* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Ibogaine in opioid detoxification
Survey
Document related concepts
Discovery and development of beta-blockers wikipedia , lookup
National Institute for Health and Care Excellence wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Theralizumab wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
Transcript
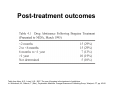
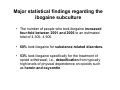
Ibogaine in opioid detoxification Kenneth Alper, M.D. Associate professor of Psychiatry and Neurology, New York University Presentation on ibogaine at Drug Policy Alliance Conference in Albuquerque, New Mexico, November 14, 2009 . Dr. Alper's presentation was one of a panel of six presentations organized and moderated by Howard Lotsof entitled "Ibogaine in Opiate Detoxification: How do we know it works? How does it work?" Clinical use of ibogaine •Given most often for opiate detoxification, and also for dependence on other drugs such as methamphetamine and cocaine. •Typically administered as a single oral dose in the range of 10 to 25 mg/kg of body weight. •Advantages attributed by those who have been treated with ibogaine are higher tolerability relative to other standard treatments for acute opioid withdrawal, and post-treatment interval of diminished drug craving that may last days to month. •Low dose protocols involving repeated administration of 10 to 50 mg/day are becoming increasingly common particularly for the treatment of stimulant dependence. Evidence for effectiveness Reporting from people who have taken ibogaine: Medical Ethnography •Consistency among reports of treatment experiences and outcomes •The strongest attribution of efficacy is for the indication of acute opioid detoxification. •Variable interval of reduced drug craving following treatment, often on the order of weeks to months •The reports of individuals who have taken ibogaine may have mechanistic significance; e.g. descriptions of panoramic memory and “oneiric” state. Published Ibogaine Case Studies • One paper describing 33 treatments for opioid dependence; complete resolution of withdrawal signs in 29 (88%)1. • Open label prospective study in St. Kitts N=32. Rating scales indicating resolution of withdrawal signs and symptoms at 24 hours, sustained improvement in depression scale scores at 1 month2. • 3 treatments, one for opioid dependence (Luciano et al. 1998) 1. Alper, KR, Lotsof, HS, Frenken, GMN, Luciano, DJ, and Bastiaans, J (1999). Treatment of Acute Opioid Withdrawal with Ibogaine. American Journal on Addictions 8: 234-242. 2. Mash DC, Kovera CA, Pablo J, Tyndale R, Ervin FR, Kamlet JD, et al. Ibogaine in the treatment of heroin withdrawal. Alkaloids Chem Biol. 2001;56:155-71. 3. Luciano, DJ. (1998). Observations on treatment with Ibogaine. American Journal on Addictions 7, 89-90. Post-treatment outcomes Table from Alper, K.R., Lotsof, H.S., 2007. The use of ibogaine in the treatment of addictions. In: Winkelman, M., Roberts, T. (Eds.), Psychedelic Medicine. Praeger/Greenwood Publishing Group, Westport, CT, pp. 43-66. June 1962, a heroin dependent lay drug experimenter serendipitously experiences the resolution of withdrawal following the use of ibogaine. The nexus of harm reduction and ibogaine Nico Adriaans (1958-1995) •Nico Adriaans was active in a network of Dutch heroin users involved in ibogaine treatment. •Adriaans founded and led the "Rotterdamse Junkiebond”, the first drug users union. •The Junkiebond greatly influenced Dutch drug policy towards adopting the harm reduction model.It initiated the first needle exchange in Rotterdam in 1981, as well as other harm reduction interventions. •Not a “hippie”, a term which denotes irresponsibility and hedonism Major statistical findings regarding the ibogaine subculture • The number of people who took ibogaine increased four-fold between 2001 and 2006 to an estimated total of 4,300- 4,900. • 68% took ibogaine for substance-related disorders. • 53% took ibogaine specifically for the treatment of opioid withdrawal; i.e., detoxification from typically high levels of physical dependence on opioids such as heroin and oxycontin Opioid dependence is the central clinical focus of the ibogaine subculture Graphic by an Amsterdam squatter for the International Coalition for Addict Self-Help, a group of Dutch Heroin users involved in ibogaine treatments. Triptych “Rise and Fall of Addiction” by Geerte Frenken Left panel from triptych “Rise and Fall of Addiction” by Geerte Frenken Ibogaine in the animal model “All models are wrong, some models are useful”- George E. P. Box Iboga Alkaloid efficacy in the animal model: morphine withdrawal • 11published independent replications in the rat, mouse and primate US patent for use of ibogaine to reduce opioid analgesic tolerance, Ciba Pharmaceutical Corp., 1957 In animals, reduced drug self-administration in following ibogaine treatment has been reported for • Morphine • Cocaine • Amphetamine • Nicotine • Alcohol How does it work? Placebo? Placebo responder ? The published literature indicates no clinically significant placebo effect in opioid detoxification. • Very few published clinical studies of opioid detoxification involving the three major treatments (methadone, buprenorphine, clonidine) even have a placebo condition. • In these few studies that did include placebo, the placebo group had significantly greater signs of withdrawal and dropped out of the study more often versus any active treatment. There is no clinically significant placebo effect in opioid detoxification. Clinical example: • Go to Newark, West Baltimore, or the Bronx. • Sell a dummy bag of baking soda and maltose. • Return to the same location the following day. • See how long you live. Is ibogaine working as an opioid agonist? Opiate receptor Cell surface Cell interior Signal transmission through the opiate receptor causes opiate effects such as euphoria or the “high” or reduction of pain Opiates, or opiate receptor agonists bind to the opiate receptor and increase signal transmission through the receptor µ $ Opiate agonist ↓ Examples of opiate agonists include: • From the opium poppy: heroin, morphine • Synthetic: methadone, oxycontin, fentanyl • Naturally occurring in the body: endorphins Opiate receptor antagonists bind to the opiate receptor and block signal transmission through the receptor Opiate antagonist X ↓ Examples of opiate antagonists include: • Naloxone (short acting) • Naltrexone (long acting) Transmission through opiate receptors is reduced in the dependent state due to the development of tolerance Normal ↓ Dependent / tolerant ↓ Ibogaine appears to reverse opiate tolerance/ dependence by normalizing transmission through opiate receptors Pretreatment Dependent / tolerant ↓ Post-treatment ↓ Evidence against ibogaine or noribogaine as an opioid substitute: • Individuals who are successfully detoxified with a single dose of ibogaine do not go back into withdrawal • Doses of ibogaine, given to non-dependent individuals, which may be higher than those used to treat opioid withdrawal, do not produce opioid overdose. (In this regard, consider that LD50 of methadone is 40 mg, whereas dosages of 80 mg/day are often used in opioid substitution maintenance) • Ibogaine and noribogaine lack some properties expected of a μ agonist, such as analgesia (but do potentiate opioid analgesics) Ibogaine might increase signal transmission through opiate receptors by an effect that is independent of substitute/agonist binding to the receptor. Pretreatment Dependent / tolerant ↓ Post-treatment ↓ This is a very important scientific possibility that could lead to fundamentally new treatment, and to a better understanding of the biological basis of addiction. WE DON’T KNOW Risks Clinical features of fatalities that have occurred within 72 hours of the ingestion of ibogaine • Significant preexisting medical, particularly cardiac disease (e.g recent MI, cardiomyopathy), with bradyarrhythmia and/or possible QTc prolongation as possible mechanisms • At least one death has involved alcohol withdrawal seizures, which are dangerous on their own, and also contribute to cardiac risk due QT prolongation. Ibogaine will not prevent seizures due to withdrawal from benzodiazepines or alcohol. • Pulmonary embolism (PE), related to risk factors such as travel, immobility within a treatment, or generally increased liability towards thromboembolic events in IVDUs • Use of opiates or stimulants during a treatment due to potentiation of toxicity • Use of indigenous forms of uncertain origin and composition such as root bark or various extracts by the inexperienced and uninformed Ibogaine and methadone in drug-related fatalities per treatment episode (TE) •Ibogaine (all known treatment episodes [TEs] 1989-2006): 11 fatalities (at least 3 in which anatomically verified, preexisting medical conditions were Identified as the cause of death by the medical examiner with no mention of ibogaine, total 8 ibogaine-related); 3,414 TEs (1 ibogaine-related death/427 TEs)1 •Methadone (Australia 2000-2003; national registration data): 282 fatalities that met author’s criteria for methadone-related death (medical examiner mentioned methadone as a cause of death or overdose during methadone treatment); 102,615 TEs (1 methadone-related death /364 TEs)2,3 •Methadone (Utah 2004; Controlled substance and medical examiner databases): 110 fatalities in which medical examiner mentioned methadone as a cause of death; 52,350 methadone prescriptions (1 methadone-related death /476 methadone prescriptions)4 1. Alper, K.R., Lotsof, H.S. and Kaplan, C.D., (2008). The ibogaine medical subculture. Journal of Ethnopharmacology 115, 9-24. 2. Gibson, A.E. and Degenhardt, L.J., (2007). Mortality related to pharmacotherapies for opioid dependence: a comparative analysis of coronial records. Drug and Alcohol Review 26, 405-410. 3. Gibson, A. and Degenhardt, L.,(2005). Mortality related to naltrexone in the treatment of opioid dependence: A comparative analysis. NDARC Technical Report No. 229. National Drug and Alcohol Research Centre, University of New South Wales, Sydney, Australia 92 pp. 4. Sims SA, Snow LA, Porucznik CA (2007): Surveillance of methadone-related adverse drug events using multiple public health data sources. Journal of Biomedical Informatics 40:382-389. The prevailing of true intention over obsession… …is both a Cardinal spiritual goal and a desired outcome of pharmacological treatment of addiction… …