), which promotes the proliferation of neutrophils; macrophage colony-stimulating factor (M-CSF), which induces macrophage colonies, and thrombopoietin (TPO), which stimulates the differentiation of platelets. The CSFs act at different points in the proliferation and differentiation pathway, and their functions overlap. Other cytokines, such as the many interleukins, the interferons, and tumor necrosis factor, support the proliferation of stem cells and the development of lymphocytes and act synergistically to aid the multiple functions of the CSFs (see Chapter 19). The genes for most hematopoietic growth factors have been cloned, and their recombinant proteins have been generated for use in a wide range of clinical problems. The clinically useful factors include EPO, TPO, G-CSF, and GMCSF. They are used to treat bone marrow failure caused by chemotherapy or aplastic anemia, the anemia of kidney failure, hematopoietic neoplasms, infectious diseases such as acquired immunodeficiency syndrome (AIDS), congenital and myeloproliferative disorders, and some solid tumors. Growth factors are used to increase peripheral stem cells for transplantation and to accelerate cell proliferation after bone marrow engraftment. Many of these uses are still investigational. In summary, blood is composed of plasma, plasma proteins, formed elements or blood cells, and substances such as hormones, enzymes, electrolytes, and byproducts of cellular waste. The blood cells consist of erythrocytes or red blood cells, leukocytes or white blood cells, and thrombocytes or platelets. Blood cells are generated from pluripotent stem cells located in the bone marrow. Blood cell production is regulated by chemical messengers called cytokines and growth factors. Diagnostic Tests After completing this section of the chapter, you should be able to meet the following objectives: ✦ Cite information gained from a complete blood count ✦ State the purpose of the erythrocyte sedimentation rate ✦ Describe the procedure used in bone marrow aspiration Blood specimens can be obtained through skin puncture (capillary blood), venipuncture, arterial puncture, or bone marrow aspiration. BLOOD COUNT Tests of the hematologic system provide information regarding the number of blood cells and their structural and functional characteristics. A complete blood count (CBC) is a commonly performed screening test that determines the number of red blood cells, white blood cells, and platelets per unit of blood. The white cell differential count is the determination of the relative proportions (percentages) of individual white cell types. Measurement of hemoglobin, hematocrit, mean corpuscular volume (MCV), mean corpuscular hemoglobin concentration (MCHC), and mean cell hemoglobin (MCH) is usually included in the CBC. Inspection of the blood smear identifies morphologic abnormalities such as a change in size, shape, or color of cells. Specific tests of red blood cell function are found in Chapter 16 and of white blood cell function in Chapter 17. ERYTHROCYTE SEDIMENTATION RATE The erythrocyte sedimentation rate (ESR) is a screening test for monitoring the fluctuations in the clinical course of a disease. In anticoagulated blood, red blood cells aggregate and sediment to the bottom of a tube. The rate of fall of the aggregates is accelerated in the presence of fib- CHAPTER 14 Hematopoietic System 9 rinogen and other plasma proteins that are often increased in inflammatory diseases. The ESR is the distance in millimeters that a red cell column travels in 1 hour. Normal values are 1 to 13 mm/hour for men and 1 to 20 mm/hour for women. REVIEW EXERCISES BONE MARROW ASPIRATION AND BIOPSY A. Explain why stem cells are used rather than mature lymphocytes. You might want to refer to Figure 14-4. Tests of bone marrow function are done on samples obtained using bone marrow aspiration or bone marrow biopsy. Bone marrow aspiration is performed with a special needle inserted into the bone marrow cavity, and a sample of marrow is withdrawn. Usually, the posterior iliac crest is used in all persons older than 12 to 18 months of age. Other sites include the anterior iliac crest, sternum, and spinous processes T10 through L4. The sternum is not commonly used in children because the cavity is too shallow and there is danger of mediastinal and cardiac perforation. Because aspiration disturbs the marrow architecture, this technique is used primarily to determine the type of cells present and their relative numbers. Stained smears of bone marrow aspirates are usually subjected to several studies: determination of the erythroid to myeloid cell count (i.e., normal ratio is 1⬊3); differential cell count, search for abnormal cells, evaluation of iron stores in reticulum cells, and special stains and immunochemical studies. Bone marrow biopsy is done with a special biopsy needle inserted into the posterior iliac crest. Biopsy removes an actual sample of bone marrow tissue and allows study of the architecture of the tissue. It is used to determine the marrow-to-fat ratio and the presence of fibrosis, plasma cells, granulomas, and cancer cells. The major hazard of these procedures is the slight risk for hemorrhage. This risk is increased in persons with a reduced platelet count. In summary, diagnostic tests of the blood include the complete blood count, which is used to describe the number and characteristics of the erythrocytes, leukocytes, and platelets. The erythrocyte sedimentation rate is used to detect inflammation. Bone marrow aspiration is used to determine the function of the bone marrow in generating blood cells. Many of the primary immunodeficiency disorders in which there is a defect in the development of immune cells of T or B lymphocyte origin can be cured with allogeneic stem cell transplantation from an unaffected donor. B. Describe how the stem cells would go about the process of repopulating the bone marrow. Bibliography Alexander W. S. (1998). Cytokines in hematopoiesis. International Reviews of Immunology 16, 651–682. Bonner H., Bagg A., Cossman J. (1999). The blood and lymphoid organs. In Rubin E., Farber J. L. (Eds.), Pathology (3rd ed., pp. 1066–1087). Philadelphia: Lippincott-Raven. Davoren J. B. (2000). Blood disorders. In McPhee S. J., Lingappa V. R., Ganong W. F., Lange J. D. (Eds.), Pathophysiology of disease (3rd ed., pp. 98–123). New York: Lange Medical Books/ McGraw-Hill. Guyton A. C., Hall J. E. (2000). Textbook of medical physiology (10th ed.). Philadelphia: W. B. Saunders. Hoffman R., Benz E. J., Shattil S. J., et al. (2000). Hematology: Basic principles and practice (3rd ed.). New York: Churchill Livingstone. Jansen J., Thompson J. M., Dugan M. J., et al. (2002). Peripheral blood progenitor cell transplantation. Therapeutic Apheresis 6(1), 5–14. Lovell-Badge R. (2001). The future for stem cell research. Nature 414(6859), 88–91. Rocha V., Wagner J. E., Sobocinski K., et al. (2000). Graft-versushost disease in children who have received a cord-blood or bone marrow transplant from an HLA-identical sibling. New England Journal of Medicine 342, 1846–1854. Rubin R. N., Leopold L. (1998). Hematologic pathophysiology. Madison, CT: Fence Creek Publishing. Stamatoyannopoulos G., Majerus P. W., Perlmutter R. M., Varmus H. (2001). The molecular basis of blood diseases (3rd ed.). Philadelphia: W. B. Saunders. Wadlow R. C., Porter D. L. (2002). Umbilical cord blood transplant: Where do we stand? Biology of Blood and Marrow Transplantation, 637–647.